What are some biological factors that contribute to mental illness?
There are many biological and neurophysiological processes that are hypothesized or known to be involved in or associated with psychopathology.
Some examples:
- Neuronal structure and function
- Brain structure and function
- Genetic/epigenetic influences
- Nervous system structure and function
What is the definition of a mental disorder?
A mental disorder is a syndrome characterized by clinically significant disturbance in an individual’s cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning. Mental disorders are usually associated with significant distress or disability in social, occupational, or other important activities.
What are some of the criteria for Persistent Depressive Disorder?
A. Depressed mood for most of the day, for more days than not, as indicated by either subjective account or observation by others, for at least 2 years.
Note: In children and adolescents, mood can be irritable and duration must be at least 1 year.
B. Presence, while depressed, of two (or more) of the following:
1. Poor appetite or overeating.
2. Insomnia or hypersomnia.
3. Low energy or fatigue.
4. Low self-esteem.
5. Poor concentration or difficulty making decisions.
6. Feelings of hopelessness.
C. During the 2-year period (1 year for children or adolescents) of the disturbance, the individual has never been without the symptoms in Criteria A and B for more than 2 months at a time.
D. Criteria for a major depressive disorder may be continuously present for 2 years.
E. There has never been a manic episode or a hypomanic episode and criteria have never been met for cyclothymic disorder.
F. The disturbance is not better explained by a persistent schizoaffective disorder, schizophrenia, delusional disorder, or other specified or unspecified schizophrenia spectrum and other psychotic disorder.
G. The symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition (e.g., hypothyroidism).
H. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
What is differential diagnosis?
A differential diagnosis means that there is more than one possibility for your diagnosis. A doctor must differentiate between multiple diagnoses to determine the correct one and make an appropriate treatment plan.
What is the Common Factors Model?
Factors necessary and sufficient for change:
- An emotionally charged bond between client and therapist
- A confiding healing setting in which therapy takes place
- A therapist who provides psychologically derived and culturally embedded explanation for emotional distress
- An explanation for distress that is adaptive, viable, and accepted by the client
- A set of procedures or rituals are enacted to address distress (i.e. treatment)
What are some developmental factors that contribute to mental illness?
It is believed that developmental trajectories or critical periods can impact the development of mental illness.
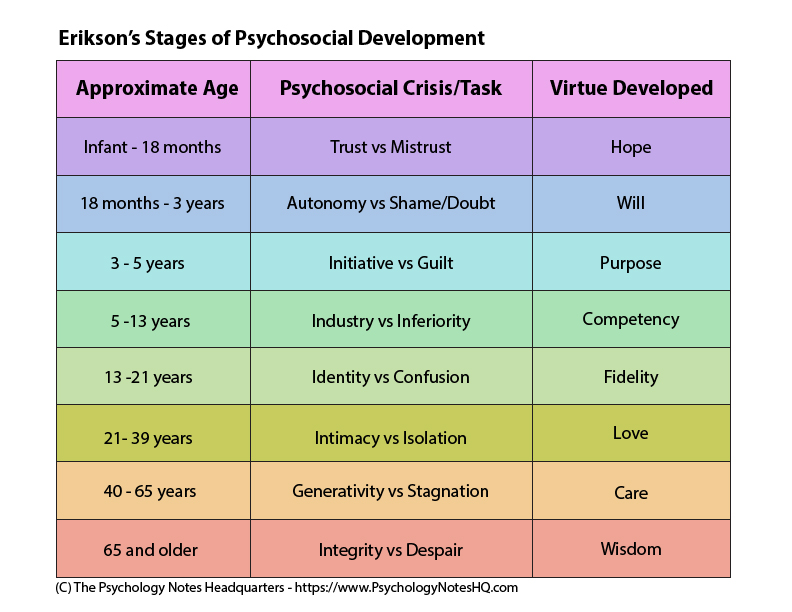
For example, Erikson believed that people advance through the stages of development based on how they adjust to social crises throughout their lives.
What manual is used to support in the diagnosis of individuals?
Diagnostic and Statistical Manual of Mental Disorders (DSM-5)
What are some of the criteria for Major Depressive Disorder?
A. The individual must be experiencing five or more symptoms during the same 2-week period and at least one of the symptoms should be either (1) depressed mood or (2) loss of interest or pleasure.
Depressed mood most of the day, nearly every day, as indicated by either subjective report or observation made by others.
Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day.
Significant weight loss when not dieting or weight gain, or decrease or increase in appetite nearly every day.
Insomnia or hypersomnia nearly every day.
Psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down).
Fatigue or loss of energy nearly every day.
Feelings of worthlessness or excessive or inappropriate guilt nearly every day.
Diminished ability to think or concentrate, or indecisiveness, nearly every day.
Recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide.
B. The symptoms cause clinically significant distress or impairment in social, occupation, or other important areas of functioning.
C. The episode is not attributable to the physiological effects of a substance or to another medical condition.
What are the differences between Major Depressive Disorder and Persistent Depressive Disorder?
The two main differences are the duration and number of symptoms.
While Major Depressive Disorder requires depressed mood most of the day, nearly every day or loss of pleasure in activities, Persistent Depressive Disorder requires depressed mood for most of the day, for more days than not for at least two years.
With Major Depressive Disorder, the individual must be experiencing five or more symptoms during the same 2-week period whereas with Persistent Depressive Disorder, they must experience two symptoms while depressed.
What are some central constructs and techniques used within the Person-Centered orientation?
Central constructs include self-actualization (humans want to grow toward harmony and complexity and we have ability to realize your potential) and need for positive regard (kindness, care, and compassion).
Client must perceive three characteristics in their therapist: genuineness, unconditional positive regard, and empathy.
What are some socio-cultural factors that contribute to mental illness?
There are many socio-cultural processes that are associated with psychopathology.
Some examples:
- Social relationships (i.e. number and quality of relationships, interpersonal dynamics)
- Beliefs and cultural norms (i.e. cultural variations in child-rearing, emotional expressivity)
- Gender effects and role deviations
What are some benefits of diagnosing?
- Categories facilitate conversation for scientists and clinicians (provides a nomenclature for practitioners)
- Provides a basis for organizing and retrieving relevant information
- Describes the common patterns of symptom presentation
- Provides a basis for prediction (course, treatment response, etc)
- Some individuals feel validated and normalized by having a diagnosis and/or explanation for their experiences
What are some of the criteria for Generalized Anxiety Disorder?
A. Excessive anxiety and worry (apprehensive expectation), occurring more days than not for at least 6 months, about a number of events or activities (such as work or school performance).
B. The person finds it difficult to control the worry.
C. The anxiety and worry are associated with three or more of the following six symptoms (with at least some symptoms present for more days than not for the past 6 months).
Restlessness or feeling keyed up or on edge
Being easily fatigued
Difficulty concentrating or mind going blank
Irritability
Muscle tension
Sleep disturbance (difficulty falling or staying asleep, or restless unsatisfying sleep)
D. The anxiety, worry, or physical symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
E. The disturbance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition (e.g., hyperthyroidism).
F. The disturbance is not better explained by another mental disorder.
What are some of the differences between Acute Stress Disorder and Post-Traumatic Stress Disorder?
The main difference is the duration since trauma exposure.
Acute Stress Disorder requires that duration of disturbance is 3 days to 1 month after trauma exposure.
Post-Traumatic Stress Disorder requires that duration of disturbance is more than 1 month.
Therefore, if symptoms persist for more than 1 month and the individual meets criteria for PTSD, their diagnosis is changed from Acute Stress Disorder to PTSD.
What are some central constructs and techniques used within the Solution Focused orientation?
Solution Focused Therapy shifts the focus from the past (a la Freud) to the future.
Basic constructs include:
- Exceptions: there is always a time when the problem doesn’t happen
- Change talk: converse in ways that bring about change
- Solutions: concentrate on acceptable solutions to the problem
- Strengths and resources: accessibility to strengths and resources
- Changing through doing, not changing through thinking
Some techniques include:
- Problem Description (ask clients to describe their problem, how they have tried to resolve these difficulties)
- Goal Setting/Miracle Question: "How would you know the problem is gone? How would your life be different?" (activates problem-solving mindset by giving people a vision of their goal
- Exploring Exceptions/Exception Question (directs clients’ attention to times when they did not have the problem and what they can do to expand the exceptions)
- Scaling Questions (help therapists and clients talk about vague topics; e.g. how sad to you feel or how motivated am I to change my relationship?)
- Coping Questions (e.g. how have you coped in the past?)
- Compliments (bring attention to the fact that the client has already done something)
- Breaking patterns (e.g., getting the client to fight in the bathroom instead of where they would normally fight)
What are some psychological factors that contribute to mental illness?
There are many psychological processes that are associated with psychopathology.
Some examples:
- Cognitive factors (i.e. thought process/content, neuropsychological factors such as attention and memory impairment)
- Behavioral factors (i.e. conditioned responses)
- Emotional reactivity and capacity for emotion regulation
- Personality traits and processes
What are some disadvantages of diagnosing?
- Diagnoses don’t account for comorbidity - the co-occurrence of “distinct” disorders, apparently interacting with one another
- Many disorders do not have distinct boundaries and none have a known etiology
- Symptoms may be better viewed along continuous dimensions of functioning
- Difficult to distinguish between normal expression of a negative emotion and having a mental disorder
- Duration cutoffs are seemingly arbitrary
- Can be stigmatizing
What are some of the criteria for Acute Stress Disorder?
A. Exposure to actual or threatened death, serious injury, or sexual violation in one or more of the following ways:
- Directly experiencing the traumatic event
- Witnessing, in person, the event as it occurs to others
- Learning that the event occurred to a close family member or close friend
- Experiencing repeated or extreme exposure to aversive details of the trauma
B. Presence of nine or more of the following symptoms from any of the five categories of intrusion, negative mood, dissociation, avoidance, or arousal:
Intrusion Symptoms
- Recurrent, involuntary and intrusive distressing memories of the traumatic event (intrusive recollections)
- Recurrent distressing dreams in which the content and/or affect of the dream are related
- Dissociative reactions (flashbacks)
- Intense or prolonged psychological distress or marked physiological reaction to cues
Negative Mood
- Persistent inability to feel positive mood states such as happiness, joy, and satisfaction (blunting of these moods)
Dissociative Symptoms
- An altered sense of the reality of one’s surroundings or oneself (distorted perception of one’s surroundings)
- Inability to remember an important aspect of the traumatic event (difficulty remembering aspects of the event)
Avoidance Symptoms
- Efforts to avoid distressing memories, thoughts, or feelings about the traumatic event
- Efforts to avoid external reminders that arouse distressing memories
Arousal Symptoms
- Sleep disturbance
- Irritable behavior and angry outbursts
- Hypervigilance
- Problems with concentration
- Exaggeration of the startle response
C. Duration of the disturbance is three days to one month
D. Clinically significant impairment or distress
E. The disturbance is not attributable to the physiological effects of a substance or to another medical condition.
What criteria is (almost) always listed to support in differentiating between diagnoses?
"The disturbance is not attributable to the physiological effects of a substance or to another medical condition."
It is important to always ensure that the symptoms are not being caused by a substance (whether illicit or prescribed) and/or another medical condition.
What are some central constructs and techniques used within the Behavioral Therapy orientation?
Central Constructs: Classical Conditioning (pairing responses a la Pavlov), Operant Conditioning (increasing or decreasing behavior a la Skinner)
Techniques: ABCs (activating event, behavior, and consequence), systematic desensitization (relaxation skills including deep breathing, progressive muscle relaxation, guided meditation, and creating a hierarchy around the phobia), exposure therapy, eye movement desensitization and reprocessing
What is the Diathesis Stress Model?
According to Diathesis-Stress Models, the cause of abnormal behavior can be view viewed as the result of an interaction between two types of factors:
- Diathesis - previous biological and environmental factors that predispose an individual towards developing a disorder or a behavior
- Stress - trigger that taxes or exceeds the individuals personal resource and results in abnormal behavior
The more diathesis there is, the less stress needed to initiate illness. However, protective factors can make it less likely that the person will experience adverse effects of the stressor.
For example, someone with low self-esteem (diathesis) who experiences adverse life effects (stress) may increase their risk of developing depressive symptoms.
What are 4 things to consider when diagnosing? (Hint: It's the 4 D's)
- Deviance - thoughts, behaviors, or emotional reactions that are unacceptable or not common in society
- Dysfunction - maladaptive behavior that impairs the individual's ability to perform normal daily functions (impairment in job, relationships, how they see themselves, etc)
- Distress - negative feelings by the individual with the disorder about the presence or the consequences of the disorder
- Danger - dangerous or violent behavior directed at the individual or others in the environment
What are some of the criteria for Post-Traumatic Stress Disorder?
A. Exposure to actual or threatened death, serious injury, or sexual violation in one or more of the following ways:
- Directly experiencing the traumatic event
- Witnessing, in person, the event as it occurs to others
- Learning that the event occurred to a close family member or close friend
- Experiencing repeated or extreme exposure to aversive details of the trauma
B. Presence of one or more of the following intrusion symptoms associated with the traumatic event:
- Recurrent, involuntary and intrusive distressing memories of the traumatic event
- Recurrent distressing dreams in which the content and/or affect of the dream are related
- Dissociative reactions (e.g., flashbacks)
- Intense or prolonged psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event
- Marked physiological reaction to internal or external cues that symbolize or resemble an aspect of the traumatic event
C. Persistent avoidance of stimuli associated with the traumatic event, as evidenced by one of the following:
- Avoidance of or efforts to avoid distressing memories, thoughts, or feelings about the traumatic event
- Avoidance of or efforts to avoid external reminders that arouse distressing memories
D. Negative alterations in cognition and mood associated with the traumatic event, as evidenced by two or more of the following:
- Inability to remember an important aspect of the traumatic event (difficulty remembering aspects of the event)
- Persistent and exaggerated negative beliefs or expectations about oneself or the world
- Persistent, distorted cognitions about the cause or consequences that lead
- individual to blame him/herself
- Persistently negative emotional state
- Markedly diminished interest or participation in activities
- Feelings of detachment or estrangement from others
- Persistent inability to experience positive emotions
E. Marked alterations in arousal and reactivity as evidenced by two or more of the following:
- Irritable behavior and angry outbursts
- Reckless or self-destructive behavior
- Hypervigilance
- Exaggeration of the startle response
- Problems with concentration
- Sleep disturbance
F. Duration of the disturbance is more than one month.
G. Clinically significant impairment or distress
H. The disturbance is not attributable to the physiological effects of a substance or to another medical condition.
What are the differences between Bipolar I and Bipolar II?
To understand the difference between the diagnoses, it is important to understand the three types of episodes: manic, hypomanic, and depressive.
Mania is a distinct period of abnormally and persistently elevated or irritable mood and abnormally and persistently increased goal-directed activity or energy lasting at least one week (or any duration if hospitalization is necessary). The mood disturbance is severe enough to cause marked impairment in social or occupational functioning or to necessitate hospitalization or there are psychotic features.
Hypomania is a distinct period of abnormally and persistently elevated or irritable mood and abnormally and persistently increased activity or energy lasting at least 4 consecutive days. The mood disturbance is not severe enough to cause marked impairment in social or occupational functioning or to necessitate hospitalization. If there are psychotic features, it is not hypomania but mania instead.
A major depressive episode is a set of symptoms from Major Depressive Disorder that must be present for a two week period.
Bipolar I must meet the criteria for a manic episode. They may also experience hypomanic or major depressive episodes.
Bipolar II must meet the criteria for a hypomanic episode and a major depressive episode. An individual must not have ever had a manic episode.
What are some central constructs and techniques used within the Cognitive Therapy orientation?
Central Constructs: Perception impacts emotions/behaviors, automatic thoughts (primal), core beliefs, cognitive distortions
Techniques: Behavioral activation, guided discovery (helps the client find the answer themselves), cognitive restructuring, downward arrow, thought record