The MOST IMPORTANT intervention in a patient who has suffered cardiac arrest
Timely, high-quality chest compressions
2 inch compression, 100-120 bpm, minimal interruptions
Consider ETCO2
A clinical tool used to assess risk of OSA in the outpatient setting is
STOP-BANG
Epworth Sleepiness Scale
Poor accuracy, not really used by sleep experts; NOT a substitute for polysomnography
The generally accepted EF cutoff for "heart failure with reduced ejection fraction" is
40%
41-49%, HFmrEF
The most common large-vessel vasculitis is
GCA
This serum lab can (sometimes) be helpful in making a diagnosis of hepatocellular carcinoma
AFP
Cirrhotics--Q6mo abdominal US (great data) +/- AFP
The two shockable rhythms are
Pulseless VT
VFib
Two classes of medications commonly associated with excessive sleepiness/fatigue
Antihistamines (1st >> 2nd gen)
Beta blockers
Alpha blockers
Antipsychotics
Benzodiazepines
Muscle relaxants
Opioids
SSRIs, SNRIs, TCAs
GABA analogues
When managing ADHF in a patient on home furosemide, what is the usual dose multiplier used to determine the appropriate dose of IV furosemide?
2.5x IV
On boards questions neuropathy, arthralgias, and pulmonary involvement are highly suggestive of this type of vasculitis (small/medium/large)
Small
In ETOH withdrawal patients with functional livers, these benzodiazepines can be considered for treatment of withdrawal symptoms in addition to lorazepam (name 2):
Chlordiazepoxide
Diazepam (data suggesting this may be superior to lorazepam even in setting of liver dysfunction)
Oxazepam
Name the three medications recommended for use in the ACLS algorithm:
Epinephrine
Amiodarone
Lidocaine
Some specific to reason for arrest (PE, etc.)
First-line pharmacotherapy for narcolepsy is
Modafinil
**Methylphenidate, amphetamines are second line; however, modafinil often is insufficient to control severe symptoms and has little-no effect on cataplexy
**GHB (oxybates) also second line--tends to be quite effective but frequent side effects
Name the four pillars of GDMT in HFrEF, and the two medication classes seen to have benefit in HFpEF?
Beta blocker
ACEi/ARB/ARNI
MRA * (data is not great for HFpEF)
SGLT2i *
Differentiating between GPA and eGPA can be very challenging in practice. On boards questions, which ANCA finding is associated with GPA?
c-ANCA, anti-PR3 (c is the 3rd letter in alphabet)
A common scoring system used to characterize short-term prognosis and benefit of glucocorticoid use in alcoholic hepatitis
Maddrey Discriminant Function
Simple test: PT/INR, bili
>32 is concerning, consider steroids (prednisolone), higher risk of mortality
Lille Score--usually done ~day 4, assess response to steroids, determine whether 28-day course would be beneficial
A 45M is BIBEMS for an unwitnessed arrest. After 45 minutes of in-hospital resuscitation, a pulse is recovered and the patient is transferred to the MICU.
72 hours later the patient is intermittently opening his eyes but shows no evidence of awareness, does not interact with others, is incontinent, and has no response to visual/tactile/noxious stimuli.
What is the name of this patient's post-arrest condition?
Persistent Vegetative State
Different from coma (unarousable) and brain death (unarousable + irreversible lose of cerebral/brainstem functions)
A 36F with no prior PMH presents to your clinic with complaint of unremitting fatigue, unrefreshing sleep, and difficulty concentrating over the past 8 months. A broad workup is initiated and is ultimately negative; an empiric trial of SSRI is attempted without improvement.
What are the three major criteria (per the IOM 2015 guidelines) to diagnose myalgic encephalitis/chronic fatigue syndrome?
- A substantial reduction or impairment in the ability to engage in pre-illness levels of occupational, educational, social, or personal activities that persists for more than six months and is accompanied by fatigue, is new, is not the result of ongoing excessive exertion, and is not substantially alleviated by rest
- Post-exertional malaise – Worsening of a patient's symptoms and function after exposure to physical or cognitive stressors that were normally tolerated before disease onset
- Unrefreshing sleep
What are the two most commonly used inotropes in cardiogenic shock, and what are their mechanisms of action?
Milrinone -- PDE inhibitor, inhibits degradation of cAMP
Dobutamine -- Beta 1 agonist (some beta-2, alpha-1)
A 70M with PMH HTN, HLD, and CAD presents with several weeks of progressively worsening headaches and pain with chewing. Over the past 3 days, he has noticed several episodes of blurry vision in the R side which resolve spontaneously after a few minutes.
What is the most appropriate initial treatment (dose, route) for this patient?
IVMP 500-1000mg QDay
also accept 1 mg/kg/day PO prednisone
It is NOT 40-60mg PO pred (unless this is their weight-based dosing) due to presence of threatened visual loss
A 42M with PMH severe AUD and numerous recent hospitalizations for ETOH withdrawal presents with confusion. He appears volume down and cachectic on exam, is started on D5LR pending further workup of confusion.
Several hours later patient is very agitated and more confused. Repeat labs reveal a new AGMA (compared to admission labs) with pH on VBG 7.1. Lactate, BHB are pending.
What treatment could have been initiated to prevent development of new AGMA?
Thiamine
Wernicke-Korsakoff important, but thiamine deficiency also severely impacts TCA cycle. Giving glucose without addressing thiamine deficiency will cause cells to ramp up anaerobic ATP production and can lead to clinically significant lactic acidosis (Type B)
Name 3 H's and 3 T's:
Hypovolemia
Hypoxia
Hydrogen ion (acidosis)
Hypo/hyper-kalemia
Hypothermia
Tension PTX
Tamponade, cardiac
Toxins
Thrombosis, pulmonary
Thrombosis, cardiac
The classic tetrad of symptoms in narcolepsy are
Sleepiness
Cataplexy (sudden, brief muscle weakness/paralysis usually a/w strong emotions
Hypnagogic hallucinations (GO-ing to sleep)
Sleep paralysis
Only present in ~1/3 of patients; lower threshold for inclusion in differential for younger patients
A 70F with PMH GAD, MDD, HTN, HLD, and NIDDM2 presents with several days of progressively worsening chest pain, SOB, and leg swelling in the setting of multiple recent life stressors. After TTE a diagnosis of Takutsubo's cardiomyopathy is made.
What is the timeline by which systolic function recovery is expected in stress cardiomyopathy?
1-4 weeks
Note: Risk of in-hospital major complication (intubation, death, cardiogenic shock) is 20-30% (similar to ACS). IF they make it through initial episode, odds of recovery are very good within 1 month
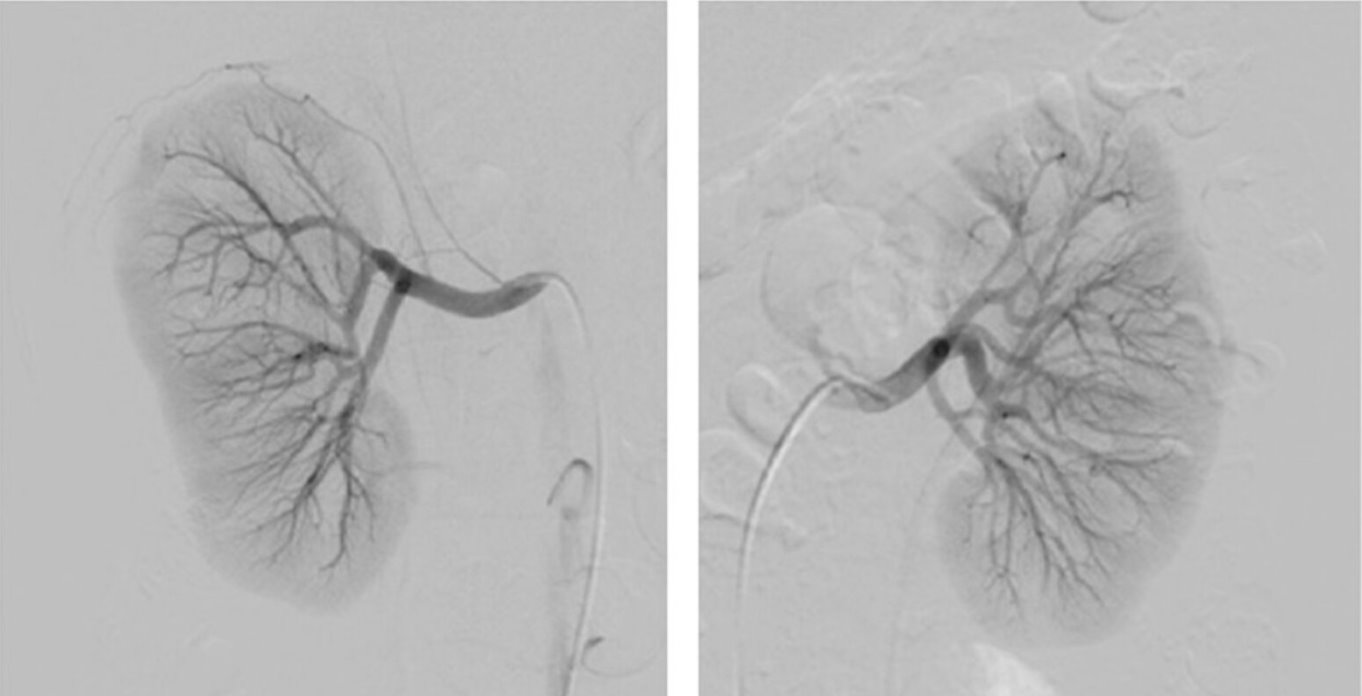
A 52M with no PMH presents with fatigue, night sweats, and bloody urine for three weeks. A broad workup is launched, demonstrates proteinuria and hematuria without infection. Complement levels are normal, cryoglobulins and ANCA are negative. Serum studies are notable for +Hep B surface antigen, Hep B quant is pending.
What is the MOST LIKELY vasculitis affecting this patient?
PAN (highly associated with Hep B, no classic lab value)
A 56M with longstanding ETOH cirrhosis c/b HE and known esophageal varices presents with bright red hematemesis and coffee-ground emesis. Which two medications must be started immediately?
Hint: NOT PPI
Octreotide -- reduce portal blood flow, decrease variceal pressure
Antimicrobial (usually CTX) -- 20% of variceal bleeds have concomitant infection, usually SBP