A 30-year-old woman is evaluated for fatigue and abdominal pain of 4 months' duration. She has lost 2.3 kg (5.1 lb) during that time. She has no other medical problems and takes no medications.
On physical examination, blood pressure is 110/72 mm Hg sitting and 90/62 mm Hg standing. Pulse rate is 70/min sitting and 88/min standing. Remaining vital signs are normal. BMI is 19. The patient has intensely tanned skin and hyperpigmented buccal mucosa and palmar creases. Visual field testing is normal.
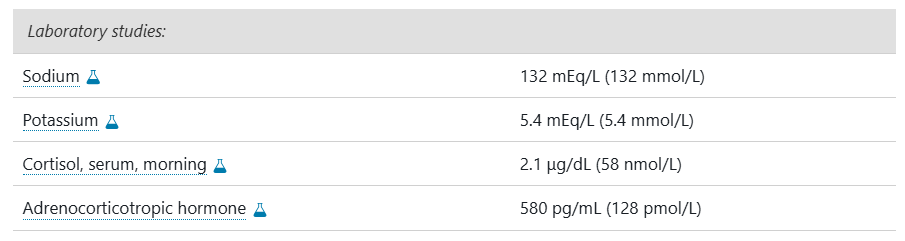
Which of the following is the most appropriate next step in management?
A. Cosyntropin stimulation test
B. Hydrocortisone plus fludrocortisone
C. Pituitary MRI
D. Prednisone
E. Serum aldosterone measurement
B
The most appropriate management is to treat with hydrocortisone twice daily and fludrocortisone once daily (Option B). This patient has primary adrenal insufficiency, as evidenced by the combination of her low morning serum cortisol and elevated adrenocorticotropic hormone level. The most common cause of primary adrenal insufficiency is autoimmune destruction of all layers of the adrenal cortex, which leads to progressive mineralocorticoid, glucocorticoid, and adrenal androgen deficiency. Most patients have positive 21-hydroxylase antibodies, and approximately 50% develop another autoimmune endocrine disorder in their lifetime, such as celiac disease, thyroid disease, or type 1 diabetes mellitus. Given that this patient has primary adrenal insufficiency, she requires both glucocorticoid and mineralocorticoid therapy. The preferred glucocorticoid for treatment of adrenal insufficiency is hydrocortisone two or three times daily to better mimic the circadian rhythm of endogenous cortisol secretion. The higher dose of hydrocortisone is given in the morning (typically 10-15 mg), and the lower dose is given in the afternoon (approximately 5 mg).
Although the cosyntropin stimulation test (Option A) is often used to diagnose adrenal insufficiency, in this patient, the diagnosis has already been confirmed by a morning serum cortisol level of less than 3 μg/dL (83 nmol/L). As a result, a cosyntropin stimulation test is not required for diagnosis and will not change management.
Given the high adrenocorticotropic hormone level, which indicates that pituitary function is intact, the etiology is confirmed to be primary and not secondary (central) adrenal insufficiency. Therefore, a pituitary MRI (Option C) is not indicated.
Adherence to multiple daily doses of hydrocortisone can be challenging. Once-daily prednisone (Option D) can be used as an alternative, but it also must be combined with fludrocortisone. Prednisone alone would not provide adequate mineralocorticoid replacement.
Serum aldosterone measurement (Option E) is not required to diagnose primary adrenal insufficiency, especially because this patient already has hyperkalemia and hyponatremia, which suggest aldosterone deficiency.
A 60-year-old woman with sepsis secondary to pyelonephritis develops acute confusion and nausea/vomiting. She has no focal deficits. Labs show: sodium 116 mEq/L, glucose 250 mg/dL, BUN 65 mg/dL, creatinine 2.1 mg/dL, ammonia 22 μmol/L (normal), normal thyroid function tests. CT head is unremarkable. EEG reveals diffuse generalized slowing. Which is the most likely cause of her encephalopathy?
A) Sepsis-associated encephalopathy
B) Hyponatremic encephalopathy
C) Uremic encephalopathy
D) Hyperglycemic hyperosmolar state encephalopathy
Correct Answer:
B) Hyponatremic encephalopathy
Explanation:
Multiple metabolic derangements can cause encephalopathy. While uremia (elevated BUN/creatinine) and hyperglycemia can contribute, severe hyponatremia (116 mEq/L) is most likely responsible here, as it causes cerebral edema and neuro symptoms. Ammonia is normal, excluding hepatic encephalopathy. SAE is a diagnosis of exclusion after ruling out metabolic causes.
Which of the following treatments for ARDS is generally thought to lack significant evidence of clinical benefit (including adult and pediatric literature)?
a) Prone positioning
b) Early neuromuscular blockade
c) iNO
d) Low tidal volume strategy
Answer: C
Prone positioning (PROSEVA), early neuromuscular blockade (ACURASYS), and low tidal volume strategy (ARDSnet NEJM 2000) have all been demonstrated (at least in some large clinical trials) to demonstrate clinical benefit in ARDS. iNO, while improving oxygenation, has not been shown to have significant clinical benefit although it is routinely used in an effort to improve oxygenation with severe ARDS and refractory hypoxemia
A 60-year-old man with fever and hypotension has blood cultures growing Escherichia coli. Imaging shows a new lung infiltrate but also hydronephrosis on renal ultrasound. Which step is most important for source control?
A) Start empiric pneumonia antibiotics and monitor
B) Urgent urology consultation for possible urinary obstruction relief
C) Bronchoscopy with lavage to identify causative organism
D) Repeat blood cultures in 48 hours
Correct Answer:
B) Urgent urology consultation for possible urinary obstruction relief
Explanation:
In E. coli bacteremia, the urinary tract is the most common source, especially with hydronephrosis indicating obstruction, which requires prompt urologic intervention for source control. Treating pneumonia alone would miss the likely source. Bronchoscopy is invasive and not first-line. Repeat cultures are important but not source control.

What is the origin of Baltimore choosing the Raven as their NFL mascot?
Answer: Edgar Allen Poe was living in Baltimore when he wrote the poem "The Raven."
A 51-year-old man is evaluated for resistant hypertension. He was first diagnosed with hypertension 10 years ago, and his blood pressure has been increasingly difficult to control. Medications are amlodipine, hydrochlorothiazide, and metoprolol.
On physical examination, his blood pressure is 164/82 mm Hg. The remainder of the examination is normal.
Laboratory testing for secondary causes of hypertension reveals primary aldosteronism.
A CT scan demonstrates a 1-cm left adrenal mass. Adrenal vein sampling does not reveal unilateral elevations in aldosterone levels.
Which of the following is the most appropriate treatment?
A. Bilateral adrenalectomy
B. Left adrenalectomy
C. Start lisinopril
D. Start spironolactone
The most appropriate treatment is to start spironolactone (Option D). Although an adrenal mass was noted on imaging, adrenal vein sampling demonstrated that this lesion is not producing aldosterone. Primary aldosteronism caused by hyperplasia of both adrenal glands (idiopathic hyperaldosteronism) is the most likely diagnosis. Idiopathic hyperaldosteronism causes approximately 60% of cases of primary aldosteronism; a unilateral aldosterone-producing adenoma (APA) is found in approximately 35% of cases. Medical therapy with an aldosterone receptor blocker, spironolactone or eplerenone, is the treatment of choice for idiopathic aldosteronism, or when patients with an aldosterone-producing adenoma are not candidates for or do not wish to undergo surgery. Spironolactone is often preferred over eplerenone because it is less expensive and has more potent aldosterone-blocking properties. However, patients on spironolactone are more likely to develop dose-dependent adverse effects, including gynecomastia and erectile dysfunction in men and menstrual irregularities in women.
Bilateral adrenalectomy (Option A) is not used in the treatment of primary aldosteronism. This procedure poses unacceptable risks to the patient, including the need for lifelong glucocorticoid and mineralocorticoid replacement, which outweigh the potential benefits. Medical therapy with aldosterone receptor blockers is first-line therapy for bilateral disease.
Adrenalectomy is effective for unilateral disease and reduces plasma aldosterone and its attendant increased risk for cardiovascular disease. This procedure is only indicated when the adrenal vein sampling lateralizes to the adrenal that is the source of excess aldosterone production. For this patient with bilateral (idiopathic) hyperaldosteronism, left adenectomy (Option B) is not indicated.
Starting lisinopril (Option C) may lead to better control of the hypertension, but it would not block the other adverse effects of hyperaldosteronism. Aldosterone has direct inflammatory and fibrotic effects that are independent of its blood pressure effects; higher cardiovascular morbidity and mortality have been noted in patients with primary aldosteronism compared with those with primary hypertension and similar blood pressure control. Therefore, treating the hypertension with lisinopril without addressing the underlying hyperaldosteronism with an aldosterone receptor blocker would subject this patient to the deleterious effects of excess stimulation of aldosterone receptors.
Which of the following molecular mechanisms is NOT typically implicated in sepsis-associated encephalopathy?
A) Microglial activation and cytokine-mediated neuroinflammation
B) Blood-brain barrier disruption leading to increased permeability
C) Direct invasion of the brain parenchyma by bacteria
D) Altered cerebral autoregulation causing ischemia-reperfusion injury
Correct Answer:
C) Direct invasion of the brain parenchyma by bacteria
Explanation:
Sepsis-associated encephalopathy is primarily caused by systemic inflammation, BBB disruption, neuroinflammation, and microvascular dysregulation but does not involve direct bacterial CNS invasion. Presence of bacteria in CNS would indicate meningitis or abscess, a different entity.
Which of the following is NOT part of the criteria for ARDS?
a) Acute onset
b) P/F ratio less than 300
c) Bilateral infiltrates on CXR
d) PCWP <10 mmHg
Answer: D
The pulmonary capillary wedge pressure is an estimate of left atrial pressure. If this value were elevated, it would suggest that cardiac dysfunction with subsequent pulmonary venous congestion could be leading to pulmonary edema and hypoxemia. While not routinely obtained in patients (typically if there is no clinical suspicion of cardiac disease, this is sufficient), if obtained, a PCWP <18 mmHg, not 10 mmHg is used for diagnosis of ARDS.
A 54-year-old man with no endocarditis or implanted devices is diagnosed with Klebsiella pneumoniae bacteremia secondary to a urinary tract infection. Blood cultures cleared within 48 hours, and he improved clinically. According to current guidelines, what is the recommended duration of antibiotic therapy?
A) 7 days
B) 10 days
C) 14 days
D) 21 days
Correct Answer:
A) 7 days
Explanation:
For uncomplicated gram-negative bacteremia with a known source and rapid clinical improvement, a 7-day course of antibiotics is sufficient according to IDSA guidelines. Longer durations (14–21 days) are reserved for complicated infections such as endocarditis, deep abscess, or implanted devices.

This is a hydrangea! This same plant can grow blue, purple, or pink flowers based on a certain growing condition. Which growing condition influences the flower color?
Answer: Soil pH
More basic soil makes the flowers grow red/pink and more acidic soil makes the flowers grow purple/blue
A 48-year-old woman is evaluated for a 6-month history of a 9.1-kg (20.1-lb) weight gain and easy bruising. She has newly diagnosed type 2 diabetes mellitus treated with metformin.
On physical examination, vital signs are normal. BMI is 38. The patient has central obesity, supraclavicular and dorsocervical fat pads, and wide violaceous striae on her abdomen.
Laboratory studies show elevated 24-hour urine free cortisol and late-night salivary cortisol levels.
Which of the following is the most appropriate diagnostic test to perform next?
A. Abdominal CT
B. Adrenocorticotropic hormone level measurement
C. 8-mg Dexamethasone suppression test
D. Inferior petrosal sinus sampling
The most appropriate diagnostic test to perform next is adrenocorticotropic hormone (ACTH) level measurement (Option B). “Cushing syndrome” is a term used to describe hypercortisolism, regardless of the cause. The initial step in evaluating suspected Cushing syndrome is to seek biochemical evidence of hypercortisolemia. At least two first-line tests must be abnormal to confirm the diagnosis. First-line tests include the overnight low-dose dexamethasone suppression test, 24-hour urine free cortisol measurement, and late-night salivary cortisol measurement. In this patient, the diagnosis of Cushing syndrome has been established given that both the urinary and late-night salivary cortisol levels are abnormal. After confirmation of Cushing syndrome, subsequent steps are to (1) determine if the Cushing syndrome is ACTH independent or dependent, and (2) localize the source of ACTH in ACTH-dependent disease or confirm the presence of adrenal mass (or masses) in ACTH-independent disease. In this patient, the next appropriate step is ACTH measurement to establish whether the patient has ACTH-dependent or -independent Cushing syndrome.
ACTH-independent Cushing syndrome is diagnosed when ACTH is suppressed (<5 pg/mL [1.1 pmol/L]). In this case, adrenal imaging with abdominal CT (Option A) or MRI is indicated. Cortisol-secreting adrenal adenomas and, rarely, carcinomas account for 15% to 20% of endogenous causes of Cushing syndrome. Excess cortisol secretion from these tumors suppresses pituitary ACTH production and is ACTH independent. Demonstration of ACTH-independent Cushing syndrome is required, however, before adrenal CT imaging is ordered, so this step is not appropriate at this time for this patient.
In patients with ACTH-dependent Cushing syndrome without a pituitary tumor visualized on MRI, an 8-mg dexamethasone suppression test (Option C) is used to help differentiate Cushing disease (pituitary Cushing syndrome) from an ectopic source of ACTH. A pituitary source of ACTH responds to negative feedback from high-dose dexamethasone, which suppresses plasma cortisol at 8 AM by more than 50%, whereas an ectopic source of ACTH does not have suppressible cortisol. This test would only be performed in ACTH-dependent disease without a visualized pituitary tumor and thus is not currently indicated in this patient.
Inferior petrosal sinus sampling (Option D) is often recommended before exploratory pituitary surgery in patients with Cushing disease. In this test, ACTH levels in the petrosal sinus are compared with those in the periphery after administration of corticotropin-releasing hormone to definitively establish the diagnosis of Cushing disease. This test is not currently indicated in this patient.
A 78-year-old man is evaluated in the emergency department for a 1-week history of fever, confusion, and altered speech. Medical history is otherwise unremarkable.
On physical examination, temperature is 39.5 °C (103.1 °F); other vital signs are normal. The patient is difficult to rouse, is disoriented, and cannot follow commands. The neurologic examination is nonfocal, and the remainder of the physical examination is normal.
Empiric intravenous vancomycin, ampicillin, ceftriaxone, and acyclovir are initiated.
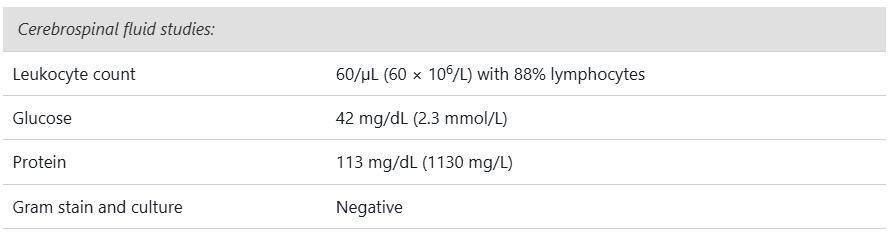
Multiplex polymerase chain reaction assay of the cerebrospinal fluid for viruses and bacteria is negative.
MRI of the brain is shown.

Which of the following is the most appropriate intravenous treatment?
A. Continue antibiotics and acyclovir
B. Continue antibiotics and discontinue acyclovir
C. Discontinue antibiotics and continue acyclovir
D. Discontinue current medications and start immune globulin and glucocorticoids
Acyclovir should be continued and antibiotics discontinued (Option C); additionally, the polymerase chain reaction (PCR) for herpes simplex virus (HSV) type 1 should be repeated in 1 week. This patient has the typical cerebrospinal fluid (CSF) findings of HSV encephalitis, including a lymphocytic pleocytosis, an elevated protein level, and a normal glucose level. This patient also has the classic imaging findings of unilateral temporal lobe enhancement. HSV PCR of the CSF confirms the diagnosis; however, false-negative results have been reported. If HSV is suspected, a repeat PCR should be obtained within 1 week while continuing acyclovir therapy.
Antibiotic treatment (Option A, B) should be discontinued because the CSF profile is not consistent with acute bacterial meningitis, and CSF Gram stain and culture and multiplex PCR for bacteria are negative. Bacterial meningitis usually presents acutely (within 1-2 days of symptom initiation) with headache, stiff neck, and altered mental status; laboratory findings include a CSF leukocyte count greater than 1000/µL (1000 × 106/L) with a neutrophilic predominance in 90% of patients, a very high CSF protein level (100-500 mg/dL [1000-5000 mg/L]), and severe hypoglycorrhachia <40 mg/dL (2.2 mmol/L). This patient's findings are not compatible with bacterial meningitis.
Starting empiric intravenous immune globulin and glucocorticoids (Option D) is appropriate for patients with a classic presentation for autoimmune encephalitis if the initial evaluation is negative for a viral cause. Repeat HSV PCR has not yet been performed for this patient, and the clinical presentation and imaging findings are not consistent with autoimmune encephalitis. The benefit of glucocorticoids in viral encephalitis has not been documented, but some experts recommend their use if significant brain edema or mass effect is present.
According to the Berlin Definition, which of the following is required for the diagnosis of moderate ARDS?
A) PaO₂/FiO₂ ratio between 200–300 with PEEP ≥5 cm H₂O
B) Bilateral infiltrates with left atrial pressure >18 mmHg
C) PaO₂/FiO₂ ratio between 100–200 with PEEP ≥5 cm H₂O
D) Acute respiratory symptoms with evidence of cardiogenic pulmonary edema
Correct Answer: C) PaO₂/FiO₂ ratio between 100–200 with PEEP ≥5 cm H₂O
Explanation:
The Berlin Definition classifies ARDS severity based on the PaO₂/FiO₂ ratio:
Mild: 200–300
Moderate: 100–200
Severe: <100
All require PEEP ≥5 cm H₂O and must have bilateral opacities not fully explained by effusions, collapse, or nodules, and respiratory failure not due to cardiac failure or fluid overload. Choice B describes older definitions (ALI criteria). Choice D is incorrect because ARDS excludes cardiogenic edema.
A patient with E. coli bacteremia from a urinary source responds well to antibiotics with defervescence. What do current guidelines recommend about repeat blood cultures in gram-negative bacteremia?
A) Repeat blood cultures are always required until negative
B) Repeat blood cultures are not routinely necessary if patient improves clinically and source is controlled
C) Repeat blood cultures should be done daily for 5 days
D) Repeat blood cultures only needed if patient is febrile after 72 hours
Correct Answer:
B) Repeat blood cultures are not routinely necessary if patient improves clinically and source is controlled
Explanation:
Current guidelines recommend that repeat blood cultures are not required in uncomplicated gram-negative bacteremia if the patient is clinically improving and source control is achieved. Repeat cultures are more important in complicated bacteremia (e.g., endocarditis, implanted devices).
In February of this year, actor Gene Hackman and his wife and classical pianist Betsy Arakawa were found dead in their Arizona home. Gene died of cardiovascular disease, but Betsy died from a complication of hantavirus called Hantavirus Pulmonary Syndrome.
How is hantavirus transmitted?
Answer: rodents, typically through exposure to mouse or rat urine, feces, and saliva. In the US it is most commonly spread by the deer mouse.
Hantavirus can cause two distinct clinical syndromes. One is the Hantavirus Pulmonary Syndrome, which is a severe flu-like illness that involves fever, chills, muscles aches, fatigue, and sometimes nausea, vomiting, and diarrhea. Later stage HPS can include dyspnea, coughing, and pleural effusions. Patients who develop respiratory symptoms have a 38% mortality rate. (https://www.cdc.gov/hantavirus/about/index.html).
Hantavirus can also trigger Hemorrhagic Fever with Renal Syndrome, a dangerous condition that can ultimately lead to organ failure, shock, and death.
A 61-year-old woman is evaluated after an abdominal CT scan for diverticulitis revealed an incidental adrenal mass. She has no other medical problems and takes no medications.
On physical examination, vital signs are normal. The remainder of the examination is unremarkable.
Abdominal CT scan shows a 3.5-cm homogeneous left adrenal mass with a density of 13 Hounsfield units. The remainder of the scan is normal.
Serum creatinine and electrolytes are normal. Testing for mild autonomous cortisol secretion is negative.
Which of the following is the most appropriate next step in management?
A. Adrenal biopsy
B. Adrenalectomy
C. Screening for primary aldosteronism
D. Screening for pheochromocytoma
D
The most appropriate next step is to screen for pheochromocytoma (Option D) with plasma free metanephrines or 24-hour urine fractionated metanephrines. The finding of an incidental adrenal mass prompts two key questions: (1) is the mass secreting excess hormone (aldosterone, cortisol, catecholamines, or androgens)?; and (2) is the mass benign or malignant? Biochemical testing for hypercortisolism should be undertaken in all patients with an incidentally discovered adrenal mass, even in the absence of typical symptoms. Screening for pheochromocytoma is indicated if the unenhanced CT attenuation is greater than 10 Hounsfield units. This asymptomatic patient with an incidentally discovered adrenal mass has no evidence of hormone excess associated with mild autonomous cortisol secretion; because the density of the mass is greater than 10 Hounsfield units, screening for pheochromocytoma is indicated.
Adrenal biopsy (Option A) has a limited role in evaluation of incidentalomas and is reserved for lesions suspicious for metastases or an infiltrative process such as lymphoma or infection. This patient has no indication for an adrenal biopsy.
Adrenalectomy (Option B) should be considered for patients with a functioning pheochromocytoma, aldosterone-producing tumor, hypercortisolism, or a suspicious imaging phenotype for adrenal carcinoma (see Figure 8). The radiologic features of this patient's mass do not suggest that adrenalectomy is needed at this time.
The patient does not require screening for primary aldosteronism (Option C) because she does not have hypertension or hypokalemia. Only patients with an incidental adrenal mass and these features require screening for primary hyperaldosteronism.
A patient with chronic liver disease presents with confusion and asterixis. Labs show elevated ammonia of 120 μmol/L and metabolic alkalosis. He is started on lactulose but mental status worsens over 48 hours. Repeat labs show WBC of 9, Hgb of 10.3, Na of 130, K of 3.2, HCO3 of 20. An ABG shows a pH of 7.30, pCO2 of 35, and a pO2 of 80. Which additional factor is most likely contributing to his worsening encephalopathy?
A) Over-sedation with benzodiazepines
B) Infection causing sepsis-associated encephalopathy
C) Hypokalemia worsening ammonia metabolism
D) Intracranial hemorrhage
Correct Answer:
C) Hypokalemia worsening ammonia metabolism
Explanation:
Hypokalemia is a common, under-recognized cause of worsening hepatic encephalopathy because it enhances renal ammonia production. Over-sedation and infection may worsen encephalopathy but hypokalemia is a correctable metabolic derangement. Intracranial hemorrhage would present with focal deficits.
A 68-year-old man with moderate ARDS (PaO₂/FiO₂ = 120) is on volume control ventilation with the following settings: TV 6 mL/kg PBW, FiO₂ 60%, PEEP 12 cm H₂O. Plateau pressure is 29 cm H₂O. Despite these settings, his PaO₂ remains 58 mmHg. Which of the following is the most appropriate next step?
A) Increase tidal volume to 8 mL/kg PBW
B) Increase FiO₂ to 80%
C) Increase PEEP to 16 cm H₂O
D) Initiate inhaled nitric oxide
Correct Answer: C) Increase PEEP to 16 cm H₂O
Explanation:
In moderate to severe ARDS, if PaO₂ remains low despite FiO₂ ≥60% and PEEP ≥10, the next step is to incrementally increase PEEP to improve alveolar recruitment, provided plateau pressure remains below 30–32 cm H₂O. Tidal volume should not be increased as it raises the risk of barotrauma. Increasing FiO₂ alone offers diminishing returns and increases oxygen toxicity. Inhaled nitric oxide may transiently improve oxygenation but has not shown mortality benefit and is not a first-line therapy.
A 74-year-old man with a history of cirrhosis (Child-Pugh B), chronic kidney disease, and atrial fibrillation on warfarin presents with fever, jaundice, hypotension, and confusion. Labs show INR 2.8, bilirubin 15 mg/dL, creatinine 3.2 mg/dL, and blood cultures positive for Klebsiella pneumoniae. Imaging confirms choledocholithiasis and biliary ductal dilation. He is started on vasopressors, broad-spectrum antibiotics, and vitamin K. What is the optimal strategy for biliary drainage in this patient?
A) Proceed with urgent ERCP after correcting coagulopathy with vitamin K and fresh frozen plasma
B) Delay ERCP until INR normalizes and renal function improves
C) Initiate percutaneous transhepatic biliary drainage immediately given high procedural risk
D) Continue antibiotics and supportive care, postponing drainage until hemodynamics stabilize
C) Initiate percutaneous transhepatic biliary drainage immediately given high procedural risk
Explanation:
In severe cholangitis complicated by multiorgan failure and coagulopathy, invasive procedures like ERCP carry high bleeding risk. Although correcting INR is ideal, urgent drainage is critical to source control and may be best achieved by percutaneous transhepatic biliary drainage (PTBD), which can be performed under local anesthesia and is safer in coagulopathic patients. Delaying drainage worsens outcomes. Vitamin K and plasma may not rapidly correct INR enough for safe ERCP.

This is a famous sled dog named Balto, who led a sled dog team in the final leg of a 600-mile journey during a blizzard to deliver the treatment for a serious illness to an isolated town. What was the medicine Balto delivered?
Answer: Diphtheria antitoxin
In 1925 there was a diphtheria epidemic and the town of Nome, Alaska, was stranded hundreds of miles away from the nearest supply of diphtheria antitoxin due to a blizzard. The only way to reach the town was by sled dog, leading to what would later be known as "The Great Race of Mercy," a quest to deliver the antitoxin. The musher was a man named Gunnar Kaasen and the final leg of the journey was 55 miles in -40 degree weather.
A 55-year-old man is evaluated 6 weeks after undergoing right adrenalectomy for a 4-cm pheochromocytoma. Before surgery, he had palpitations, sweating, and suboptimal blood pressure control despite 4 antihypertensive agents. His plasma free metanephrine levels were significantly elevated. He has recovered from surgery and currently feels well. He has no family history of hypertension or endocrinopathy. Medical history is otherwise unremarkable, and his only medication is lisinopril.
On physical examination, blood pressure is 133/79 mm Hg, and pulse rate is 90/min. Other vital signs and physical examination findings are normal.
His plasma free metanephrine levels are within the normal range.
Which of the following is the most appropriate next step in management?
A. Iodine 123–metaiodobenzylguanidine scan
B. Medical genetics counseling
C. Serum calcitonin measurement
D. 24-Hour urine fractionated metanephrine and catecholamine measurement
This patient with pheochromocytoma should be offered medical genetics counseling (Option B). Pheochromocytomas are catecholamine-secreting tumors that arise from the chromaffin cells of the adrenal medulla. Pheochromocytoma may be associated with hereditary syndromes, including multiple endocrine neoplasia type 2 (MEN2), von Hippel-Lindau syndrome, and neurofibromatosis 1. Approximately 30% of nonsyndromic apparent sporadic pheochromocytomas are associated with a genetic mutation. Diagnosis of pheochromocytoma at a later age or the absence of a family history does not rule out the possibility of an association with a genetic mutation. Therefore, genetic counseling should be offered to all patients, such as this one, who present with pheochromocytoma.
Routine screening with iodine 123–metaiodobenzylguanidine (MIBG) scanning for potential metastatic disease is not clinically indicated in patients who have unilateral pheochromocytoma, most (90%) of which are benign (Option A). MIBG or fluorodeoxyglucose-PET imaging may be considered in patients who have a large pheochromocytoma (>10 cm) or an established hereditary disorder associated with pheochromocytoma or paraganglioma. This patient has a 4-cm unilateral pheochromocytoma without an established hereditary disorder and does not currently require MIBG scanning.
While pheochromocytoma may be associated with MEN2 (and hence medullary thyroid carcinoma), serum calcitonin measurement is not recommended as a screening test in patients without a history of thyroid nodules (Option C). Evaluation for possible MEN2 should be considered in patients with bilateral pheochromocytoma and/or a palpable thyroid mass.
Patients with pheochromocytoma should undergo postoperative and long-term annual biochemical screening as recurrence can arise many years after surgery. Plasma free metanephrine levels have a sensitivity of 96% to 100% and a specificity of 85% to 89% and are more convenient to measure compared to a 24-hour urine collection. This patient has a known pheochromocytoma with elevated preoperative plasma free metanephrines that are now within the normal range. Therefore, additional measurement of 24-hour urine fractionated metanephrine and catecholamine levels is not required (Option D).
A 29-year-old woman is evaluated in the emergency department for loss of consciousness. This morning her mother found her unconscious in bed, drooling, and shaking all her limbs. The patient was unresponsive for 3 to 4 minutes, and was confused for about 5 minutes after regaining consciousness. By the time she reached the emergency department, she had recovered completely. She has had no recent illness, including infection, head trauma, or history of prior similar episodes.
She has no history of alcohol or illicit drug use. She has no other medical problems and her only medication is a combined oral contraceptive.
On physical examination, vital signs are normal. All other examination findings, including those from a neurologic examination, are unremarkable.
Results of a comprehensive metabolic profile and toxicology screen are normal. A CT of the head without contrast in the emergency department is normal. An electroencephalogram has been scheduled.
Which of the following is the most appropriate management?
A. Brain MRI without contrast
B. CT of the head with contrast
C. Levetiracetam
D. Lumbar puncture
The most appropriate management for this patient is a brain MRI without contrast (Option A). For any patient with a first seizure, obtaining a detailed history is crucial to distinguish seizures from other causes of symptoms. Making the distinction between seizure and nonseizure events and first-time versus recurrent episodes is key in selecting the proper management. The patient likely had a first (new-onset) seizure, and neuroimaging is indicated for all adult patients with a first-time seizure. CT of the head is adequate initially to rapidly exclude emergent pathology, including hemorrhage, but MRI is required and preferred in most patients. Because temporal lobe epilepsy is common, MRI sequences focusing on the hippocampus and temporal lobes are useful. Outpatient electroencephalography (EEG) also is recommended in patients with a first seizure (and has already been scheduled in this case). A single routine EEG is only 40% to 50% sensitive in the diagnosis of seizure, but the yield can increase to 80% to 90% with repeated studies, prolonged studies, and studies that capture sleep.
Following a first seizure, contrast-enhanced CT (Option B) or MRI may be deferred unless infection, tumor, or vascular lesions are suspected. These imaging procedures are not indicated in this patient.
Levetiracetam (Option C) would be indicated for this patient if epilepsy was suspected (i.e., if the seizure recurrence risk was determined to be at least 60%). Determining seizure recurrence risk for this patient would first require brain MRI and EEG to detect the presence of any significant abnormality that would support a diagnosis of epilepsy.
Unlike in children, a seizure in adults is not enough of an indication for lumbar puncture (Option D). Other signs of meningitis, such as neck stiffness, fever, altered mental status, or headache, are indications for lumbar puncture; this patient does not have these signs.
A 68-year-old male with ARDS has the following ABG on volume control ventilation (TV 6 mL/kg PBW, PEEP 16 cm H₂O, FiO₂ 70%, RR 28): pH 7.30, PaCO₂ 55 mmHg, PaO₂ 62 mmHg, HCO₃⁻ 25 mEq/L. Plateau pressure is 33 cm H₂O. What is the most appropriate ventilator adjustment?
A) Decrease tidal volume to 4 mL/kg PBW to reduce plateau pressure
B) Reduce respiratory rate to 20 breaths per minute to lower plateau pressure
C) Decrease tidal volume to 5 mL/kg PBW and maintain PEEP
D) Increase sedation and initiate paralysis
Correct Answer: C) Decrease tidal volume to 5 mL/kg PBW and maintain PEEP
Explanation:
Plateau pressure >30 cm H₂O is elevated, indicating increased risk for barotrauma. Reducing tidal volume helps lower plateau pressures, even if it increases PaCO₂ (permissive hypercapnia is acceptable if pH >7.20). Reducing respiratory rate may worsen hypercapnia. Decreasing tidal volume to 4 mL/kg may cause severe acidosis, so a modest reduction is preferred. Increasing sedation and paralysis is not primarily for ventilator adjustment but may be used adjunctively.
A patient with prosthetic valve endocarditis caused by Pseudomonas aeruginosa is receiving cefepime and tobramycin. The ID consultant suggests adding rifampin. What is the rationale, and what is a major consideration before adding rifampin?
A) Rifampin enhances biofilm penetration; consider drug interactions with other antibiotics
B) Rifampin shortens therapy duration; major side effect is nephrotoxicity
C) Rifampin is bacteriostatic; must be given as monotherapy to avoid resistance
D) Rifampin treats concomitant fungal infections; risk of hepatotoxicity is negligible
Correct Answer:
A) Rifampin enhances biofilm penetration; consider drug interactions with other antibiotics
Explanation:
Rifampin is added in prosthetic valve endocarditis to target biofilm-associated bacteria. However, it has significant drug-drug interactions (inducing metabolism of many drugs), and careful monitoring is required. Rifampin is bactericidal but should never be given as monotherapy due to rapid resistance development. It does not treat fungal infections.
Insulin was discovered in 1921 and successfully isolated from a dog pancreas.
The first purified sample of insulin used to treat a patient with diabetes was extracted in 1922 from a different animal source. What animal was the source of the treatment insulin?
Answer: cattle
A surgeon named Frederick Banting and his collaborators won the Nobel Prize in Medicine in 1923 for the discovery and implementation of insulin as a life-saving medication for patients with diabetes.