I Hardly Knew Her!
I Hardly Knew Her!
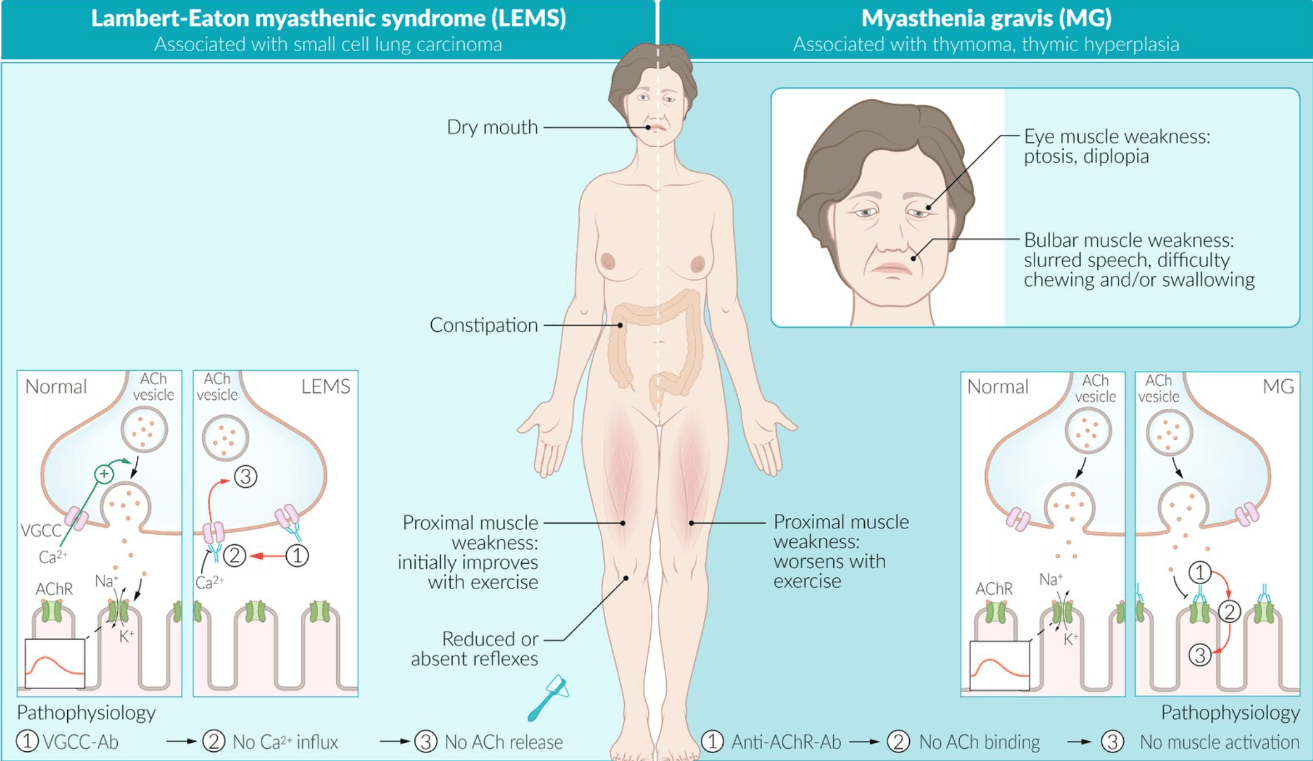
What is the hallmark symptom pattern of myasthenia gravis that helps distinguish it from other neuromuscular disorders?
Fatigable, fluctuating skeletal muscle weakness that worsens with activity and improves with rest.
Teaching note: Weakness most often begins in ocular muscles (ptosis, diplopia) and may later involve bulbar, limb, or respiratory muscles.
Describe the basic organization of the brachial plexus from its spinal root origins to its terminal branches.
The brachial plexus arises from spinal roots C5–T1, forming roots → trunks → divisions → cords → terminal branches (musculocutaneous, axillary, radial, median, and ulnar nerves)
🩺 Teaching note: Remember the mnemonic “Real Texans Drink Cold Beer” — helps track plexus levels for upper limb innervation
What is the difference between a macule and a papule on clinical and microscopic examination?
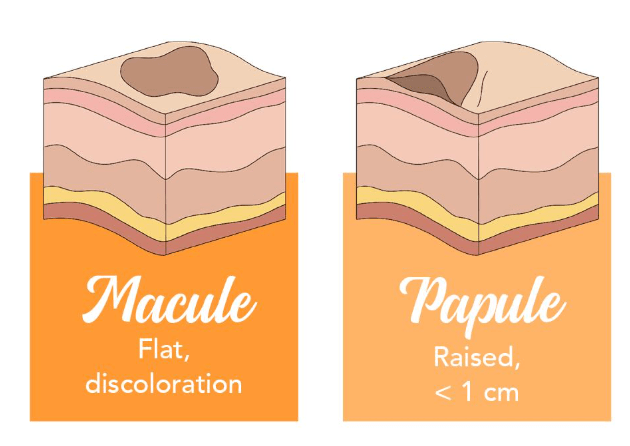 Macule: flat, circumscribed area of color change (<1 cm), no elevation or depression; histologically shows pigment or vascular change without thickness.
Macule: flat, circumscribed area of color change (<1 cm), no elevation or depression; histologically shows pigment or vascular change without thickness.
Papule: elevated, solid lesion (<1 cm), with epidermal or dermal thickening.
🩺 Teaching note: Plaques are simply confluence of papules — same concept, broader area.
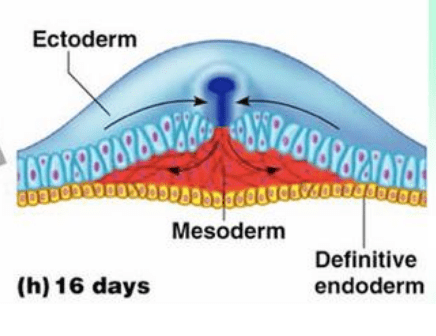
What are the two layers of the bilaminar germ disc, and what do they each form?
Epiblast: gives rise to all three germ layers (ectoderm, mesoderm, endoderm).
Hypoblast: contributes to formation of the yolk sac lining.
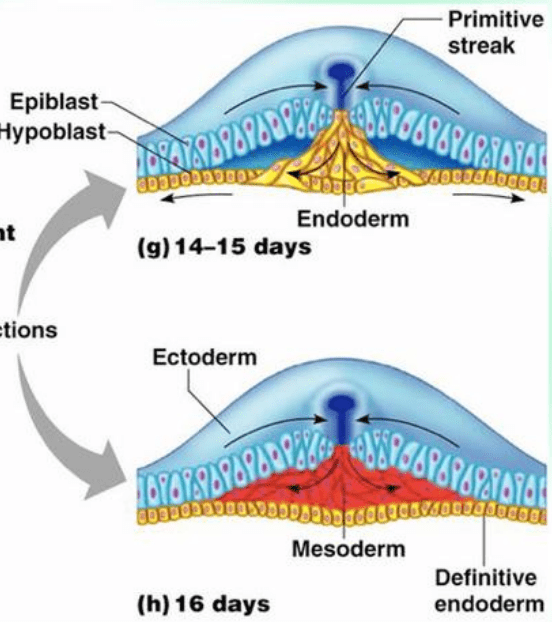
🩺 Teaching note: The bilaminar disc forms during week 2 — “two layers in week two” is the classic mnemonic.
What is the main pathophysiologic mechanism driving plaque psoriasis?
Overactivation of T-helper (Th1/Th17) cells leads to cytokine-mediated keratinocyte hyperproliferation and inflammation in the epidermis.
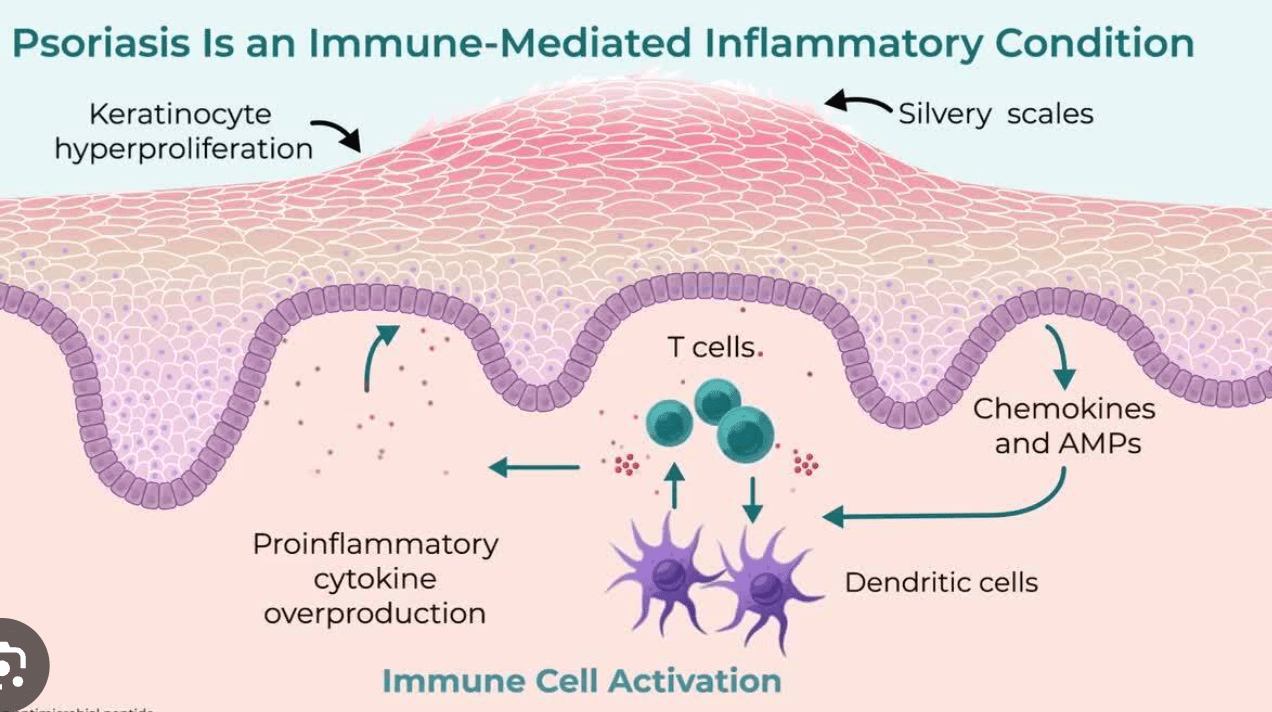 🩺 Teaching note: Results in well-demarcated erythematous plaques with silvery scales.
🩺 Teaching note: Results in well-demarcated erythematous plaques with silvery scales.
What are the typical deep tendon reflex and pupillary findings in patients with myasthenia gravis?
Deep tendon reflexes and pupils are normal.
🩺 Teaching note: MG affects voluntary skeletal muscle, not smooth muscle (like the iris), so pupils remain unaffected- unlike cranial nerve III palsy.
What are the major branches of the axillary artery, and how are they divided by their relation to the pectoralis minor muscle?
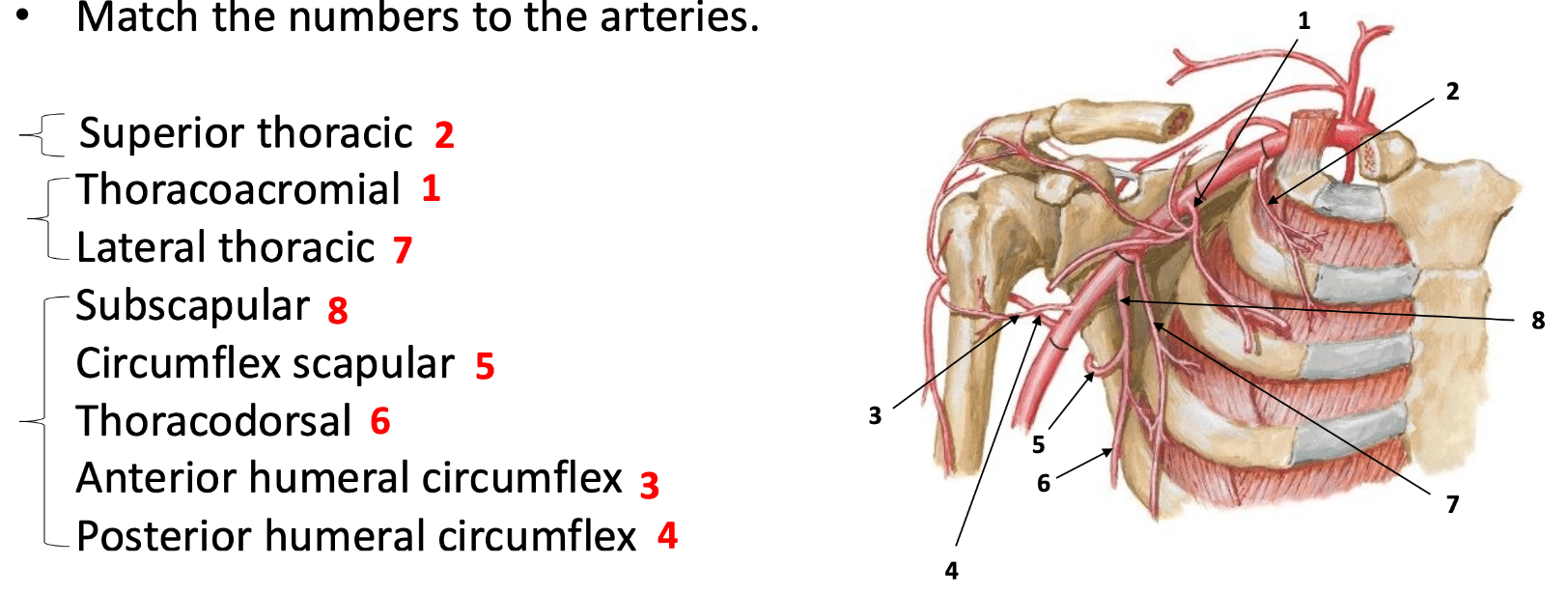
🩺 Teaching note: The axillary artery originates from the subclavian and terminates as brachial artery at the lower border of teres major
Define and differentiate vesicle, bulla, and pustule based on their contents and histology.
Vesicle: small (<1 cm) fluid-filled cavity within or below the epidermis.
Bulla: larger (>1 cm) blister, same mechanism.
Pustule: pus-filled cavity with neutrophilic infiltrate.
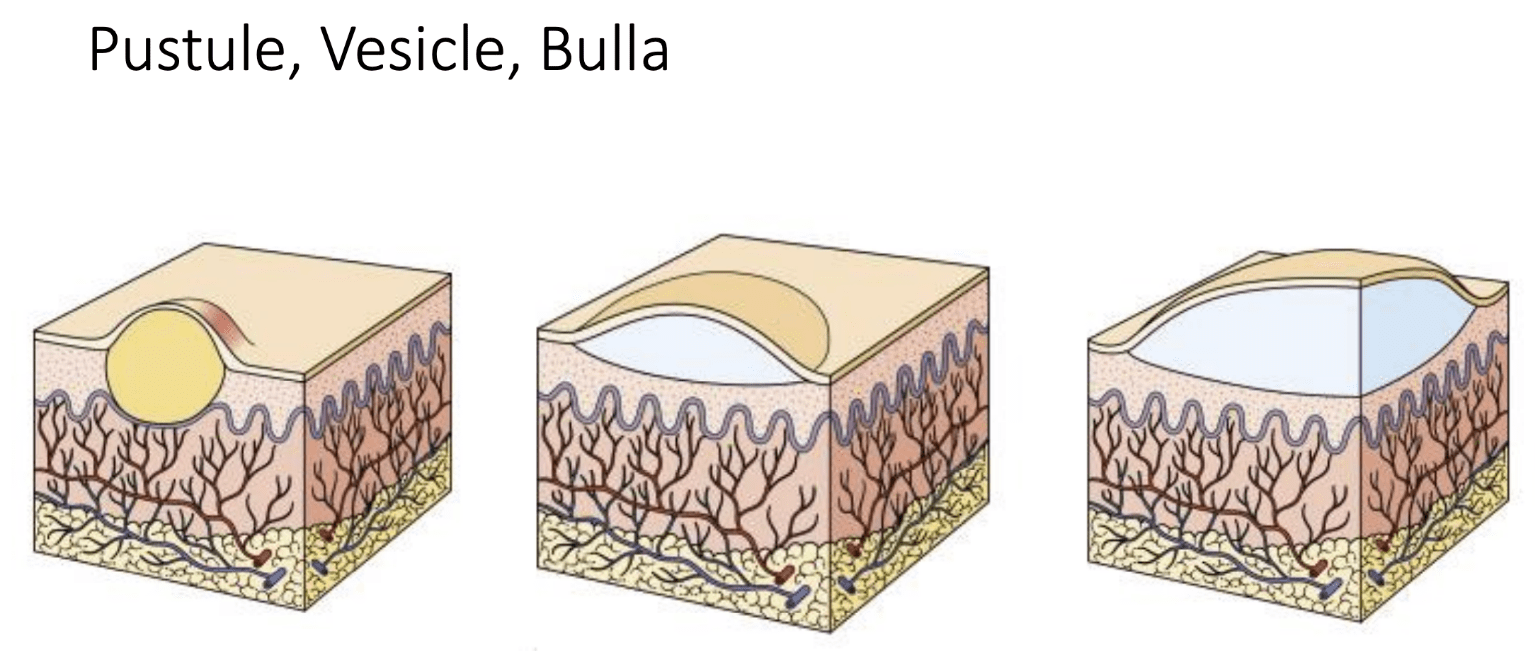
🩺 Teaching note: These are primary skin lesions — early features of inflammatory or infectious dermatoses.
Describe the process of gastrulation and list the three germ layers formed from the primitive streak.
Epiblast cells migrate inward through the primitive streak (invagination), displacing the hypoblast and forming:
Ectoderm (outer layer → epidermis, neural tissue)
Mesoderm (muscles, bones, connective tissue)
Endoderm (gut lining, glands)
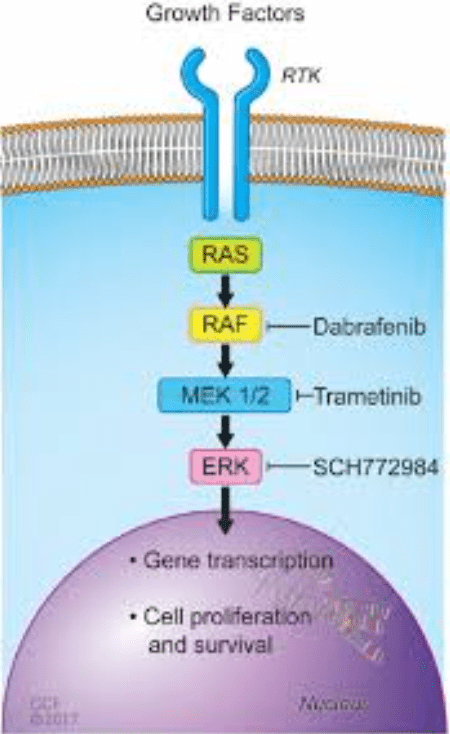
What are the molecular targets of the small-molecule inhibitors dabrafenib and trametinib used in melanoma treatment?
Dabrafenib: inhibits the mutant BRAF V600E kinase.
Trametinib: inhibits MEK1/2, downstream of BRAF in the MAPK pathway.
What is the underlying autoimmune mechanism that causes the weakness in myasthenia gravis?
Autoantibodies target acetylcholine receptors (AChR) or related proteins (MuSK/LRP4), reducing receptor numbers and activating complement, which disrupts neuromuscular transmission.
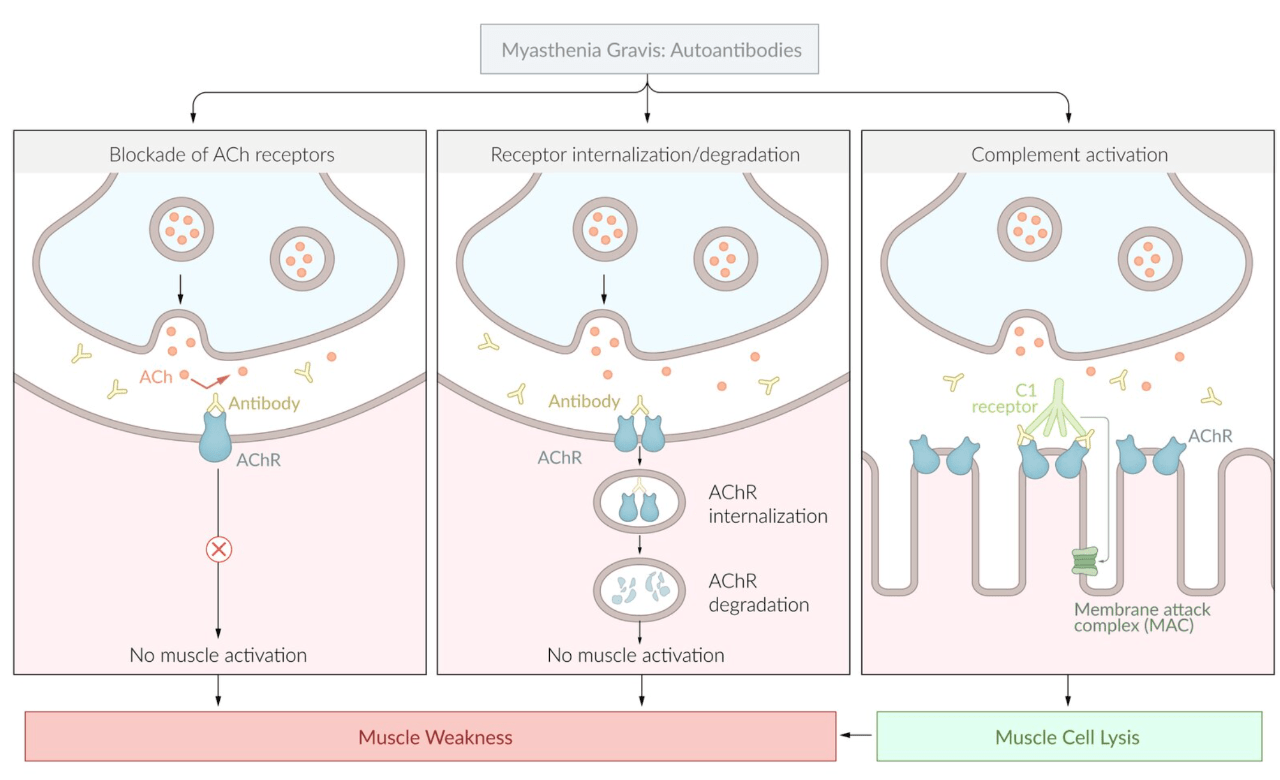 🩺 Teaching note: The result is a decreased safety factor at the neuromuscular junction, producing activity-dependent fatigue.
🩺 Teaching note: The result is a decreased safety factor at the neuromuscular junction, producing activity-dependent fatigue.
What are the main terminal branches of the brachial plexus and the major muscles they innervate?
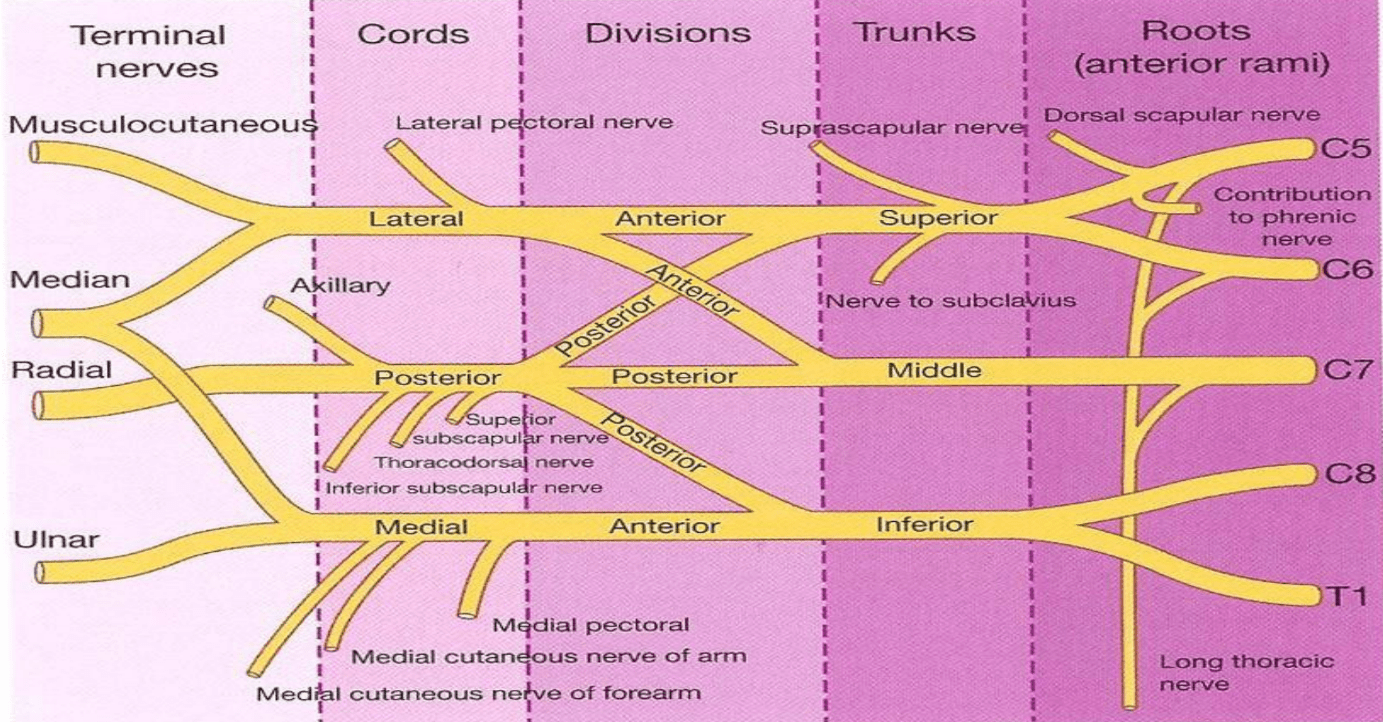 Musculocutaneous: biceps brachii, brachialis, coracobrachialis
Musculocutaneous: biceps brachii, brachialis, coracobrachialis
Axillary: deltoid, teres minor
Radial: triceps brachii, extensors of forearm
Median: most forearm flexors, thenar muscles
Ulnar: flexor carpi ulnaris, medial half of flexor digitorum profundus, most intrinsic hand muscles
What are the key microscopic findings of epidermal hyperplasia (acanthosis) and hyperkeratosis, and which common skin disorder features both?
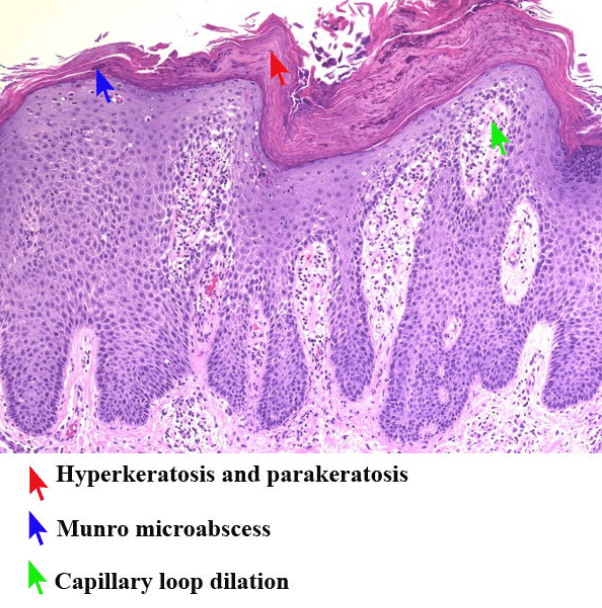 Acanthosis: thickened stratum spinosum with elongated rete ridges.
Acanthosis: thickened stratum spinosum with elongated rete ridges.Hyperkeratosis: thickened stratum corneum, often with retained nuclei (parakeratosis).
Seen together in psoriasis
🩺 Teaching note: These reflect chronic epidermal stimulation and accelerated keratinocyte turnover.
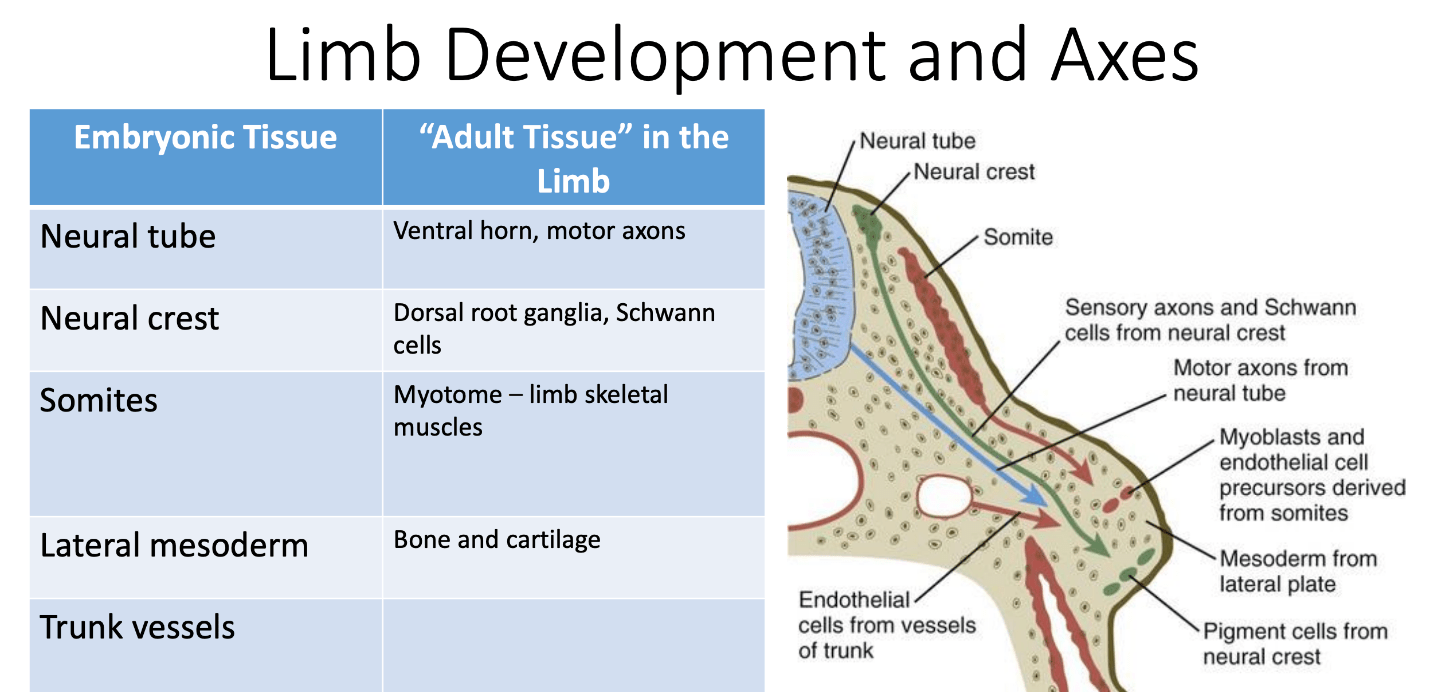
What do somites become in "adult tissue" in the limb?
Myotome – limb skeletal muscles.
What is the Parkland formula, and how is it applied in burn management?
4 mL × body weight (kg) × %TBSA burned
Half of the volume is given in the first 8 hours, and the other half over the next 16 hours.
🩺 Teaching note: Used for initial fluid resuscitation in severe burns to prevent hypovolemic shock.
What diagnostic test shows a “decremental” response in patients with myasthenia gravis, and what does that finding mean?
The repetitive nerve stimulation (RNS) test shows a progressive ≥10% fall in compound muscle action potential amplitude, indicating impaired neuromuscular transmission.
🩺 Teaching note: The test mimics repetitive use of muscles; single-fiber EMG is even more sensitive when RNS is inconclusive.
Describe the lymphatic drainage of the breast and explain its clinical importance.
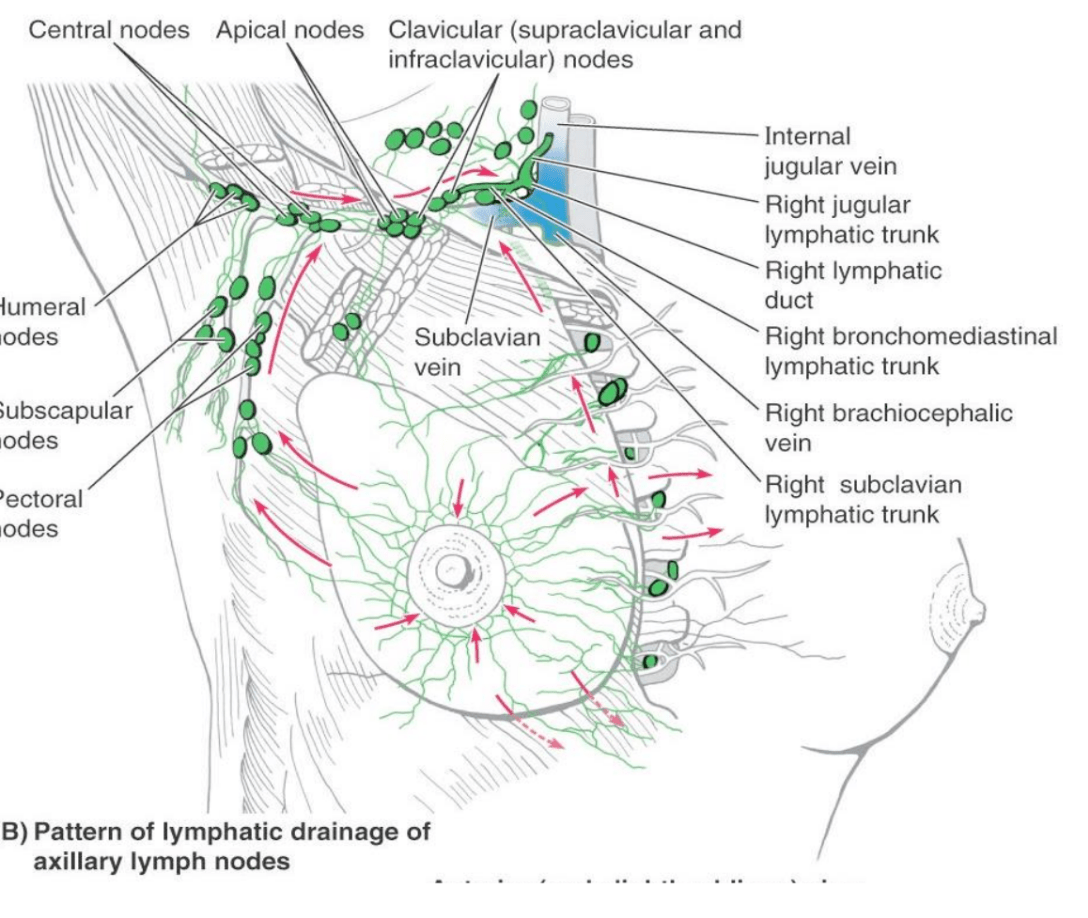
The lateral quadrants drain mainly to axillary lymph nodes, especially the anterior (pectoral) group; medial quadrants may drain to parasternal nodes.
🩺 Teaching note: This pathway explains axillary node involvement in breast cancer metastasis and why mastectomy requires careful nerve preservation (e.g., long thoracic, thoracodorsal nerves)
Describe the clinical and histologic features of the secondary skin lesion “crust”, and how it relates to erosion, ulcer, and fissure.
Crust: dried serum, blood, or exudate on the surface of a lesion — represents healing or surface damage.
Forms after erosion or ulceration; may line the edges of a fissure.
🩺 Teaching note: Crust formation signals superficial epidermal loss and helps distinguish exudative from scaly lesions.
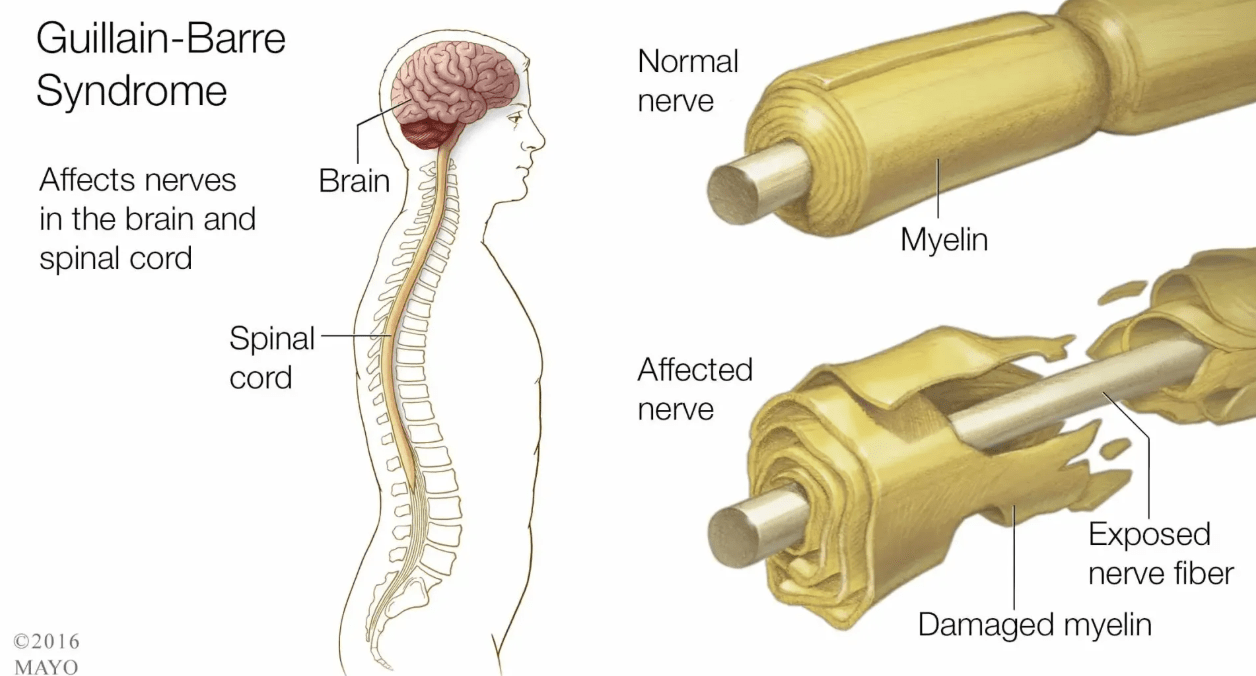
How does myelination increases the speed of nerve conduction and what occurs in demyelinating neuropathies such as Guillain–Barré syndrome?
Myelin insulates axons, allowing action potentials to jump between nodes of Ranvier via saltatory conduction, greatly increasing conduction velocity.
Loss of myelin slows or blocks conduction → weakness, areflexia, and sensory loss.
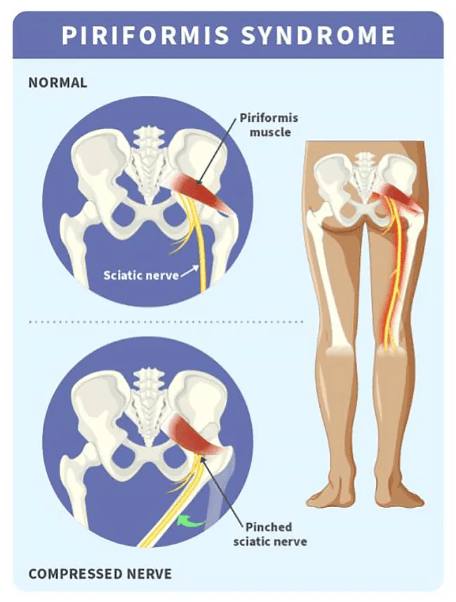
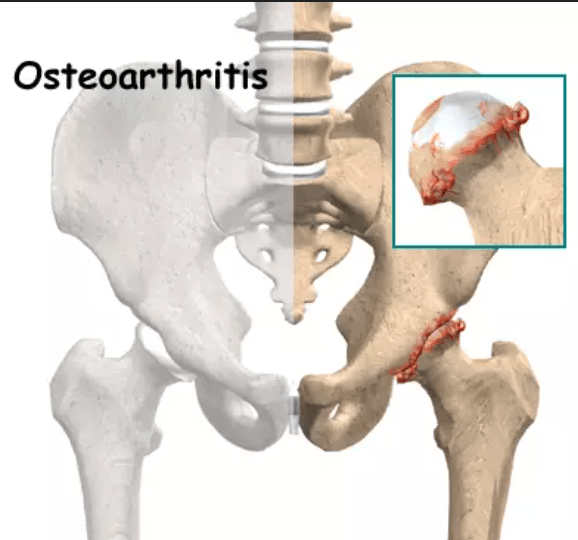
What physical exam finding helps distinguish piriformis syndrome from hip osteoarthritis?
Piriformis syndrome causes buttock pain radiating down the leg worsened by hip rotation, while osteoarthritis causes groin pain and limited range of motion.
🩺 Teaching note: Piriformis compresses the sciatic nerve; OA involves degenerative joint changes.
How does pyridostigmine improve muscle strength in patients with myasthenia gravis?
It inhibits acetylcholinesterase, prolonging acetylcholine action at the synaptic cleft and enhancing transmission at the remaining functional receptors.
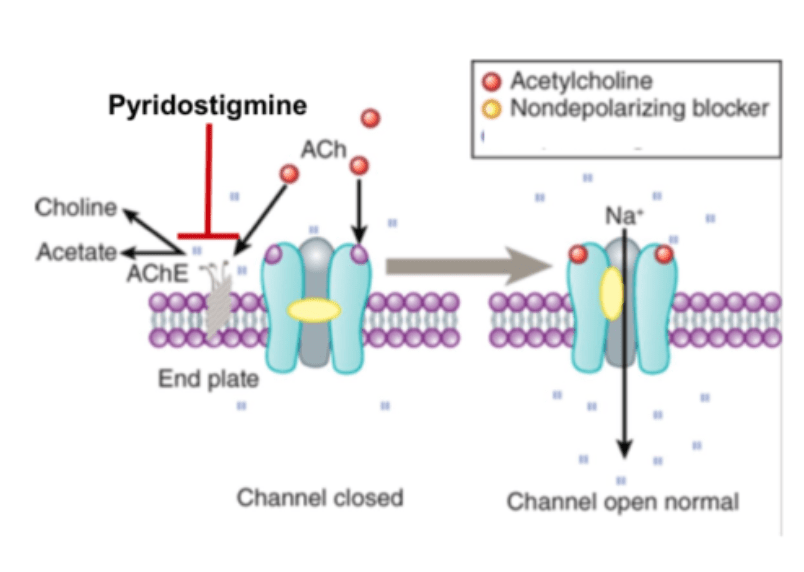 🩺 Teaching note: It’s first-line symptomatic therapy- main side effects include GI upset and increased secretions due to cholinergic activity.
🩺 Teaching note: It’s first-line symptomatic therapy- main side effects include GI upset and increased secretions due to cholinergic activity.
What are the boundaries and contents of the cubital fossa, and why is this area clinically significant?
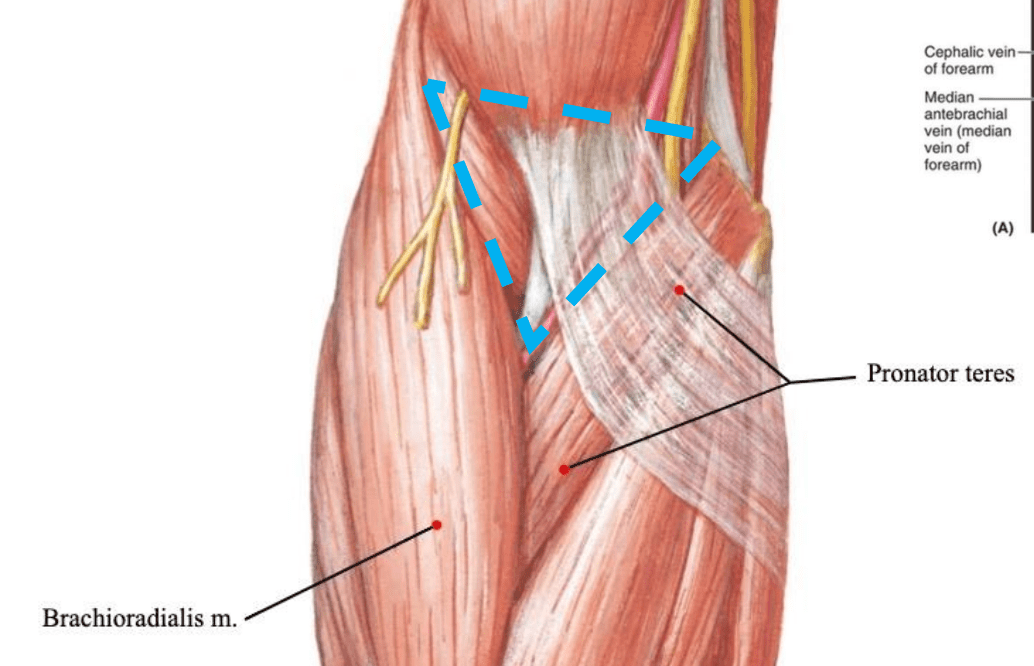
Boundaries:
Superior: imaginary line between humeral epicondyles
Medial: pronator teres m.
Lateral: brachioradialis m.
Contents (lateral to medial): radial n., biceps tendon, brachial a., median n. (RTAM)
🩺 Teaching note: It’s a key site for venipuncture and evaluation of brachial artery pulse; nerve/artery injury can occur during trauma or procedures
Describe the pathogenesis and key clinical features of Cutibacterium (Propionibacterium) acnes infection leading to acne vulgaris and outline one pharmacologic treatment.
Pathogenesis: Follicular keratin plug + sebum accumulation → bacterial proliferation → inflammation.
Clinical: Comedones, papules, pustules on face, chest, back.
Treatment: Topical retinoids or benzoyl peroxide (pharmacologic)
🩺 Teaching note: Antibiotic resistance concerns make combination therapies standard of care.
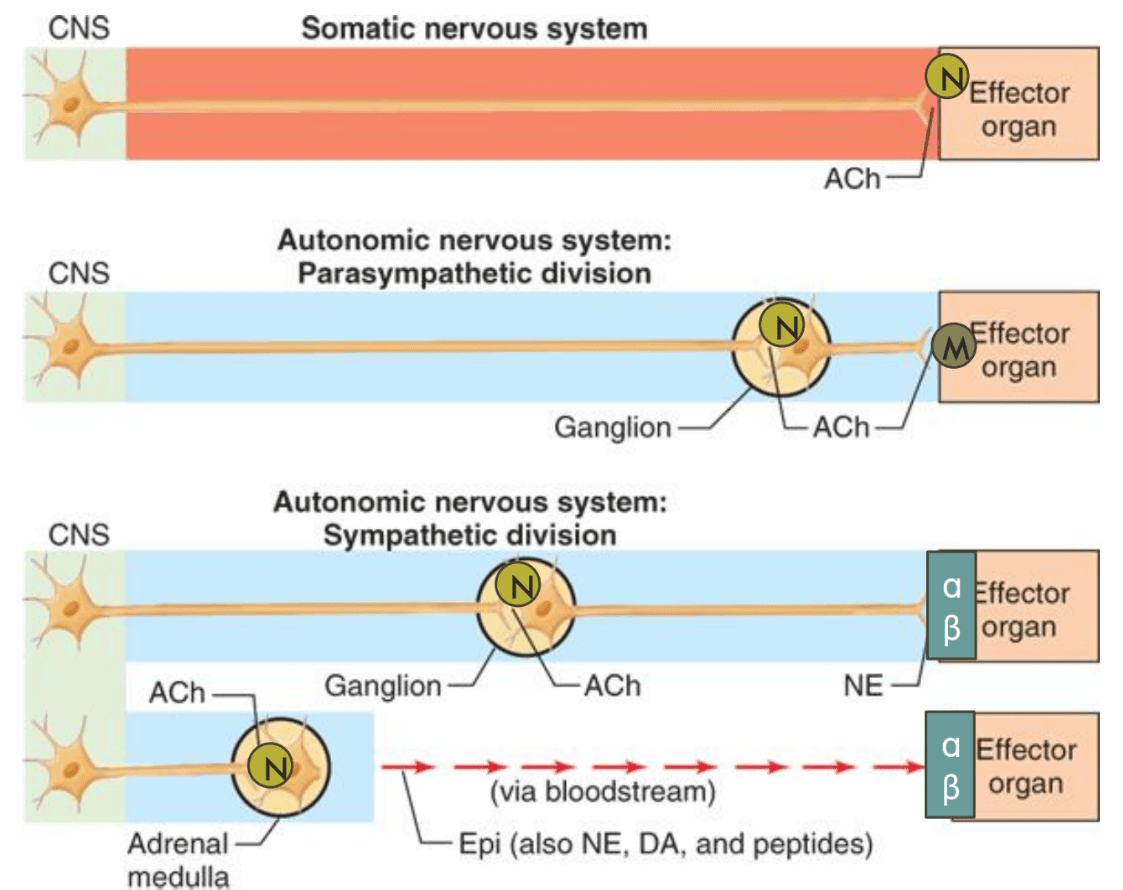
Compare the somatic and autonomic divisions of the peripheral nervous system in terms of structure, neurotransmitters, and effect.
Somatic: single neuron; acetylcholine → skeletal muscle; voluntary, excitatory only.
Autonomic: two-neuron chain;
Sympathetic: ACh → norepinephrine; fight/flight
Parasympathetic: ACh → ACh; rest/digest
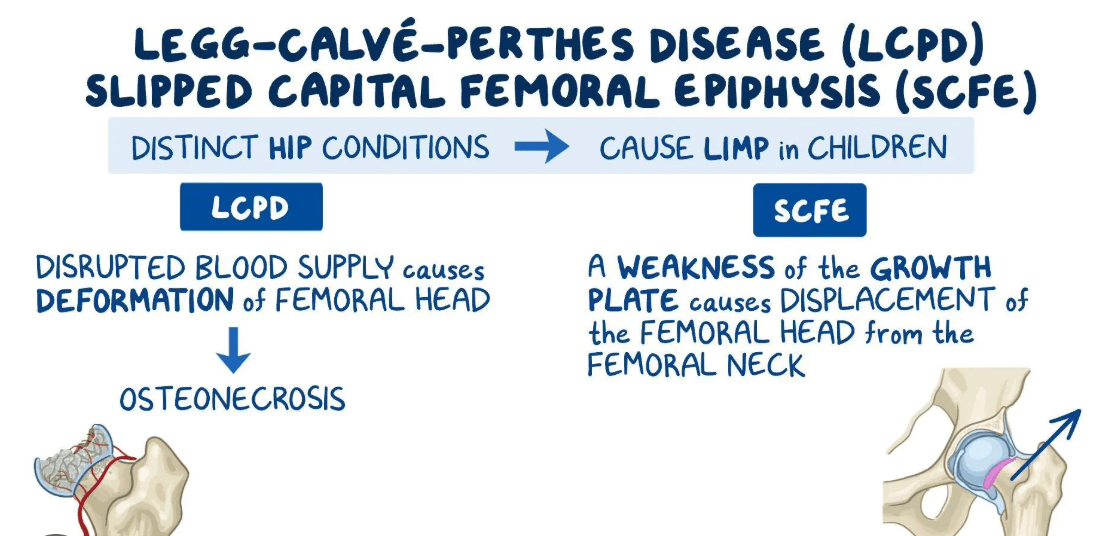
How do Legg–Calvé–Perthes disease and Slipped Capital Femoral Epiphysis (SCFE) differ in presentation?
Perthes: idiopathic avascular necrosis of femoral head; affects boys 4–8 years, presents with painless limp.
SCFE: displacement of femoral epiphysis; affects obese adolescents, presents with painful limp.