Protection of vital organs
Framework to support body structures, mobility
Movement; produce heat and maintain body temperature
Facilitate return of blood to the heart
Reservoir for immature blood cells
Reservoir for vital minerals
What is the Function of the musculoskeletal system
Function in bone formation
what are osteoblasts
Found in the upper and lower extremities. They are shaped like rods or shafts with rounded ends
what are long bones
The junction of two or more bones
what is joint/articulation
hold the bones together and joints allow the body to move.
what are muscles and tendons
Rare bone disorder associated with vitamin D deficiency, resulting in decalcification and softening of bone
What is osteomalacia?
health history and physical examination that evaluates the effects of the musculoskeletal disorder on the patient.
What does the nursing assessment of a patient with MSK dysfunction include
determine bone density, texture, erosion, and changes in bone relationships
what are bone x-rays
A chronic autoimmune disease characterized by the inflammation of the synovial joints.
What is rheumatoid arthritis?
600 IU
what is young adults daily intake of vitamin D
hematoma formation
What happens during stage I of bone healing?
Irregular shaped bones located in the ankle and hand
what are short bones
synarthrosis
amphiarthrosis
diathrosis
what are the Three basic kinds of joints
attached by tendons to bones, connective tissue, other muscles, soft tissue, or skin.
what are muscles
difficult to walk, rise from a chair, low back pain, progressive muscle weakness, weight loss , deformity of spine (kyphosis), fracture with delayed healing
What are S/S of osteomalacia?
During the interview and physical assessment, the patient may report pain, tenderness and altered sensations.
what are common syx associated with MSK dysfunction
performed to determine the structure and composition of bone marrow, bone, muscle, or synovium to help diagnose specific diseases. It involves excising a sample of tissue that can be analyzed microscopically to determine cell morphology and tissue abnormalities.
What is a biopsy
An autoimmune disease in which the normal immune response is directed against an individual's own tissue, including the synovial joints, tendons, and bones, resulting in inflammation and destruction of these tissues.
What is a rheumatoid arthritis?
98%
What percent of the body's calcium is in the bones
remodeling
osteoclasts remove necrotic bone
What happens during stage IV of bone healing?
Located where extensive protection of underlying structures is needed
what are flat bones
fibrous joints, immovable joints, fibrous tissue banding (skull sutures)
what are synarthrosis joints
limp and without tone (most often seen in lower motor neuron disorders such as muscular dystrophy)
what is flaccid muscle
Diet – Vit D, calcium and phosphorous rich
Vit.D3 (cholecalciferol), vit.D2 (ergocalciferol)
Calcium salts and phosphorous supplements may also be prescribed
What is the management of Osteomalacia ?
Pain, tenderness, altered sensation
Posture and gait
Bone integrity
Joint function
Muscle strength and size
Skin
Neurovascular status
what is Important to assess during an MSK physical assessment
determine any abnormality of function and to differentiate muscle and nerve problems. can be used to identify the extent of damage if nerve function does not return within 4 months of an injury. Needle electrodes are inserted into selected muscles, and responses to electrical stimuli are recorded on an oscilloscope.
What is electromyography
(inflammatory granular tissues) forms at junctions of synovial tissues and articular cartilage, it interfere with nutrition transport
What is PANNUS?
800-1000IU
what is adults 50+ daily intake of vitamin D
1-2 days after fracture
When does stage I of bone healing occur
Includes bones such as the vertebrae and bones of the jaw
what are irregular bones
cartilaginous joints, allow limited movement, vertebral joints and symphysis pubis).
what are amphiarthrosis joints
produced by the maintenance of some of the muscle fibers in a contracted state.
what is muscle tone
Idiopathic skeletal bone disorder in which there is excessive bone resorption followed by replacement of altered bone tissue.The new bone is larger, disorganized and structurally weaker.Common sites – pelvis , long bones, spine, ribs, sternum and cranium
What is Paget's Disease ?
ADLs
IADLs
Ability to perform various activities
Note any problems related to mobility
Family history
General health maintenance; occupation
Learning needs; socioeconomic factors
Medications (include over-the-counter)
what are Important social information to collect during MSK history
with or without the use of oral or intravenous (IV) contrast agents, shows a more detailed cross-sectional image of the body.
used to visualize and assess tumors; injury to the soft tissue, ligaments, or tendons; and severe trauma to the chest, abdomen, pelvis, head, or spinal cord.
It is also used to identify the location and extent of fractures in areas that are difficult to evaluate (e.g., acetabulum) and not visible on x-ray
What is a computed tomography
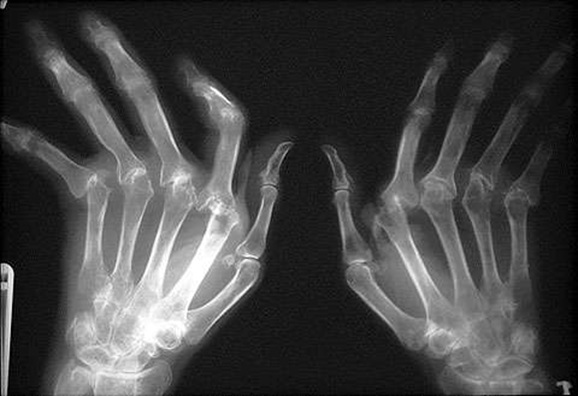
What is X ray of RA?
located in the shaft of long bones and in flat bones.
what is vascular tissue
fibrocartilaginous callus formation
fibroblasts and osteoblasts migrate to fracture site
What happens during stage II of bone healing?
an increased forward curvature of the thoracic spine that causes a bowing or rounding of the back, leading to a hunchback or slouching posture. Can occur at any age and may be caused by degenerative diseases of the spine.
what is kyphosis
synovial joints, freely movable
what are diarthrosis joints
greater-than-normal tone (most often seen in upper motor neuron disorders such as cerebral palsy)
what is spastic muscle
Increase bone volume in the spine can cause spinal cord or cranial root compression leads to head ache, blindness, vertigo, hearing loss with tinnitus and dementia
What are complication of Paget's disease?
Assess by having patient walk away from examiner for short distance. Observe for smoothness and rhythm. If any limping, note which side is favored.
How to assess gait
noninvasive imaging technique that uses magnetic fields and radio waves to create high-resolution pictures of bones and soft tissues.
It can be used to visualize and assess torn muscles, ligaments, and cartilage; herniated discs; and a variety of hip or pelvic conditions.
What is magnetic resonance imaging?
Morning stiffness lasting over 1 hour for at least 6 weeks duration. Symmetric soft tissue swelling. Elevated ESR, C- reactive protein.
What are diagnostic criteria for RA?
Calcitriol, PTH, Calcitonin, Thyroid hormones, cortisol, growth hormone, testosterone and estrogen.
What are important hormones for bone formation and maintenance
Mature bone cells that function in bone maintenance.
what are osteocytes
an exaggerated curvature of the lumbar spine. Often seen in pregnancy
what is lordosis/swayback
Felt around or in joint and typically worsens with movement
How will a patient with joint pain describe their pain?
Results when the cross-sectional area of the muscle increases
what is hypertrophy
N-telopeptide and C-telopeptide they are biomarkers used to measure the rate of bone turnover, can be measure from urine or serum
What are diagnosis investigation of Paget's disease ?
Assess for deformities and alignment. Compare symmetric parts of the body. Shortened extremities, amputations and body parts that are not in anatomic alignment are noted.
How to assess bone integrity
used to identify the cause of any unexplained joint pain and progression of joint disease by using radiopaque contract injected into the joint cavity to visualize its structures- uses serial xray method
what is arthrography
a degenerative joint disease characterized by destruction of the articular cartilage, inflammation of joints and overgrowth of bone
What is osteoarthritis?
located in the sternum, ilium, vertebrae and ribs in adults and is responsible for red blood cells, white blood cells and platelet production.
what is red bone marrow
Multinuclear cells that function in dissolving and resorbing bone
what are osteoclasts
a lateral curving deviation of the spine. Causes are congenital, idiopathic or d/t damage of the paraspinal muscles as in muscular dystrophy
what is scoliosis
shortening of surrounding joint structure
what is a contracture
Decrease in size of muscle d/t disuse
what is atrophy
Calcitonin – decrease osteoclastic activity . First Line is an oral Alendronate. Supplementation with Calcium. When not tolerated, IV pamidronate or zoledronic acid
What is Management of Paget's disease?
may include abnormal angulation of long bones, motion at joints other than joints and crepitus (a grating or crackling sound or sensation) at the point of abnormal motion
what would describe a fracture finding
performed through the use of x-rays or ultrasound, measures bone mass density, predicts fracture risks
What is bone densitometry
Affects the articular cartilage and leads to chondrocyte response , subchondral bone (bony plate that supports the articular cartilage) and synovium
What is osteoarthritis?
sensations of burning, tingling or numbness.
May be caused by pressure on nerves or by circulatory impairment
what is Paresthesia's
bony callus formation
ossification begins during 3rd or 4th week
What happens during stage III of bone healing?
Bone pain: dull, deep ache that is "boring" in nature. This pain is not typically related to movement and may interfere with sleep.
How will a patient with bone pain describe their pain?
partial separation of articular surfaces
what is subluxation
Smooth/Visceral-(Involuntary and NON-striated)
Skeletal-(Voluntary and striated)
Cardiac-(Involuntary and striated)
what are the 3 types of muscles?
A severe pyogenic infection and inflammation of bone and surrounding tissues
What is Osteomylitis?
assess nerves and function, evaluate sensation and the evaluation of motion. Make sure no signs of symptoms of compartment syndrome
how to perform a neurovascular assessment?
performed to detect metastatic and primary bone tumors, osteomyelitis, some fractures, and aseptic necrosis, and to monitor the progression of degenerative bone diseases.
what is a bone scan
Hard bony enlargements on distal interphalangeal joints
What are Heberden's nodes?
Sac filled with synovial fluid, cushions the movement of tendons, ligaments and bones over bones or other joint structures. Can be found in the elbow, shoulder, hip and knee
what is a bursa sac
dynamic tissue in a constant state of turnover.
what is bone
exists in areas where support is needed, and cancellous bone is found where hematopoiesis and bone formation occur.
what is cortical bone
excessive fluid within the capsule
what is effusion
"soreness or aching and is referred to as "muscle cramps."
How will a patient with muscle pain describe their pain?
Bone infection persists for longer than 4 weeks and also failed to respond to the initial treatment
What is chronic osteomyelitis?
Evaluated by noting range of motion, deformity, stability, tenderness, and nodular formation
how to perform a joint assessment
allows direct visualization of a joint through the use of a fiberoptic endoscope. Thus, it is a useful adjunct to diagnosing joint disorders. Biopsy and treatment of tears, defects, and disease processes may be performed through the arthroscope-procedure takes place in the operating room under sterile conditions with either injection of a local anesthetic agent into the joint or general anesthesia
What is arthroscopy
Hard bony enlargements on proximal interphalangeal joints
What are Bouchard's nodes ?
in which joint disorders would nodules possibly be present
what are rheumatoid arthritis, gout or osteoarthritis
Ossification matrix is formed and bound to collagen
what is osteogenesis (bone formation)
nurtures and facilitates longitudinal growth
what is the epiphyseal plate
complete separation of joint surfaces
what is dislocation
The body is able to perform a wide variety of movements as a result of the coordination
Isolated encapsulated pockets of microorganisms surrounded by bone matrix –capable of reinfection at any time
What are Brodie's Abscesses?
The normal curvature of the spine is convex through the thoracic portion and concave through the cervical and lumbar portions.
what is Normal physical assessment of posture
carried out to obtain synovial fluid for purposes of examination or to relieve pain due to effusion. Examination of synovial fluid is helpful in the diagnosis of septic arthritis and other inflammatory arthropathies and reveals the presence of hemarthrosis
what is arthrocentesis
Injection into the joint (intra articular injection) with gel like substance (hyaluronates) – have properties of synovial fluid.
What is viscosupplementation?