A 58-year-old man is evaluated for right leg tiredness and cramping when walking 25 yards. His feet are shown following elevation (top) and during dependent positioning (bottom).


Which of the following is the most likely diagnosis?
A) Inferior vena cava thrombosis
B) Livedo reticularis
C) Peripheral artery disease
D) Venous insufficiency
C) Peripheral artery disease
The most likely diagnosis is peripheral artery disease involving the right extremity. The patient has right foot pallor with elevation and dependent rubor. Previously known as the Buerger test, the patient's foot color is observed when it is elevated and again when it is dependent. The likelihood ratio of a positive finding (elevation pallor and dependent rubor) in the symptomatic extremity is 2.8 for peripheral artery disease.
A 45-year-old man is evaluated for an 18-month history of intermittent nonproductive cough and exertional dyspnea with intermittent wheezing. He is a current smoker with a 20-pack-year smoking history. He works in an auto body shop as a painter. He takes no medications.
Vital signs are normal. An occasional faint wheeze is auscultated. Chest radiograph is normal.
Which of the following is the most appropriate diagnostic test?
A) CT of the chest
B) Diffusing capacity
C) Lung volumes
D) Spirometry
D) Spirometry
This patient smokes and has an intermittent cough and dyspnea, and he likely has COPD. Dyspnea and productive cough are characteristic symptoms of COPD; however, the presentation is variable, and the cough can be nonproductive. Diagnosis requires the presence of appropriate symptoms and spirometric findings of fixed airflow obstruction. Spirometry should be performed before and after bronchodilator treatment in patients who present with progressive dyspnea, chronic cough, or chronic sputum production, particularly if a risk factor (such as smoking or occupational inhalation exposure) is present. The role of screening spirometry in asymptomatic individuals with risk factors is controversial. Spirometry measures FEV1, FVC, and the FEV1/FVC ratio to assess for and quantify airflow obstruction. The presence of persistent airflow limitation is confirmed by a postbronchodilator FEV1/FVC ratio of less than 0.70. This differs from the finding in patients with asthma, whose airflow obstruction is fully reversible with bronchodilator therapy.
Chest CT (Option A) is used to evaluate parenchymal lung lesions (such as nodules) and other potential chest pathology (such as pleural or mediastinal disease). It is not useful in diagnosing airway obstruction, particularly in this patient with a normal chest radiograph. The U.S. Preventive Services Task Force recommends annual lung cancer screening with low-dose helical CT in adults aged 50 to 80 years who have a 20-pack-year smoking history and currently smoke or have quit within the past 15 years; this 45-year-old patient does not fit these criteria.
Measuring diffusing capacity (DLCO) (Option B) or lung volumes (Option C) is not required to diagnose COPD but may help in determining the severity of disease. DLCO measurement estimates the amount of gas transfer through the alveolar/capillary unit and is proportional to the surface area of functional lung. DLCO is measured by inhalation of a gas mixture containing carbon monoxide and helium; the resulting value is corrected for lung volumes and hemoglobin level. DLCO is reduced in conditions in which functioning alveolar capillary units are destroyed (emphysema), infiltrated (interstitial lung diseases), or removed (lung resection), and in which their function is compromised (pulmonary parenchymal and vascular disorders). Conditions that increase pulmonary capillary blood volume, such as pulmonary alveolar hemorrhage, left-to-right shunt, or asthma, can cause an elevation in DLCO.
Lung volumes can be measured by body plethysmography of nitrogen diffusion. Measures include total lung capacity (TLC), vital capacity, functional residual capacity, expiratory reserve volume, and residual volume (RV). The TLC is normal or even increased in pure obstructive disease. Elevation of TLC and RV (120% of predicted or greater) can be observed in obstruction and generally indicates hyperinflation and air trapping, a common pattern in severe COPD and asthma. If FEV1 or FVC is reduced and the FEV1/FVC ratio is 0.70 or greater, the pattern may be interpreted as restrictive, but measurement of TLC is needed for confirmation. If TLC is less than 80% of predicted (or the lower limit of normal), a restrictive pattern is present.
- Spirometry should be performed before and after bronchodilator treatment in patients aged 40 years and older who present with progressive dyspnea, chronic cough, or chronic sputum production, particularly if a risk factor for COPD (such as smoking or occupational inhalation exposure) is present.
- The diagnosis of COPD is confirmed by a postbronchodilator FEV1/FVC ratio of less than 0.70.
Describe why this is done:

Dix Hallpike Maneuver
The clinician then watches the patient's eyes for torsional and up-beating nystagmus, which should start after a brief delay and persist for no more than one minute. This would indicate a positive test.
Dx: BPPV
A 72-year-old woman is evaluated in the emergency department for a 1-hour history of left-sided weakness. The patient has hypertension and dyslipidemia. She has had no recent surgery or history of gastrointestinal, genitourinary, or intracranial bleeding. Medications are amlodipine and atorvastatin.
On physical examination, blood pressure is 168/92 mm Hg; the remaining vital signs are normal. Oxygen saturation is 97% with the patient breathing ambient air. Left facial weakness, dysarthria, decreased sensation to pinprick on the left side of the body, and left arm and leg drift are noted. A bedside swallow examination is positive for dysphagia. Her score on the National Institutes of Health Stroke Scale is 6. Neurologic examination reveals a normal mental status. The remainder of the physical examination is normal.
A CT scan of the head without contrast shows no intracerebral hemorrhages or early hypodensities.
Which of the following is the most appropriate treatment?
A) Intravenous alteplase
B) Intravenous low-molecular-weight heparin
C) Intravenous nicardipine
D) Oral aspirin
A) Intravenous alteplase
She has an acute ischemic stroke and is seen within 3 hours of onset of symptoms, which include the disabling neurologic feature of hemiparesis involving the left face, left arm and leg, and left-sided sensation. Her National Institutes of Health Stroke Scale score is 6. The patient does not have any absolute or relative exclusion criteria for thrombolysis, including recent surgery, prior or current intracranial hemorrhage, extensive hypodensity on imaging, or blood pressure above the target of 185/110 mm Hg. The benefits of intravenous alteplase in acute ischemic stroke, including the lower likelihood of neurologic disability at 3 months poststroke, are generally thought to outweigh the small risk of hemorrhage.
Acute administration of anticoagulation in ischemic strokes (whether related to atrial fibrillation or not) does not reduce the short-term risk of recurrent stroke and increases the risk of hemorrhage into the territory of cerebral infarction (hemorrhagic conversion). Low-molecular-weight heparin (Option B) is not indicated.
Treatment of blood pressure with antihypertensive agents (such as nicardipine [Option C]) is not indicated in acute ischemic stroke unless the blood pressure of a patient eligible for alteplase is greater than 185/110 mm Hg (or is greater than 220/120 mm Hg for patients who are not candidates for thrombolysis). If intravenous alteplase is administered, target blood pressure is less than 180/105 mm Hg.
Aspirin (Option D) should be held for 24 hours after thrombolysis to reduce the risk of intracerebral hemorrhage. If this patient were not a candidate for thrombolysis, aspirin administered within 48 hours is indicated in order to reduce the risk of subsequent stroke but should not be administered now given the positive dysphagia screen and the need for thrombolytic therapy.
A 42-year-old woman with systemic sclerosis is evaluated for progressive dyspnea and exertional chest pain.
An apical four-chamber echocardiogram is shown.

Which of the following is the most likely diagnosis?
A) Hypertrophic cardiomyopathy
B) Pulmonary hypertension
C) Restrictive cardiomyopathy
D) Stress-induced cardiomyopathy
B) Pulmonary hypertension
The most likely diagnosis is pulmonary hypertension. The apical four-chamber echocardiogram view shows dilation of both the right atrium and right ventricle. On a normal apical four-chamber view, the right ventricle should be smaller than the left ventricle, but in this image, the right ventricle is significantly larger than the left. The right atrium also dwarfs the left atrium. Other echocardiographic findings in patients with pulmonary hypertension may include right ventricular hypokinesis, septal flattening or bowing toward the left ventricle, tricuspid regurgitation, pulmonary insufficiency, and midsystolic closure of the pulmonary valve
An 80-year-old man is evaluated for a 6-week history of resting right foot and first toe pain. He has type 2 diabetes mellitus, hypertension, and hyperlipidemia. He has a 50-pack-year smoking history but quit 10 years ago. Medications are low-dose aspirin, metformin, lisinopril, and atorvastatin.
On physical examination, vital signs are normal. The right foot is pale and mottled. A 4 × 4–cm ulceration is noted on the lateral aspect of the right fifth metatarsal. Pedal pulses are diminished on the left and absent on the right.
The ankle-brachial index is 0.62 on the left and 0.44 on the right.
Which of the following is the most appropriate next step in management?
A) CT angiography
B) Hyperbaric oxygen treatment
C) Invasive angiography
D) Primary below-the-knee amputation
C) Invasive angiography
- Chronic limb-threatening ischemia is characterized by more than 2 weeks of ischemic rest pain, nonhealing wound/ulcers, or gangrene in one or both legs that is attributable to objectively proven peripheral artery disease.
- In patients with chronic limb-threatening ischemia, immediate invasive angiography with endovascular revascularization is often the most effective strategy to preserve tissue viability.
The most appropriate next step in the management of this patient with chronic limb-threatening ischemia (CLTI), also called critical limb ischemia, is to perform invasive angiography of the affected limb (Option C) with subsequent revascularization. CLTI is characterized by more than 2 weeks of ischemic rest pain, nonhealing wound/ulcers, or gangrene in one or both legs that is attributable to objectively proven peripheral artery disease (PAD). PAD can be confirmed with ankle-brachial index testing (often <0.4 in CLTI), toe-brachial index testing, and other measures. Unlike patients with other symptoms of PAD (e.g., intermittent claudication), patients with CLTI often cannot exercise because of skin ulceration and/or ischemic rest pain. The primary goal for patients with CLTI is to revascularize the limb to reduce the incidence of major amputation, and invasive angiography expedites the diagnosis and allows for concurrent endovascular revascularization. In patients who undergo successful limb revascularization, the 1-year risk for major amputation is significantly lower than in patients who do not undergo revascularization.
Owing to the high morbidity and mortality associated with CLTI, immediate referral for invasive angiography with endovascular revascularization is often the most effective strategy to preserve tissue viability. Noninvasive imaging studies, such as CT angiography (Option A), would result in treatment time delays in this patient with CLTI and a viable limb.
Clinical trials of hyperbaric oxygen therapy (Option B) for the treatment of arterial ulcers have focused on patients without severe PAD and have not demonstrated a long-term benefit on wound healing or an improvement in amputation-free survival compared with sham treatment. Hyperbaric oxygen therapy is not a viable treatment option for this patient who needs urgent revascularization.
Primary amputation (Option D) refers to amputation without attempting to salvage the limb. In patients with CLTI and limb viability, invasive angiography and revascularization as an initial strategy is always preferred to primary major amputation of the lower extremity. Patients older than 65 years who undergo major amputation have a 1-year mortality rate of nearly 50% and a 3-year mortality rate higher than 70%.
A 61-year-old woman is evaluated in the emergency department for a COPD exacerbation characterized by increased dyspnea and increased purulent sputum production. Home medications are mometasone furoate-formoterol, tiotropium bromide, and albuterol inhalers.
On physical examination, temperature is 37.2 °C (99.0 °F), blood pressure is 135/82 mm Hg, pulse rate is 112/min, respiration rate is 21/min, and oxygen saturation is 94% breathing oxygen, 5 L/min by nasal cannula. Pulmonary examination reveals diffuse expiratory wheezing but no use of accessory muscles. The remainder of the physical examination is noncontributory.
Arterial blood gas studies:
pH 7.36
PCO2 43 mm Hg (5.7 kPa)
PO2 65 mm Hg (8.6 kPa)
Chest radiograph shows hyperinflation and flattened diaphragm but no infiltrate.
Nebulized albuterol and oral azithromycin are initiated.
Which of the following is the most appropriate additional management?
A) High-flow nasal cannula
B) Noninvasive bilevel positive airway pressure ventilation
C) Prednisone
D) Sputum culture
C) Prednisone
The goals of treatment of an acute COPD exacerbation are to relieve acute symptoms and to prevent future exacerbations. If the patient has hypoxia, supplemental oxygen should be used to maintain an oxygen saturation of 88% to 92%. Noninvasive or invasive mechanical ventilation may be necessary if ventilation or oxygenation is inadequate. Acute symptoms should be treated with short-acting β2-agonists with or without anticholinergic agents. Glucocorticoids are a mainstay of the treatment of COPD exacerbations because they can improve FEV1 and hypoxia; decrease the need for hospitalization when used early; and decrease the frequency of treatment failures, length of stay, and time to subsequent exacerbations. Short courses of lower-dose oral glucocorticoids (prednisone 40 mg/d for 5 days) have been found to be equivalent to higher doses, longer courses, and intravenous administration.
Supplemental oxygen therapy should be used for patients with acute COPD exacerbations to maintain an oxygen saturation of 88% to 92%. This patient is maintaining oxygen saturation greater than 88% while receiving oxygen through a standard nasal cannula; thus, a high-flow nasal cannula (Option A) is unnecessary.
For patients with acute hypercapnic respiratory failure with acidosis due to a COPD exacerbation, noninvasive ventilation with bilevel positive airway pressure (Option B) can improve symptoms and reduce intubation rates, length of hospital stay, and mortality. However, this patient has adequate ventilation (as evidenced by her normal pH and PCO2 levels) and does not require noninvasive ventilation.
A sputum culture (Option D) is not routinely obtained in patients with a COPD exacerbation because the results rarely affect management.
- Glucocorticoids are a mainstay of the treatment of COPD exacerbations because they can improve FEV1 and hypoxia; decrease the need for hospitalization when used early; and decrease the frequency of treatment failures, length of stay, and time to subsequent exacerbations.
- In patients with COPD exacerbation, short courses of lower-dose oral glucocorticoids (prednisone 40 mg/d for 5 days) have been found to be equivalent to higher doses, longer courses, and intravenous administration.
Describe this finding:

Brudzinski's sign
Dx: Bacterial Meningitis
Burdzinski's sign is characterized by reflexive flexion of the knees and hips following passive neck flexion. To elicit this sign, the examiner places one hand on the patient's chest and the other hand behind the patient's neck. The examiner then passively flexes the neck forward and assesses whether the knees and hips flex. Upon passive neck flexion, a positive test results when the patient flexes his knees and hips
For Brudzinski's sign, estimates are that the diagnostic sensitivity is between 2 and 43%, and the specificity for meningitis is between 80 to 100%
A 34-year-old woman is hospitalized for right-sided visual loss of 2 days' duration. She has no headache, eye pain, or neck pain. She has had two prior pregnancies without complications. She has no other symptoms and is otherwise well.
On physical examination, vital signs are normal. Right visual field deficit in both eyes is observed. Pupils are equal in size and are reactive to light; she has full eye movements.
Complete blood count, coagulation profile, and C-reactive protein level are normal.
CT scan of the head shows a left occipital infarct. Magnetic resonance angiogram of the head and neck and ECG are normal.
Which of the following is the most appropriate diagnostic test to perform next?
A) Catheter angiography
B) Lumbar puncture
C) Transesophageal echocardiography
D) Transthoracic echocardiography with agitated saline
D) Transthoracic echocardiography with agitated saline
The patient had an embolic stroke, given the location in the occipital lobe and normal findings on vascular imaging. Leading causes of stroke in young patients with no risk factors include cervicocephalic artery dissection, a hypercoagulable state, vasculitis, and embolism from a patent foramen ovale. This patient does not have a headache, and the magnetic resonance angiogram was normal, making a dissection very unlikely. Her lack of other systemic symptoms, including fevers, rash, and joint pain, makes vasculitis less likely. A primary hypercoagulable state remains possible and should be investigated, although it is less likely given her normal laboratory values and prior pregnancies without complications. TTE with agitated saline injection can reveal a right-to-left shunt, is less invasive than other cardiac imaging, and is indicated in younger patients with stroke without other risk factors. Agitated saline with a TTE is not indicated in patients older than 45 to 50 years because a patent foramen ovale is less likely to be causally related to symptoms in that age group.
A 60-year-old woman with exertional dyspnea is evaluated for pulmonary arterial hypertension. She has limited cutaneous systemic sclerosis.
Physical examination shows jugular venous distention, a prominent S2, right ventricular heave, peripheral edema, and sclerodactyly. Lungs are clear. Chest radiograph shows right ventricular (RV) enlargement. CT angiography is negative. Pulmonary function tests show a diffusing capacity of 47% of predicted and are otherwise normal. RV systolic pressure is 52 mm Hg by echocardiography.
Which of the following is the most appropriate diagnostic test to perform next?
A) Fractional exhaled nitric oxide
B) High-resolution CT of the chest
C) Right heart catheterization
D) 6-Minute walk test
C) Right heart catheterization
The most appropriate diagnostic test to perform next is right heart catheterization (Option C). Systemic sclerosis, particularly limited cutaneous systemic sclerosis, is associated with pulmonary vascular disease caused by direct proliferative effects on the vascular wall that obliterate pulmonary arterioles and capillaries. These changes result in pulmonary arterial hypertension (PAH), which eventually leads to right ventricular (RV) dysfunction, or cor pulmonale. This patient's symptoms (exertional dyspnea), physical examination findings (jugular venous distention, prominent S2, and right ventricular heave), and echocardiographic findings (RV enlargement, elevated pulmonary artery pressure) are consistent with PAH. Because echocardiography may underestimate true pulmonary artery pressures, right heart catheterization is required to confirm pulmonary hemodynamics, diagnose PAH, and determine whether there is a specific response to vasodilator infusion, which may help guide therapy.
Measurement of fractional exhaled nitric oxide (FeNO) (Option A) provides a noninvasive way to quantify eosinophilic airway inflammation and serves as a complementary tool in the diagnosis and management of lung diseases—in particular, asthma. Elevated FeNO levels correlate modestly with blood and sputum eosinophilia and can predict glucocorticoid responsiveness in patients with respiratory symptoms. More than half of patients with asthma have eosinophilic (type 2) airway inflammation, and FeNO levels may be useful in patients in whom treatment is being considered. Measurement of FeNO does not assist in the diagnosis of pulmonary arterial hypertension.
In the evaluation of suspected pulmonary hypertension, a high-resolution CT (HRCT) scan of the chest (Option B) should be obtained if there is suspicion for interstitial lung disease. However, this patient has lungs clear to auscultation, a normal chest radiograph, and except for a low diffusing capacity, normal pulmonary function tests. HRCT is not necessary in this patient.
The 6-minute walk test (Option D) provides a useful baseline before initiation of specific PAH therapy. This test or cardiopulmonary exercise testing can be performed to assess functional status and contribute to prognostic assessment. However, neither test provides the specific diagnostic information obtained by right heart catheterization and would not be the appropriate next diagnostic test.
A 74-year-old man is evaluated for a 6-month history of progressive bilateral calf pain. The discomfort is worse with walking and improves quickly with rest. Medical history is significant for hypertension and hyperlipidemia. He has a 50-pack-year history of smoking but quit 5 years ago. Medications are rosuvastatin, quinapril, and metoprolol.
On physical examination, vital signs are normal. A right femoral bruit is noted. Bilateral femoral pulses and pedal pulses are faint. Motor and sensory examinations are normal; reflexes are normal.
The ankle-brachial index is 0.92 on the right and 0.94 on the left.
Which of the following is the most appropriate test to perform next?
A) Exercise ankle-brachial index testing
B) Invasive angiography
C) Magnetic resonance angiography
D) Segmental lower extremity blood pressure testing
A) Exercise ankle-brachial index testing
- Between 19% and 31% of patients with typical claudication symptoms have a normal or borderline ankle-brachial index.
- Exercise ankle-brachial index (ABI) testing is useful to evaluate for peripheral artery disease in patients with normal ABI values (>0.90 and ≤1.40) and high pretest probability.
This patient has limb symptoms consistent with peripheral artery disease (PAD). Generally, patients with claudication have an ABI of 0.40 to 0.90, whereas patients with ischemic rest pain, ulceration, or gangrene have an ABI less than 0.40. A resting ABI greater than 1.40 indicates the presence of noncompressible, calcified arteries in the lower extremities and is considered uninterpretable. Between 19% and 31% of patients with typical claudication symptoms have a normal or borderline ABI. Because this patient with classic claudication symptoms and faint pulses has a nondiagnostic ABI, further testing is indicated. Exercise ABI testing is useful in patients with ABI values between 0.91 and 1.40 and high pretest probability of PAD. It requires ABI measurements at rest and after treadmill walking or plantar flexion exercises. A post-exercise ankle pressure drop of 30 mm Hg or more or significant decline in the ABI suggests PAD.
Invasive angiography (Option B) is often reserved for patients with an indication for revascularization, usually either intermittent claudication or chronic limb-threatening ischemia. Likewise, noninvasive anatomic imaging studies, including arterial duplex ultrasonography, CT angiography, and magnetic resonance angiography (Option C), are used to plan for endovascular or surgical revascularization. This patient with typical limb symptoms, normal resting ABI values, and no contraindication to exercise should undergo noninvasive physiologic testing, such as exercise ABI, to confirm the diagnosis of PAD before anatomic assessment is considered.
Segmental blood pressure measurements (Option D) of the lower extremities are typically performed in patients with abnormal resting ABI values to localize diseased vessels or segments. This procedure involves pulse volume recordings (measurement of the magnitude and contour of blood pulse volume in the lower extremities) and blood pressure measurements at several locations in the lower extremities. In this patient, the resting ABI was normal; thus, the indication for segmental blood pressure measurement is unclear.
A 59-year-old man is seen in a follow-up visit for a 6-month history of progressively worsening chronic cough productive of small amounts of thin clear sputum and dyspnea on exertion. He has shortness of breath when he walks quickly and when he walks uphill. He has a 45-pack-year smoking history but quit 2 years ago. He has been using albuterol as needed since his diagnosis of COPD 3 months ago, but he remains symptomatic.
On physical examination, oxygen saturation is 95% with the patient breathing ambient air. Scattered expiratory wheezing is heard. Cardiac examination is normal.
Chest radiograph from 3 months ago shows flattened diaphragm but no infiltrate.
Spirometry at the time of diagnosis showed reduced postbronchodilator FEV1/FVC ratio and FEV1 of 69% of predicted.
Which of the following is the most appropriate pharmacologic treatment?
A) Inhaled fluticasone propionate–salmeterol
B) Inhaled tiotropium bromide
C) Prednisone
D) Roflumilast
B) Inhaled tiotropium bromide
This patient's pulmonary disease is consistent with COPD. He has a chronic cough and dyspnea on exertion, a significant smoking history, a chest radiograph showing hyperinflation, and spirometry results demonstrating nonreversible obstruction. Pharmacologic therapies can be used to reduce symptoms, improve quality of life, and reduce exacerbations in patients with COPD. Regardless of COPD severity, bronchodilators are the mainstay of COPD therapy. Inhaled bronchodilators include β2-agonists and antimuscarinic agents. There are inhaled short- and long-acting forms of both types. Initial management includes short-acting bronchodilators, but a long-acting β2-agonist (LABA) or a long-acting muscarinic antagonist (LAMA), such as tiotropium bromide, should be added if symptoms are still poorly controlled. A combination LABA–LAMA can be used if patients have persistent symptoms despite monotherapy with either long-acting bronchodilator.
Inhaled glucocorticoids (Option A) can be used in combination with a bronchodilator in COPD but should not be used as monotherapy unless the patient cannot use a bronchodilator. A combination inhaled glucocorticoid–LABA could be considered if the patient's symptoms are poorly controlled with LABA or LAMA monotherapy, but that approach has not yet been tried in this patient.
Evidence-based guidelines do not endorse chronic oral glucocorticoid therapy with agents such as prednisone (Option C) because clinical trials have not shown improved outcomes with oral glucocorticoid therapy. In addition, there is ample evidence that chronic oral glucocorticoid therapy has potential for harm, including but not limited to hypertension, hyperglycemia, osteoporosis, and susceptibility to infection. Oral glucocorticoids are recommended for short-duration treatment of acute exacerbations of COPD.
Roflumilast (Option D), a selective phosphodiesterase-4 inhibitor, can reduce symptoms and exacerbations in patients with COPD who have chronic bronchitis or frequent exacerbations; thus, it is not the initial therapy of choice in this patient who lacks the sputum production of chronic bronchitis or history of frequent exacerbations.
- Regardless of COPD severity, β2-agonists and anticholinergic/antimuscarinic agents are the mainstay of therapy.
- Initial management of COPD includes short-acting bronchodilators, but a long-acting β2-agonist or long-acting muscarinic antagonist should be added if symptoms remain poorly controlled.
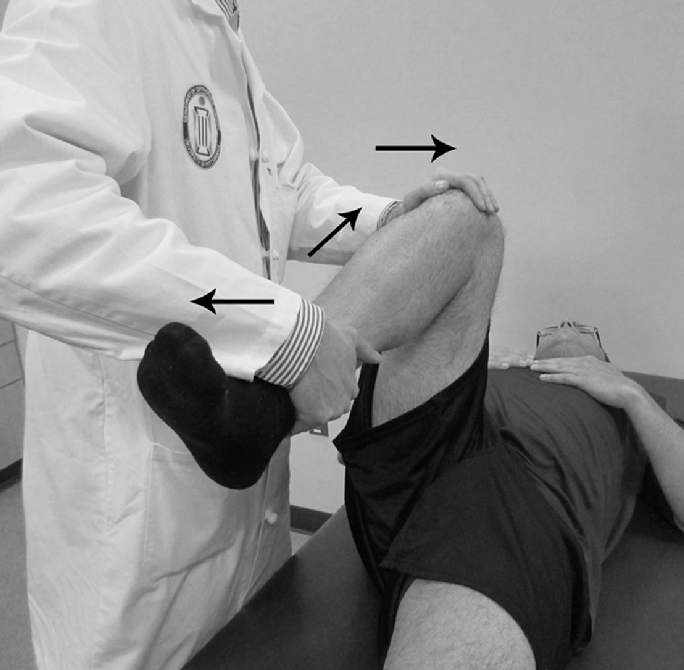
Describe this maneuver:
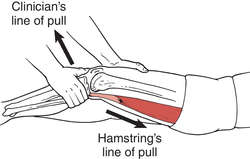
Lachman Maneuver
The Lachman test is a physical examination maneuver used to assess the integrity of the anterior cruciate ligament in a suspected anterior cruciate ligament (ACL) injury.
The patient is positioned supine with their injured knee flexed to 20 to 30 degrees while also slightly externally rotating the injured leg to relax the iliotibial band. The examiner then uses one hand to stabilize the distal femur while using the other hand to grasp the proximal tibia. Next, an anterior force is applied to the proximal tibia in an attempt to sublux the tibia forward while keeping the femur stabilized.[5]
The test is considered positive if there is excessive anterior translation of the proximal tibia greater than the uninjured side and also a lack of a firm endpoint.
Tibial translation or movement of 5 mm or more than movement in the normal limb generally indicates a rupture of the ACL, and more than 2 mm of anterior translation of the affected knee compared to the unaffected knee is considered a positive test indicating ACL injury.
Lachman's test is generally regarded as the best test for assessing ACL integrity with a sensitivity of 87% and a specificity of 93%.
A 61-year-old woman is evaluated for sudden paralysis of the right side. A CT scan without contrast taken 7 hours after symptom onset (left panel) and 24 hours after symptom onset (right panel) are shown.

Which of the following is the most likely diagnosis?
A) Herpes simplex encephalitis
B) Intracerebral hemorrhage
C) Ischemic stroke
D) Subarachnoid hemorrhage
C) Ischemic stroke
The most likely diagnosis is ischemic stroke. This patient's initial CT scan (left panel) is unremarkable, showing no evidence of hemorrhagic stroke, which would appear as a white density within the gray brain tissue, or infarction. The initial noncontrast head CT in ischemic stroke is often normal, but within 24 to 48 hours after onset of stroke symptoms, the ischemic brain tissue becomes edematous, resulting in a hypodense region on CT scan, as seen on this patient's follow-up CT scan (right panel). If the edema is significant, a mass effect may be seen with shift of midline structures (as is seen on the follow-up scan) and obliteration of the basilar cisterns. CT is insensitive for the presence of herpes simplex encephalitis, but temporal lobe hypodensities may be seen in severe cases.
A 76-year-old woman is seen for a preoperative medical evaluation before elective total ankle arthroplasty. She has heart failure with reduced ejection fraction and COPD. She has no chest pain, presyncope, or change in weight. Medications are tiotropium, budesonide, and albuterol inhalers; furosemide; metoprolol; lisinopril; and 2 L/min of oxygen via nasal cannula during exertion.
On physical examination, blood pressure is 145/80 mm Hg, pulse rate is 109/min, respiration rate is 24/min, and oxygen saturation is 90% breathing ambient air. Jugular venous pressure is elevated. There is an S4 and a grade 2/6 systolic murmur at the lower left sternal border. Breath sounds are distant without crackles.
A recent transthoracic echocardiogram showed an ejection fraction of 40%, moderate to severe right ventricle dysfunction, pulmonary artery systolic pressure of 65 mm Hg, and tricuspid regurgitation. ECG shows right bundle branch block.
Which of the following is the most appropriate preoperative management of this patient?
A) Cancel surgery
B) Increase furosemide
C) Initiate tadalafil
D) Start continuous oxygen therapy
A) Cancel surgery
The most appropriate preoperative management of this patient is to cancel surgery (Option A) and refer the patient for evaluation by a pulmonary hypertension (PH) specialist. In the perioperative period, PH, defined as pulmonary artery pressure (PAP) greater than 25 mm Hg, is associated with mortality rates of 4% to 24% and significant morbidity in up to 42% of patients. Potential complications of PH include myocardial infarction, arrhythmias, right ventricular (RV) failure, venous thromboembolism, and pulmonary failure. Patients with high-risk PH features, including group 1 PH (pulmonary arterial hypertension), PAP greater than 70 mm Hg, and moderate or severe RV dysfunction, should undergo a thorough preoperative risk assessment by a PH specialist. Surgery should generally be avoided in patients with severe PH. This patient has severe COPD and heart failure with reduced ejection fraction with evidence of PH and moderate to severe right ventricular dysfunction. She should be referred to a PH specialist for evaluation prior to the elective procedure.
Although increasing this patient's furosemide (Option B) may be indicated for heart failure and volume overload, changes to the medication regimen should be made as part of an overall treatment strategy and not as part of a preoperative evaluation. Decisions regarding medication management in the perioperative period in this patient should be made in conjunction with a PH specialist.
Most cases of PH are caused by left-sided heart disease and hypoxic respiratory disorders. Treatment is directed toward the underlying disorder. Patients with group 1 PH (which includes idiopathic and heritable pulmonary arterial hypertension, and disease related to drugs and toxins, connective tissue diseases, HIV infection, schistosomiasis, and portal hypertension) may be treated with a calcium channel blocker or vasodilator therapy, such as tadalafil (Option C) following vasoreactivity testing. Starting tadalafil is not indicated.
Chronic hypoxia with resultant pulmonary vasoconstriction may be a major contributor to a patient's PH, but further evaluation is necessary prior to instituting continuous oxygen therapy (Option D).
- Patients with high-risk pulmonary hypertension undergoing noncardiac surgery have high risk for complications, including myocardial ischemia, venous thromboembolism, cardiogenic shock, and dysrhythmias, and should be evaluated by a pulmonary hypertension specialist before undergoing surgery.
A 78-year-old man is evaluated for bilateral exertional leg pain that resolves within 2 minutes after resting. He also has hypertension, hyperlipidemia, and type 2 diabetes mellitus. Medications are metformin, atorvastatin and lisinopril.
On physical examination, vital signs are normal. Diminished distal popliteal, ankle, and pedal pulses are present. There are no bruits. Resting ankle-brachial index measurements are 1.42 in both legs.
Which of the following is the most appropriate diagnostic test?
A) Exercise ankle-brachial index
B) MR angiography of lower extremities
C) Segmental pressure measurements of lower extremities
D) Toe-brachial index
D) Toe-brachial index
- In patients with an ABI greater than 1.40, a toe-brachial index is used for diagnosis.
- Exercise ankle-brachial index testing can be useful if there is a high clinical suspicion for peripheral artery disease but normal resting ankle-brachial index measurements.
Peripheral artery disease (PAD) is typically characterized by narrowing of the aortic bifurcation and arteries of the lower extremities, including the iliac, femoral, popliteal, and tibial arteries. Atherosclerosis is the most common cause. The most commonly used diagnostic modality to identify lower extremity PAD is measurement of the resting ankle-brachial index, the ratio of lower extremity to upper extremity systolic blood pressures. In healthy persons, the ankle pressure should be the same as or slightly higher than the brachial pressure; therefore, a normal resting ABI is between 1.00 and 1.40. In the presence of atherosclerotic narrowing of the limb arteries, the downstream blood pressure and concomitant ABI value is lower. A resting ABI of 0.90 or less is diagnostic for PAD and correlates with abnormalities seen on imaging of the arterial tree. A resting ABI greater than 1.40 indicates the presence of noncompressible, calcified arteries in the lower extremities and is considered uninterpretable. This is most commonly found in patients with diabetes mellitus and/or advanced chronic kidney disease. In patients with an ABI greater than 1.40, a toe-brachial index is used for diagnosis. A toe-brachial index less than 0.70 is diagnostic for PAD.
Exercise ABI testing (Option A) can be useful if there is a high clinical suspicion for PAD but normal resting ABI test result. A decrease in the ABI to less than 0.90 or a relative decrease of greater than 20% measured immediately after symptom-limited exercise is diagnostic of PAD. This patient has an abnormally elevated ABI, and the most appropriate test is measurement of the toe-brachial index.
In patients with an established diagnosis of PAD and indications for revascularization, further vascular anatomic data can be obtained noninvasively by using gadolinium-enhanced MR angiography (Option B) or contrast-enhanced multidetector CT angiography. However, these tests should be reserved for patients who have not benefitted from medical therapy and should not be used to diagnose PAD.
Segmental pressure measurements (Option C) in a vascular laboratory may be used to localize diseased vessels in the lower extremities. The procedure involves pulse volume recordings (measurement of the magnitude and contour of blood pulse volume in the lower extremities) and blood pressure measurements at several locations in the lower extremities (high thigh, low thigh, calf, posterior tibial artery, and dorsalis pedis artery). Segmental pressure measurements can be a useful noninvasive method to localize vascular obstruction, but a toe-brachial index is the initial test of choice in this patient with high probability of disease but normal resting ABI measurements.
A 62-year-old man is evaluated in follow-up examination for COPD. Despite smoking cessation, adherence to his medical regimen, good inhaler technique, and participation in pulmonary rehabilitation, he continues to experience breathlessness with mild exertion and has diminished quality of life. He has a minimal dry cough, and he has never required treatment for an acute exacerbation of COPD. Medications are fluticasone-umeclidinium-vilanterol and albuterol inhalers as needed. Immunizations are up to date.
On physical examination, vital signs are normal. Oxygen saturation is 93% with the patient breathing ambient air. There are diminished breath sounds.
A 6-minute walk test shows a minimum oxygen saturation of 90% with the patient breathing ambient air. Spirometry shows an FEV1 of 35% of predicted and a DLCO of 42% of predicted.
Chest imaging shows upper-lobe-predominant emphysema.
Which of the following is the most appropriate treatment?
A) Long-term azithromycin therapy
B) Lung volume reduction surgery
C) Roflumilast
D) Supplemental oxygen
B) Lung volume reduction surgery ***Now Endobronchial Valves***
- Lung volume reduction surgery improves quality of life, exercise tolerance, pulmonary function, and survival in selected patients with emphysema.
- Ideal patients for lung volume reduction therapy are those with upper-lobe-predominant emphysema, FEV1 and DLCO of 20% of predicted or higher, and low exercise tolerance after completion of pulmonary rehabilitation.
The most appropriate therapy for this patient is lung volume reduction surgery (Option B). Lung volume reduction surgery improves quality of life, exercise tolerance, pulmonary function, and survival in patients with emphysema. The National Emphysema Treatment Trial also found that success relied on ideal patient selection. Ideal patients are those with upper-lobe-predominant emphysema, FEV1 and DLCO of 20% of predicted or higher, and low exercise tolerance after completion of pulmonary rehabilitation. Patients with an FEV1 of less than 20% of predicted, a DLCO of less than 20% of predicted, or non-upper-lobe-predominant disease had high mortality rates. Bronchoscopic surgery is also a possible therapeutic option. Carefully selected patients who received endobronchial valve therapy have a greater likelihood of an increase in their FEV1 of 15% or greater, significant improvements in their 6-minute walk distances, and improvements in their dyspnea.
Macrolide antibiotics such as azithromycin (Option A) have anti-inflammatory and antimicrobial effects. Long-term macrolide therapy may reduce the frequency of exacerbations when prescribed to patients with severe COPD and a history of frequent exacerbations. Chronic antibiotic therapy is not indicated for most patients with COPD, and this patient has no indication for chronic antibiotic therapy.
Roflumilast (Option C) is a selective phosphodiesterase-4 inhibitor that is used to reduce chronic symptoms and the frequency of exacerbations in patients with severe COPD who have either primarily symptoms of chronic bronchitis or frequent exacerbations. This patient with symptoms and radiographic findings most consistent with emphysema and no history of frequent exacerbations does not have an indication for roflumilast therapy.
The patient had a minimum oxygen saturation of 90% during a 6-minute walk test. Supplemental oxygen therapy (Option D) improves quality of life and decreases mortality for patients with COPD and an arterial PO2 of 55 mm Hg (7.3 kPa) or less or an oxygen saturation of 88% or less. For patients with COPD and comorbidities such as erythrocytosis, heart failure, or cor pulmonale, supplemental oxygen is reasonable if the arterial PO2 is 59 mm Hg (7.8 kPa) or less or oxygen saturation is 89% or less. This patient does not meet the criteria for supplemental oxygen.
Whats happening here?
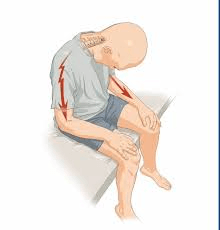
Lhermitte's Sign
Lhermitte's sign (also known as Lhermitte's phenomenon or the barber chair phenomenon) is the term used that describes a transient sensation of an electric shock that extends down the spine and extremities upon flexion and/or movement of the neck
However, the overall prevalence of Lhermitte's sign in patients with MS ranges from 9 to 41%
Despite the low sensitivity in those with MS, it has been said to have a very high specificity of 97% for compressive myelopathy as the underlying etiology.[15] One study also compared the prevalence in patients with MS and neuromyelitis optica (NMO).
A 74-year-old woman has a follow-up evaluation of left arm weakness due a right frontal cerebral infarct that occurred 2 weeks ago. She has hypertension and dyslipidemia. Current medications are aspirin, chlorthalidone, and atorvastatin.
On physical examination, vital signs are normal. Left arm shows 4/5 muscle strength throughout, with increased tone in the elbow and finger flexors. Cardiac and peripheral vascular examinations are normal.
LDL cholesterol level is 68 mg/dL (1.76 mmol/L). Serum creatinine level, basic metabolic profile, and aminotransferase levels are normal.
CT scan of the head shows a right frontal lobe infarct involving the cortical surface compatible with an embolic stroke. ECG shows sinus rhythm, left atrial enlargement, and left ventricular hypertrophy. Transthoracic echocardiogram shows an ejection fraction of 50% with no wall motion abnormalities, left atrial dilation, valvular regurgitation, or stenosis. Carotid duplex ultrasound shows less than 40% stenosis in both carotid arteries and normal flow in the vertebral arteries. Magnetic resonance angiogram of the brain shows no major arterial stenoses.
Which of the following is the most appropriate management?
A) Adding clopidogrel to aspirin
B) Changing aspirin to rivaroxaban
C) Prolonged ambulatory ECG
D) Transesophageal echocardiography
C) Prolonged ambulatory ECG
The patient had an embolic stroke of undetermined source (ESUS), based on the infarction on the cortical surface without an alternative source of emboli identified (e.g., large artery atherosclerosis or atrial fibrillation). Prolonged cardiac rhythm evaluation with ambulatory cardiac ECG or an implantable loop recorder may be positive for atrial fibrillation in approximately one third of patients with ESUS and dictate a change in therapy. The patient has several predictors of finding atrial fibrillation, including left atrial enlargement and hypertension.
Dual antiplatelet therapy (DAPT) with aspirin and clopidogrel (Option A) started 12 to 24 hours after stroke onset and continued for 21 to 90 days in patients with TIA and minor ischemic stroke results in a small but significant reduction in risk of recurrent stroke at 90 days. This patient has missed the window for DAPT and more than likely has an embolic rather than large vessel ischemic stroke; therefore, DAPT is not indicated.
Changing aspirin to rivaroxaban (Option B) is not appropriate because direct-acting anticoagulants have not been established as effective and safe therapy in patients with ESUS. In two clinical trials examining rivaroxaban or dabigatran versus aspirin in ESUS, aspirin was equivalent for stroke prevention and was associated with fewer hemorrhagic complications. Further trials are ongoing in patients with a higher suspicion for atrial fibrillation.
Transesophageal echocardiography (TEE) (Option D) can be considered in younger patients without risk factors in whom a transthoracic echocardiogram was negative for a source of emboli or in patients with a high suspicion for high-risk embolic sources, such as bacterial endocarditis or an atrial myxoma. TEE is a low-yield diagnostic test in an older patient in sinus rhythm with multiple risk factors for stroke.
A 42-year-old man is evaluated for fatigue, dyspnea, and lightheadedness. He was diagnosed with a provoked pulmonary embolism 5 months ago and has been taking apixaban since then. Initially, his dyspnea and tachycardia improved, but over the past 2 months, he has had progressive exertional dyspnea.
On physical examination, vital signs are normal. BMI is 28. Cardiopulmonary examination is normal.
An echocardiogram reveals right atrial enlargement and right ventricular hypertrophy and an elevated mean pulmonary artery pressure.
Which of the following is the most appropriate diagnostic test?
A) CT angiography of the chest
B) D-dimer assay
C) Right heart catheterization and pulmonary angiography
D) Ventilation/perfusion scan
D) Ventilation/perfusion scan
The most appropriate diagnostic test is ventilation/perfusion (V/Q) scanning (Option D) to screen for chronic thromboembolic pulmonary hypertension (CTEPH). The diagnosis of CTEPH is difficult and can be overlooked as a cause of pulmonary hypertension (PH). In patients diagnosed with PH, evaluation for CTEPH is warranted even when a history of acute pulmonary embolism is absent. The incidence of CTEPH following acute pulmonary embolism is likely less than 5%. More than 20% of patients with CTEPH do not have a previous diagnosis of pulmonary embolism. Therefore, the diagnosis of CTEPH should not automatically be excluded in patients without a history of pulmonary embolism. In patients who develop or continue to have symptoms suggesting PH after 3 months of appropriate anticoagulation for pulmonary embolism, screening for CTEPH is warranted. A normal V/Q scan is sufficient to exclude CTEPH as its sensitivity for detecting chronic thrombus approaches 100%. An abnormal V/Q requires additional investigation, typically with right heart catheterization and pulmonary angiography.
CT angiography (CTA) of the chest (Option A) is capable of detecting chronic thromboembolic material within dilated central pulmonary arteries but is less sensitive than pulmonary angiography or V/Q scanning in detecting CTEPH.
D-dimer (Option B) is useful for evaluating patients with suspected acute pulmonary embolism, but it has no utility in the evaluation of patients for CTEPH. This patient is taking apixaban and therefore is at very low risk for acute pulmonary embolism. In addition, his symptoms are progressive in nature, supporting a chronic condition over a recurrent thromboembolic event.
For patients with suspected CTEPH and an abnormal V/Q lung scan, right heart catheterization and pulmonary angiography (Option C) will confirm pulmonary hypertension, exclude competing diagnoses, and provide vital information related to potential therapy. Right heart catheterization and pulmonary angiography can be avoided in patients with a normal V/Q scan, and they should not be used as the initial tests in patients with suspected CTEPH.
A 75-year-old man is evaluated in the emergency department for a 2-day history of left leg pain. The pain started abruptly and has been constant. He has diabetes mellitus, hypertension, peripheral artery disease, and hyperlipidemia. Medications are metformin, chlorthalidone, atorvastatin, cilostazol, and low-dose aspirin.
On physical examination, pulse rate is 108/min and irregular; other vital signs are normal. Cardiac examination reveals an irregularly irregular rhythm. The left lower extremity is cold and mottled. The left popliteal and ankle pulses are absent. Passive range of motion is normal in the left leg, but the patient has significant pain and is unable to actively flex the left knee fully. Left leg sensation is intact. The remainder of the physical examination is unremarkable.
ECG shows atrial fibrillation.
Which of the following is the most appropriate next step in management?
A) Angiography
B) Apixaban
C) Intravenous tenecteplase
D) Unfractionated heparin
E) Venous duplex ultrasonography
D) Unfractionated heparin
- Classically, patients with acute limb ischemia present with at least one of the six P's: paresthesia, pain, pallor, pulselessness, poikilothermia (coolness), and paralysis.
- Patients with acute limb ischemia should receive emergent systemic anticoagulation and diagnostic angiography in preparation for revascularization.
Classically, patients with acute limb ischemia present with at least one of the six P's: paresthesia, pain, pallor, pulselessness, poikilothermia (coolness), and paralysis. Acute limb ischemia is most commonly caused by acute thrombosis of a lower extremity artery, stent, or bypass graft. Other causes include thromboembolism, vessel dissection (usually occurring periprocedurally), or trauma. This patient's presentation is consistent with acute limb ischemia due to atrial fibrillation–related thromboembolism, and the most appropriate first steps are to (1) initiate intravenous anticoagulation with unfractionated heparin, (2) perform angiography, and (3) establish a plan for reperfusion of the leg.
Invasive angiography of the lower extremity (Option A) should be expedited, as endovascular or surgical revascularization is warranted to preserve limb function and prevent major amputation. However, anticoagulation, typically with unfractionated heparin, should be initiated as soon as the diagnosis is suspected, before performing diagnostic testing.
This patient, who has atrial fibrillation, needs anticoagulation following this event. However, because intervention is needed to restore blood flow, unfractionated heparin should be initiated now, not an oral anticoagulant such as apixaban (Option B). Unfractionated heparin has a rapid onset and offset of action, allowing for more flexibility in dose titration or discontinuation when needed for invasive procedures.
Intravenous systemic thrombolysis, such as with tenecteplase (Option C), has not been proved effective in most patients with acute limb ischemia. However, catheter-based thrombolysis is effective for patients with acute limb ischemia and a salvageable limb.
Venous duplex ultrasonography (Option E) is not indicated in this patient who has no evidence of massive venous thrombosis. Iliofemoral venous thrombosis is a rare cause of acute limb ischemia and should be suspected in patients with sudden severe pain, swelling, cyanosis, and edema. These findings are not present in this patient.
A 58-year-old man hospitalized 5 days ago for a COPD exacerbation is now evaluated for discharge. He required bilevel positive airway pressure for 1 day because of acute hypercapnic and hypoxic respiratory failure. He was treated with prednisone and levofloxacin. This is his second hospitalization for a COPD exacerbation in the past 6 months and the fourth course of prednisone for his COPD in that time. Before hospitalization, his baseline function was limiting dyspnea after walking a few minutes. Medications are inhaled fluticasone furoate-umeclidinium-vilanterol.
On physical examination, oxygen saturation is 96% with the patient breathing ambient air. BMI is 29. He coughs frequently during examination, and faint expiratory wheezing is present in the upper lobes of the lungs. Cardiac examination is normal.
Arterial blood gas studies (at time of discharge):
pH 7.39
PCO2 43 mm Hg (5.7 kPa)
PO2 75 mm Hg (10.0 kPa)
Prehospitalization spirometry showed a postbronchodilator reduced FEV1/FVC ratio and an FEV1 of 42% of predicted.
Inhaler technique is reviewed. He is enrolled in a supervised pulmonary rehabilitation program. Immunizations are up to date.
Which of the following is the most appropriate additional treatment?
A) Nocturnal noninvasive bilevel positive airway pressure ventilation
B) Roflumilast
C) Supplemental oxygen
D) No additional treatment
B) Roflumilast
- Roflumilast, a selective phosphodiesterase-4 inhibitor, can reduce symptoms and exacerbations in patients with severe COPD who have a chronic bronchitis phenotype or frequent exacerbations.
This patient has COPD with Global Initiative for Chronic Obstructive Lung Disease (GOLD) class D severity based on his high symptom burden and exacerbations. He is already receiving combination inhaled therapy with a long-acting β2-agonist, long-acting muscarinic antagonist, and inhaled glucocorticoid. Roflumilast, a selective phosphodiesterase-4 inhibitor, can reduce symptoms and exacerbations in patients with severe COPD who have a chronic bronchitis phenotype or frequent exacerbations. Given this patient's clinical picture, he would likely benefit from the addition of roflumilast. Azithromycin, a macrolide antibiotic, can also be used for patients with COPD and persistent exacerbations, especially in those who are current nonsmokers. There are no head-to-head comparisons of roflumilast with azithromycin. The choice of medication is determined by the medication's side effects, drug interactions, and contraindications.
Nocturnal noninvasive ventilation with bilevel positive airway pressure (Option A) can be prescribed for patients with concomitant obstructive sleep apnea or chronic hypercapnic respiratory failure (PCO2 of 52 mm Hg [6.9 kPa] or higher). In select populations, it may improve hospital-free survival. This patient does not meet the criteria for nocturnal noninvasive ventilation.
For patients with COPD, supplemental oxygen therapy (Option C) improves quality of life and decreases mortality in patients with an arterial PO2 of 55 mm Hg (7.3 kPa) or less or an oxygen saturation as measured by pulse oximetry of 88% or less. For patients with COPD who also have cor pulmonale, heart failure, or erythrocytosis, these thresholds are lowered to a PO2 of 59 mm Hg (7.8 kPa) or less or oxygen saturation of 89% or less. However, this patient does not meet these criteria.
Because this patient will likely benefit from the addition of roflumilast, discharging him with no additions to his treatment regimen (Option D) would not be appropriate.
Name this maneuver and what it is used to diagnose:
FADIR
AKA Flexion, adduction, and internal rotation
What: Passive flexion of hip to 90 degrees with adduction and internal rotation
Dx: Anterior rim femoroacetabular impingement syndrome, labral tear and hip OA with posterior sign
A 64-year-old man is hospitalized for right-sided weakness and slurred speech of 24 hours' duration. He has hypertension and dyslipidemia. Current medications are aspirin and high-intensity atorvastatin.
On physical examination, blood pressure is 190/88 mm Hg and oxygen saturation is 98% with the patient breathing ambient air. The remaining vital signs are normal. Abnormal physical examination findings are confined to right facial weakness and right arm and leg pronator drift. National Institutes of Health Stroke Scale score is 3.
ECG is normal. Serum creatinine level is 0.9 mg/dL (79.6 µmol/L), and cardiac biomarkers are negative.
CT scan of the head shows a left frontal infarction. CT angiogram shows 80% stenosis of middle cerebral artery.
Which of the following is the most appropriate immediate treatment?
A) Chlorthalidone
B) Furosemide
C) Intracranial stenting
D) Lisinopril
E) No additional intervention or treatment
E) No additional intervention or treatment
In patients not eligible for thrombolytic therapy, the blood pressure (BP) threshold for initiating antihypertensive therapy is greater than 220/120 mm Hg; reduction of BP by 15% during the first 24 hours may then be reasonable.
A 42-year-old man with 6 months of progressive dyspnea is diagnosed with chronic thromboembolic pulmonary hypertension following right heart catheterization and pulmonary artery angiography. Medical history is otherwise unremarkable, and he takes no medications.
Apixaban is initiated.
Which of the following is the most appropriate management?
A) Add riociguat
B) Balloon pulmonary angioplasty evaluation
C) Surgical thromboendarterectomy evaluation
D) No additional treatment
C) Surgical thromboendarterectomy evaluation
The most appropriate treatment for this patient with chronic thromboembolic pulmonary hypertension (CTEPH) is referral for surgical thromboendarterectomy evaluation (Option C). CTEPH consists of organized, chronic thrombi within the pulmonary arterial system. Patients with CTEPH demonstrate both mechanical obstruction of pulmonary arteries and features of disordered pulmonary angiogenesis, fibrinolysis, and vascular remodeling. These changes manifest in increased pulmonary vascular resistance and elevated mean pulmonary artery pressure. Untreated, CTEPH can lead to right-sided heart failure and death. Lifelong anticoagulation to help prevent further thromboembolism and consideration of thromboendarterectomy are indicated for CTEPH. The only potentially curative therapy for CTEPH is pulmonary thromboendarterectomy. Because the disease is usually progressive, surgical evaluation at an experienced center is warranted in all patients with CTEPH, regardless of disease severity. Approximately half of patients with CTEPH will be eligible for surgery. Pulmonary thromboendarterectomy can result in normalization of pulmonary hemodynamics in about one third of patients who undergo surgery.
For patients who are not candidates for surgical intervention or who choose not to pursue this path, medical therapy is indicated. Currently, the only medication approved for treating CTEPH is riociguat (Option A), a stimulator of soluble guanylate cyclase, the primary receptor for nitric oxide.
Balloon pulmonary angioplasty (Option B) may be appropriate for some nonoperative patients. Balloon pulmonary angioplasty is an emerging field. A catheter-directed balloon is inserted into the pulmonary artery and inflated to improve blood flow and reduce vascular resistance within the pulmonary circulation. Neither riociguat nor balloon pulmonary angioplasty should be offered before considering surgical intervention. In patients with inoperable CTEPH and those who have persistent pulmonary hypertension following thromboendarterectomy, balloon pulmonary angioplasty or medical therapy with riociguat should be considered.
No further treatment (Option D) is inappropriate for this patient. Lifelong anticoagulant therapy is indicated in all patients to prevent further thromboembolism, but because the disease is progressive without intervention, evaluation for surgical thromboendarterectomy is important.