Superficial-thickness burn 1ST degree
Sunburn, flash burn
a. Involves injury to the epidermis; the blood supply to the dermis is still intact.
b. Mild to severe erythema (pink to red) is present, but no blisters.
c. Skin blanches with pressure.
d. Burn is painful, with tingling sensation, and the pain is eased by cooling.
e. Discomfort lasts about 48 hours; desquamation(pealing skin) 2-3 days after burn, healing occurs in about 3 to 6 days.
f. No scarring occurs and skin grafts are not required.
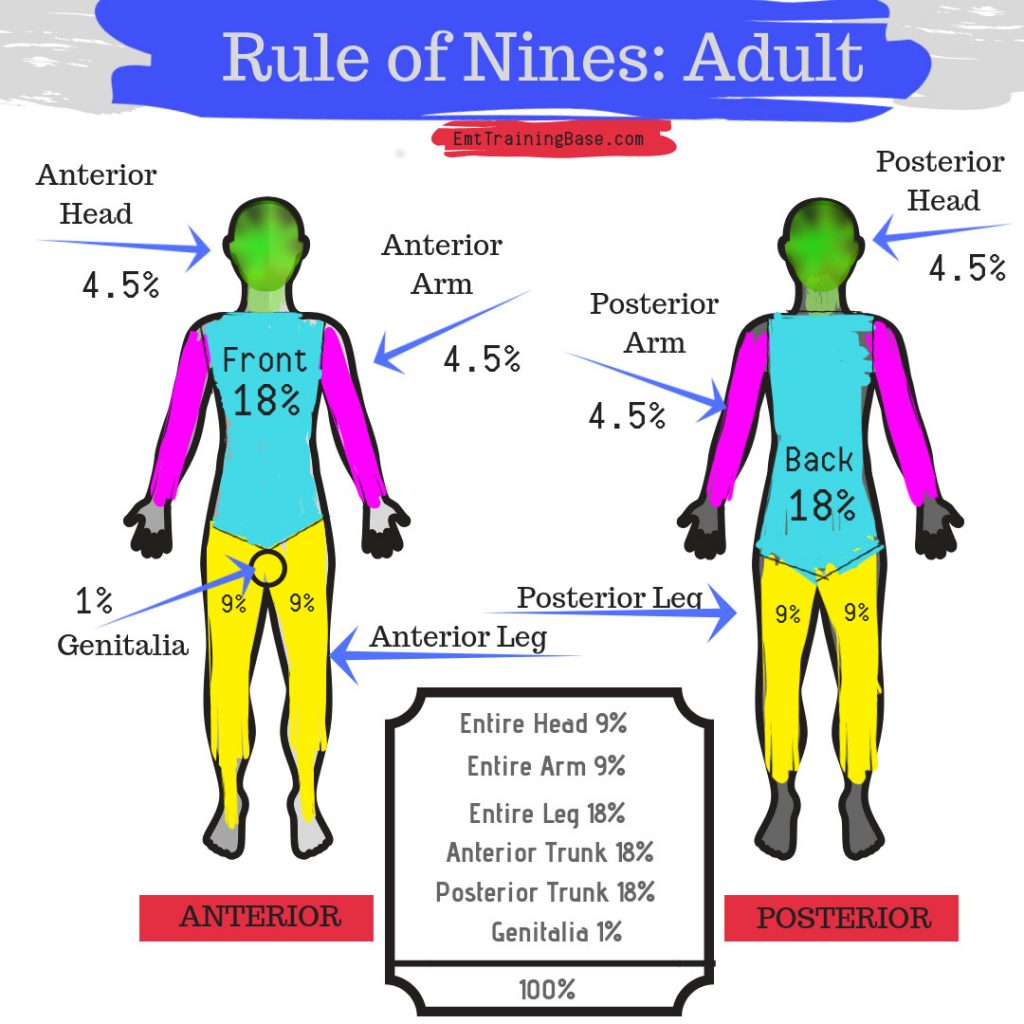
Size and depth of injury
size- Rule of 9's, depth-classification
Pulmonary
Pulmonary edema and failure related to INH injury
(Pay close attention 8-12 hours after fluid resuscitation)
Resuscitation Phase!
Emergent
24 to 48 hours—until diuresis occurs (TBSA > 25%)
• Potential for decreased oxygenation
• Potential for shock
• Pain (acute and chronic)
• Potential for Acute Respiratory Distress Syndrome
(ARDS)
Resuscitation Phase
Emergent
Interventions
Resuscitation Phase
Emergent
Interventions
• Secure airway
• Support circulation—FLUID REPLACEMENT!
• Prevent infection
• Maintain body temperature
• Provide emotional support
Superficial partial-thickness burn- 2nd degree
-scald, flame, brief contact with hot object
-deeper into the dermis, blood supply reduced
-large blisters
-mottled pink to red with a wet, shiny weepy surface
-edema
-painful and sensitive to cold air
-heals 10-21 days w/ no scarring but pigment discoloration
- grafts may be used if the healing process is prolonged
Rule of 9's
GI
Curlings Ulcer and paralytic ilius
(USE PPI’S AND H2 BLOCKERS! FEED YOUR PATIENTS!)
Surgical Management in Emergent
Phase
ESCHAROTOMY
Why is it performed?
- Compartment syndrome: Severe burns can cause tissue swelling that prevents blood from flowing easily. This can lead to compartment syndrome, which compresses blood vessels, nerves, muscles, and tissue.
- Respiratory compromise: Burns to the chest and upper torso can make it difficult to breathe.
- Loss of tissue perfusion: Burns can cause pressure to build up, which can lead to tissue perfusion loss. How is it performed?
- A senior member of the burn medical team performs the procedure using sterile technique
- Incisions are made through the eschar to release pressure
- The incisions are not closed because the area needs to be monitored
- The area is covered with sterile dressings and bandages
and FASCIOTOMY
deep partial thickness - 2nd degree
scald, flame, prolonged contact with hot object, grease, chemical, tar
- extends deeper into the dermis
- blister formation usually does not occur because dead tissue is thick and sticks to underlying viable tissue
- may or may not blanch, edema is moderate.
- can convert to full thickness if tissue damage increases by infection, hypoxia, or ischemia.
-heals in 3-6 wks, scar formation and skin grafting may be necessary
Parkland Formula
CALCULATED AT TIME OF INJURY
Crystalloid IV solution only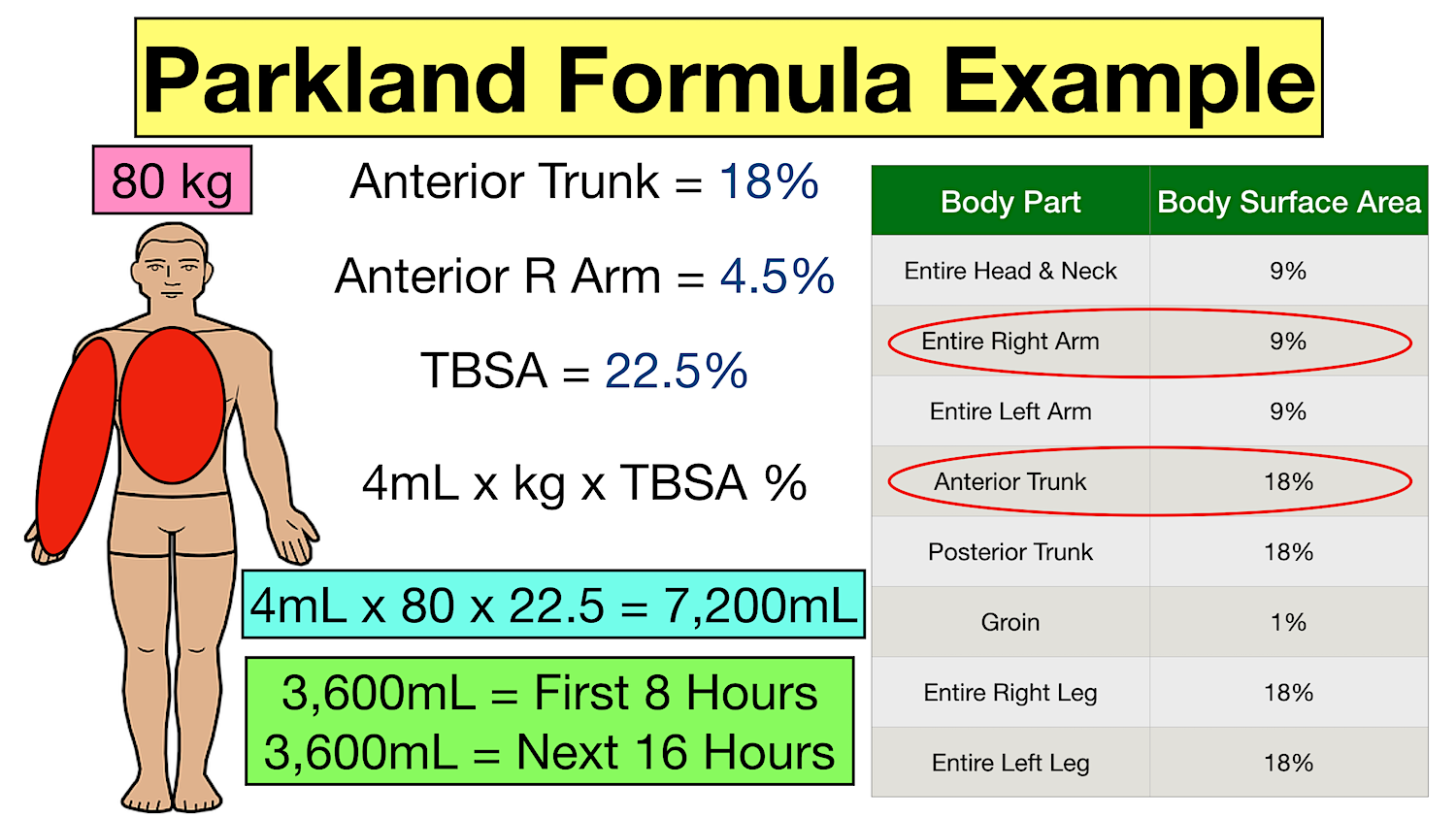
Vascular
Vasodilation – WHAT HAPPENS AS A
RESULT?
3rd spacing and/or capillary leak syndrome
Decreases blood volume
Acute Phase
Diuretic Phase
36 to 48 hour after injury; until wound closure is
completed
(remobilization of fluid)
Goals of Management
• Continued systems assessments
• Burn wound care – SEPSIS RISK!
• Pain control
• Psychosocial interventions
Acute Phase
•Mechanical debridement
•Hydrotherapy
•Enzymatic debridement
•Autolysis
•Collagenase
full thickness - 3rd degree
scald, flame, prolonged contact with hot objects, grease, tar, electricity, chemical
-destruction of dermis and epidermis into the subQ tissue, will not heal by re-epithelialization, grafting may be required.
-dry hard leathery eschar, crust and dead tissue must slough off or removed before healing can occur.
-waxy white, deep red, yellow whit or black in appearance
- edema under eschar
-sensation reduced or abesnt d/t nerve ending damage
- healing is wks -months, depends on blood supply
- requires removal of eschar and split or full thickness grafting
-scarring and wound contractures are likely
Electrolyte Imbalance
HYPERkalemia(cell destruction), HYPOnatremia
CV CO
deep full thickness - 3rd degree
flames, electricity, grease, tar, chemical
-injury beyond skin to underlying fascia and tissues, muscle tendons bone are damaged
- appears black and zero sensation
-eschar is hard and inelastic
-no pain d/t nerve endings destroyed
- healing takes months and grafts are required d/t no regrowth of tissue