The date of PIVC insertion needs to be documented in the flowsheets, but where else does the date need to be written?
The sticker on the PIVC itself!
PIVC's can stay in for 3 days if inserted in hospital, however if inserted in the community they can only remain in for 24 hours. This helps the ward staff to know when to remove them to prevent infections and emboli.
How many seconds must you count a paediatric respiratory rate for?
60!
Paeds require a full minute to assess an accurate respiration count as their rate can vary significantly across this time.
GCS & 4AT scores are tools primarily assessing higher cognitive function.
True or False?
GCS is NOT a measure of Cognition. GCS is a scale which provides a quick bedside glance of just how far you are away from a coma, (15 = Very. 3 = Not.)
Bonus points if they can tell us about the boxing matches in Glasgow!
4AT scales on the other hand are attention / distraction questions to establish a delirium baseline. They are designed to alert you to new-onset delirium.
Higher cognitive function tests are tests like the MiniMental & MoCA!
(This question courtesy of SPOC nurse Eirona)
What does "GRN" stand for?
As in "Hey, the GRN is beeping."
GRN stands for GOVERNMENT RADIO NOTIFICATION!
Night shift afficionado Sandy Huddleston is famous for bringing what sweet treat on nightshifts?
A cracking Vanilla Slice!
Per policy, inserting a PIVC requires an order in Sunrise/EMR. True/False?
Technically true!
Per SALHN policy & protocol PIVC insertion should actually be an ORDER which we can sign-off as being done in the worklist manager.
(This never happens in practice if we're honest)
Ventolin (Salbutamol) relieves wheeze by what pathophysiological process?
(Looking for the clinical name/process specifically)
Bronchodilation!
Salbutamol is a B2 agonist, which causes bronchodilation (the opening of airways)
NIPP and NI medication cannot be given to patients over 65 - True or False?
FALSE - The policy has precautions not exclusions. Doses of medication and contraindications may change, however they are not complete exclusions!
(This question courtesy of SPOC nurse Eirona)
You are the TA. A concerned relative states that his mum is in the car on the ramp, and needs your help to get her out. There is a wheelchair nearby.
How should you retrieve this patient?
You should ALWAYS leave triage with a buddy! Never attend the ramp by yourself.
If you're leaving triage (or the hospital for that matter) to go outside, always tell someone first.
Kidnappings and other nasty situations are rare, but they do happen! Plus you may also injure yourself, or the relative attempting to extricate the patient from the car if both people are not trained in manual handling.
In this instance using a Manning board / car slide board with a buddy is your best bet for safe extrication.
Former Medical Lead Consultant Andrew Blythe hails from which country?
South Africa
A casual pool RN who completed her grad program in ED and has been in ED for a total of 9 months but has nursed for 5 years total is caring for a patient in the RAC. She notices they are dehydrated, with no signs of heart failure and haven't previously received fluids. She cannulates the patient and commences a 500ml NaCl 0.9% bag over one hour as per the Standing Medication Order.
What's wrong with the above scenario?
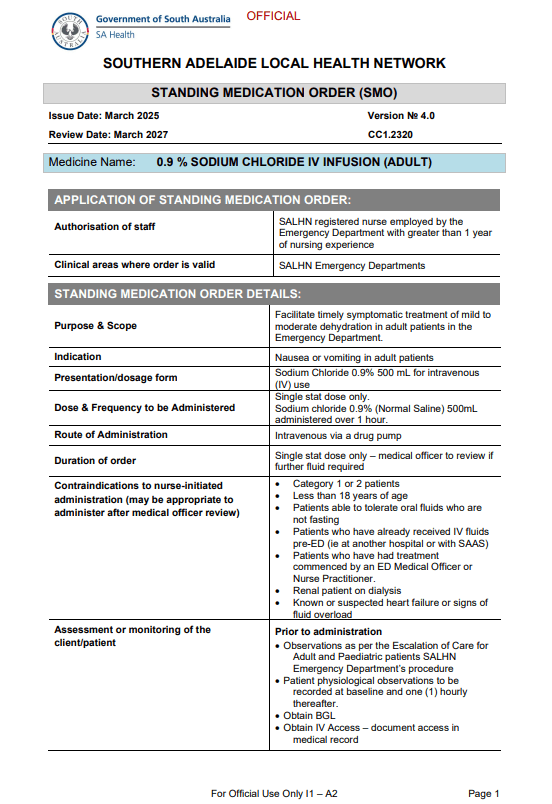
Per policy, she can't use the Standing Medication Order. She's not employed by the Emergency Department, she's employed by the casual pool.
The same restriction applies for new grads once they've finished their training until they hit their 1 year of experience. It's a grey area if you were an EN with more than a year of experience and are now a TPPP as an RN employed by the ED.
When a patient in respiratory distress begins grunting, they are attempting to naturally generate what phenomenon in their lungs?
PEEP! (Positive-End Expiratory-Pressure)
If your patient is trying to make or improve their own PEEP, this is a very late sign of significant respiratory deterioration.
It implies whatever is going on is a very significant respiratory failure.
!!!!SURPRISE GROUP ANSWER ROUND!!!!
Each group can make x1 guess on the below question. Many answers *are* correct, and are worth 300 points, however there is a SECRET answer worth 600 POINTS!
Name an overlooked, but common sign indicating increasing frailty & difficulty with ADL's in the geriatric population which you might find when assessing "E" (Exposure) in a primary survey.
Inability to look after one's own feet - If you can't reach your own feet, or see your own feet, what else are you not managing, or NOT seeing?
Elderly patients which present with dirty, poorly managed or injured feet at baseline should raise red flags for any discharge considerations.
(This question courtesy of SPOC nurse Eirona)
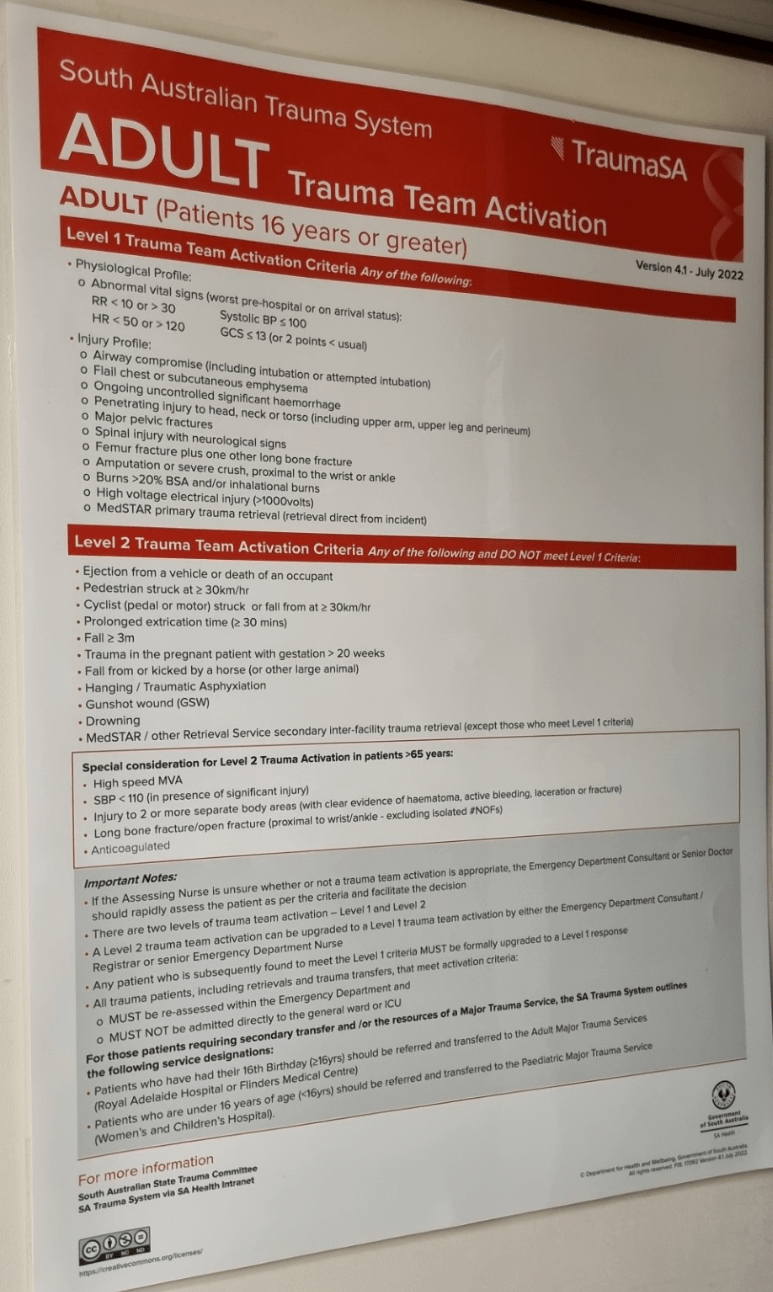
You receive a GRN for a patient.
SAAS is 5 minutes away with a 27 YO male MVA. Driver, travelling at 120km/hr, lost control of vehicle, slid to a stop against a barrier. Nil cabin intrusion, self-extricated, obs WNL on scene with SAAS.
Should this patient have a trauma call activated per criteria? Why/Why not?
Per criteria, no. Speed alone with no other injury or trauma profiles is NOT an indication for a trauma call activation.
HOWEVER - in the older cohort (65 Years +) high-speed MVA is a *special consideration*
WHO'S THAT ED NURSE?
Which ED nurse scored a deal as a promoter for a brand of fun scrubs in 2025?
It's Bailey!
Which of the following is *not* a requirement for sterility when assessing a sealed sterile item like a syringe or needle?
A) Within Expiry Date
B) Pack is intact and visibly clean e.g no holes or tears, no water marks, no dust
C) Equipment is functional and not defective
D) No additional writing on the pack
The answer is...
C - Equipment is functional and not defective
Whether the equipment is functional or not is irrelevant to it's sterility. While you would still dispose of the item, sterility requirements are the following
Within expiry date, an intact pack, and with no additional writing
A pneumonia is an example of what kind of Ventilation/Perfusion (VQ) Mismatch?
 If there's something wrong with the inside of the alveoli - it's a SHUNT
If there's something wrong with the inside of the alveoli - it's a SHUNT
If there's something wrong with the vessels, it's DEADSPACE
What are the 5 Limbic Considerations for Fragile Brains?
1.Food and Fluids
2.Sleep/ Wake Cycle
3. Elimination
4. Discomfort
5. Pain.
The limbic system manages all of the above, and also manages the "fight or flight" response. We can't always expect to win with fragile brains, however by making sure we make efforts to address all five points, we should have an easier shift!
(This question courtesy of SPOC nurse Eirona)
A 77 YO female presents to triage.
She describes a 2 day hx of 3/10 "cramping" lower abdominal pain which she's still experiencing. No change in bowels from normal, no fevers. Observations are within normal range. Despite age fit healthy & no relevant pmhx.
Per ATS, what's the triage, and what stream is she going to?
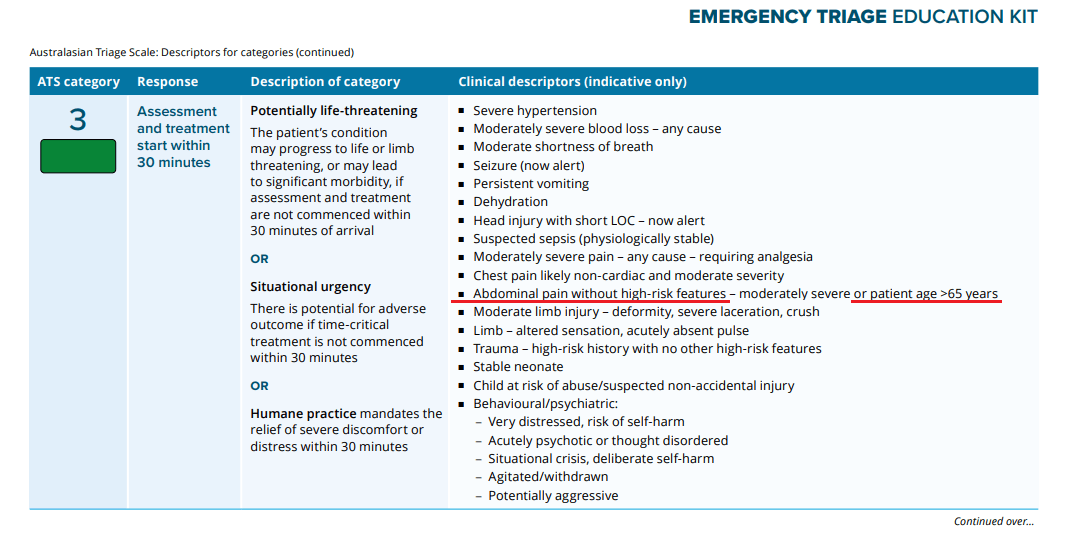
Remember the ETEK is a guide and your triage is your triage. However per the ETEK, this patient is a Priority 3! Due to age, she'll be for the Acute stream.
ED Nurse Alex has been involved as a franchisee for which famous fast food chain?
Domino's Pizza
A patient presents to ED with their own Diazepam, Oxycodone & Tapentadol DDA's which need to be locked away. This question has multiple parts.
1. Describe the checking & sealing process
2. State which DDA count book(s) the medication(s) are recorded in
3. How many pages will these medications take up inside of the book(s)?
1. Medications need to be completely visualised, counted, and confirmed with an appropriate witness. (At least one RN) then placed in a sealed tamper-evident bag where they can be viewed without opening.
2. These would be stored in the PATIENT'S OWN book
3. THREE DRUGS, THREE PAGES. It seems wasteful, but per policy, one drug, one page. It doesn't matter if it's the same patient or not.
You have a patient on 75% FiO2 via NRB.
You perform an ABG, and find their PaO2 is 250.
Is this a problem? If so, why or why not?
Yes, their PaO2 should be 375! They're headed for T1RF.
To convert FiO2 to PaO2, times by 500.
Expected PaO2 should be FiO2 (As a fraction, so in this case 75% = 0.75 x 500 = 375) So we expect a PaO2 of ~375
If you had less than 375, you're headed towards T1RF, as we're giving LOADS of extra O2 and we're still not meeting what we should be getting, which means the patient is using more than we're giving!
When drawing blood in geriatric populations, it is better to swap a certain colour tube for another, as it allows for geriatric-specific add-ons by the hometeams RCOT/OPAL
What colour tube are we replacing, and why? For what tests?
Replace your green tube with a gold tube. The vast majority of tests specific to a green top can be run in a gold, which allows the add-ons the below tests with the same blood volume.
B12, Folate & Thyroid battery tests (TFT, TSH, PTH) These tests are relevant to geriatric workup from everything to anaemia to dementia & constipation
(This question courtesy of SPOC nurse Eirona)
You are the triage assist nurse. The triage nurse asks you to check on a Priority 3 patient in the WR & report the obs back to them.
You perform the Obs and find them ALL wildly out of range in the purple zone (CRT) with an elevated RR, HR & lowered sats & BP.
PER POLICY - What is the appropriate response for this patient? For bonus points, what would *YOU* do as the TA in this scenario?
Per policy, if there is no immediate threat to life that warrants an emergency bell, the correct course of action is to speak with the triage nurse and have the patient uptriaged appropriately.
Per reality, the answer depends. Let's briefly discuss.
Which ED Registrar once worked as a Safari Ranger in Africa before settling down to a nice relaxing career of Emergency Medicine?
Liesel Drake!
A patient diagnosed with pulmonary tuberculosis was sent to North 12. They are admitted to 6A and transferred through the hospital.
What precautions should they have been on, what PPE should staff entering wear, and are there any special considerations for cleaning the room afterwards?
1. Airborne - Latent TB isn't particularly transmissible, but Pulmonary TB is!
2. PPE should be gowns, gloves, *N95* masks Eyewear +/- A Face shield.
3. Yes! If they weren't in a negative pressure room, the room should be left vacant for 2 hours.
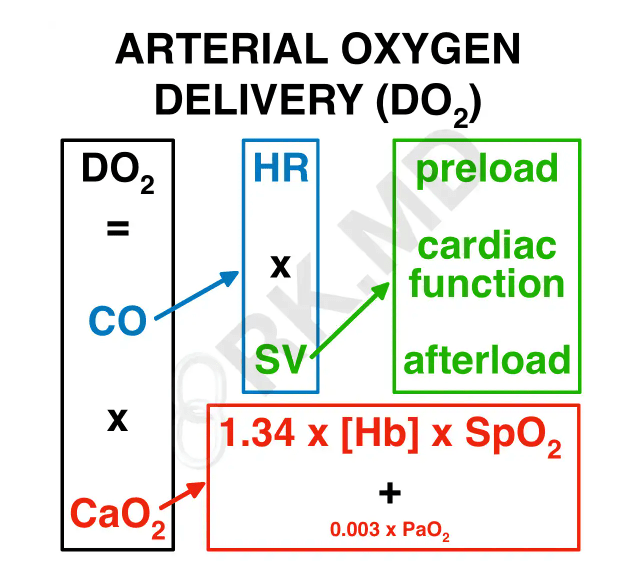 Cardiac Output (HR x SV [Preload, Contractility, Afterload) x Arterial Oxygen Content (1.34 [carrying capacity of haemoglobin] x HB x SpO2 + 0.003 x PaO2)
Cardiac Output (HR x SV [Preload, Contractility, Afterload) x Arterial Oxygen Content (1.34 [carrying capacity of haemoglobin] x HB x SpO2 + 0.003 x PaO2)
What this is basically a measure of how much blood is the heart pumping out every minute, combined with how much oxygen are all the haemoglobin carrying (SpO2), + all the oxygen dissolved in plasma. (PaO2)
Worldwide data shows that Trauma Calls in the Elderly are complicated and either over called or not called at all, however regardless of call - post fall there are three areas of patient management which we are lacking in the ED. What are they?
1.C-Spine precautions at less than 30 degrees - this is OLD data. You will occlude airways and cause choking if you lie older necks flat. (think kids resus, not tilting heads back).
2. Poor retention/urinary management. Those people who understand that they are in c-spine precautions will stay in them and often go into retention, please document pt output, also remember that C-spine precautions end above the "bra strap" digging in heels and lifting bottoms for slipper pans is OK. (Give pain relief first)
3. Pressure areas - because it takes too long for non trauma falls to be seen (not judgement, just fact) the chance of pressure area injury is high.
This does not mean a nimbus, it just means that if they can be reminded to lift arms and bend knees, flex feet up and down, wriggle toes and be assisted to move off of boney prominences we negate further harm.
If they cannot move independently, use log rolls as per normal, or you can escalate to the radiology department - let them know that they have been in C-spine for XX hours and are at increasing risk of pressure injuries / retention / airway compromise after consultation with the Senior MO.
(This question courtesy of SPOC nurse Eirona)
**SURPRISE LIGHTNING ROUND**
WHAT'S THAT QUESTION????
I say the ANSWER - you guess the QUESTION.
Every correct answer is worth 200 points! Wrong answers have NO penalty. Five seconds to answer.
10mls of Saline (A flush/normal flush volume)
Paracetamol, Endone, Ibuprofen, Ondansetron, 500mls of Saline. (Nurse initiated medications)
3 rounds of 6 puffs 20 minutes apart (Rescues)
10mg & 2mg (Doses for Olanzapine + Lorazepam for agitation)
Pink Blood Top. (What's the colour for a crossmatch)
After touching a patient's surroundings. (Moment 5 of Hand Hygiene)
33# (Emergency phone number)
#89 (pager system contact number
Code Purple (Colour-Code for a bomb threat.)
Nine questions - 1800 points! Let's tally them up!
Spell This ED Consultant's last name.
Joel P _ _ _ _ _ _ _ _
(Hint, it's Polish)
Przybylko