What does a low hemoglobin level indicate about oxygen-carrying capacity?
Decreased oxygen-carrying capacity and risk for inadequate tissue perfusion
What are some Mnemonics for Pain Assessment?
PQRST, OLDCARTS (Note: you will not be tested on the mnemonic itself but you will have to apply this in test questions)
Describe a Stage 1 pressure injury.
Intact skin with non-blanchable redness
What is the body's primary source of energy?
Carbohydrates
What is the correct order for abdominal assessment?
Inspection, Auscultation, Percussion, Palpation
What does an elevated WBC indicate?
The body is actively fighting an infection
What is the gold standard for pain assessment?
Patient's self-report (pain is subjective)
How often should immobile patients be repositioned to prevent pressure injuries?
Every 2 hours
What position should a patient be in when eating to reduce aspiration risk?
Upright at 90 degrees (high Fowler's position)
Why is auscultation done BEFORE palpation in abdominal assessment?
Touching the abdomen can stimulate or alter bowel sounds
What should the patient do with the FIRST morning urine specimen when starting a 24-hour urine collection?
Void and DISCARD it (start with empty bladder)
What is the difference between acute pain and chronic pain in terms of duration?
Acute pain has sudden onset and resolves with healing; chronic pain lasts longer than 6 months
What does the Braden Scale assess and what does a lower score indicate?
Assesses patient's risk for pressure injury; lower score = higher risk
What are the signs and symptoms of hypoglycemia (low blood sugar)?
Tremors, sweating, confusion, dizziness, hunger
What do absent bowel sounds indicate?
Paralytic ileus (temporary impairment of intestinal motility; no contractions = food/fluids do not pass through digestive tract) or obstruction (no sounds after 3-5 minutes per quadrant)
Name ONE things to assess before administering contrast dye.
Allergy to iodine/shellfish, kidney function.
You should also about metformin use but we have not gone over medications (save that info for Semester 2)
When should you use a cold pack versus a hot pack?
Cold pack for acute injuries/reduces swelling; Hot pack for chronic pain/relaxes muscles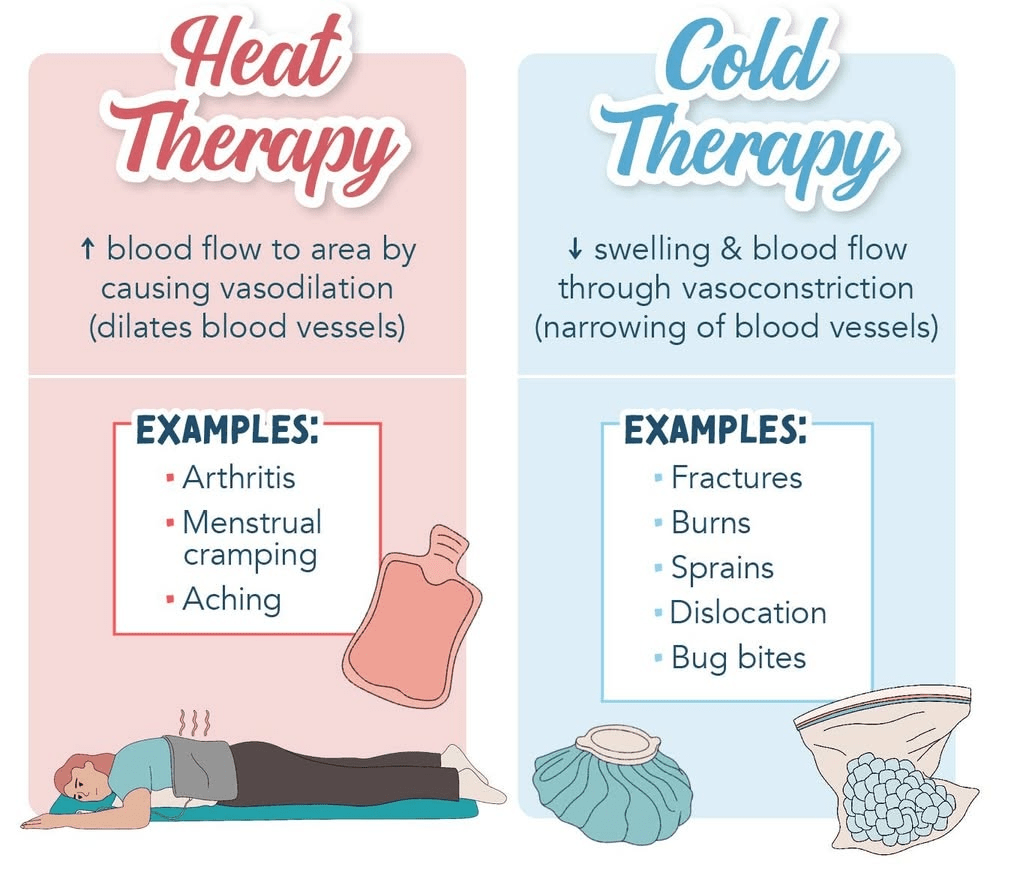
Name FOUR factors that negatively impact wound healing.
Poor nutrition, inadequate hydration, poor circulation, infection, chronic diseases, smoking, age, medications (any 4)
A patient with diarrhea should eat what kinds of food?
Bland, low-fiber to help firm stool such as bananas, rice, applesauce, toast
List two risk factors for constipation.
Immobility, inadequate fluid intake, low-fiber diet, opioid medications, ignoring urge to defecate (any 2)
What does HbA1c measure and what time period does it reflect?
Average blood glucose control over the past 2-3 months (reflects RBC lifespan)
List THREE nursing interventions to prepare the environment for sleep.
Reduce noise, dim lights, maintain comfortable temperature, cluster care activities, manage pain before bedtime (any 3)
What stage is this ulcer?
The presence of both eschar/slough is hiding the true depth of this pressure injury, making it unstageable.
What important teaching must you give when a patient increases fiber intake?
Must increase water intake (fiber absorbs water; without enough water can worsen constipation)
What is a vagal response during an enema and what should you do if it occurs?
Sudden drop in heart rate and BP causing dizziness/fainting; STOP the procedure, keep patient safe, monitor vital signs