Acute inflammation of the lungs in which the alveoli and bronchi become plugged with thick fluid.
Causes productive cough, fever, tachypnea, pleuritic chest pain, dyspnea, and systemic malaise, myalgias, and anorexia.
What is pneumonia?
Distinguishing symptoms: fever, tachypnea, and dyspnea.
Infections can be acquired in the community (CAP), the hospital (HAP), or ventilator associated (VAP).
Can be caused by bacteria, viruses, fungi, or non-infectious irritants like chemicals, smoke, aspirating food/water/vomit.
Can lead to sepsis and is a major cause of death.
Patho: inflammation leads to migration of WBCs, capillary leak, and accumulation of edema/exudates. Fluid collects around alveolar resulting in impaired gas exchange.
Treatment depends on suspected etiology, symptoms should show improvement after drug therapy started.
If a patient with asthma is using their rescue albuterol inhaler more than twice weekly for symptom management, the nurse knows the patient should start taking this type of daily inhaler.
What is corticosteroid inhaler?
Additional questions:
What are other ways to help prevent asthma attacks or exacerbations? Think of interventions inside and outside of the home
Are there any other medications that may be helpful for managing asthma?
This medication is used to treat influenza and can be prescribed for this condition within 48hour of symptom onset.
What is oseltamivir (Tamiflu)?
This pattern of bowel inflammatory differentiates Crohn's disease from ulcerative colitis.
What is:
Crohn's disease affects patches of bowel from the mouth to the anus whereas ulcerative colitis affects continuous stretches of only the colon/rectum.
Tachycardia, decreased urinary output, and confusion are all signs of this condition.
What is dehydration?
Recommended vaccination annually for this acute viral infection that causes severe muscle aches, fever, chills, fatigue, sore throat, and rhinorrhea.
What is seasonal influenza?
For a patient with COPD that is on supplemental oxygen, this is the appropriate range for oxygen saturation.
Patients with COPD that need supplemental oxygen should only be using enough oxygen to maintain an oxygen saturation of 88-92%. This has to do with diminished respiratory drive due to chronic exposure to increased levels of CO2.
This class of inhaled medications can be used in pneumonia to treat dyspnea and wheezing.
What are bronchodilators?
This differentiates upper GI bleeds from lower GI bleeds.
What are:
Upper sx: red or coffee-ground emesis, melena, decreased BP; increased HR
Diagnostics: EGD to find source
Lower sx: Bright bloody stool or melena stool, decreased BP; increased HR
Diagnostics: colonoscopy
These are all ways to treat hypokalemia.
What is liquid potassium, IV potassium, and potassium-rich foods?
Additional questions:
What foods are rich in potassium?
What is the appropriate rate for administration of IV potassium?
This disease is not considered contagious if there are no presenting symptoms or evidence of disease on chest x-ray or sputum culture.
What is tuberculosis (TB)?
Most common bacterial infection worldwide.
Spread by airborne droplets.
It is common to be infected with the bacillus and never develop active TB. A healthy individual can fight off the growth of bacillus, but lesions that form can remain inactive.
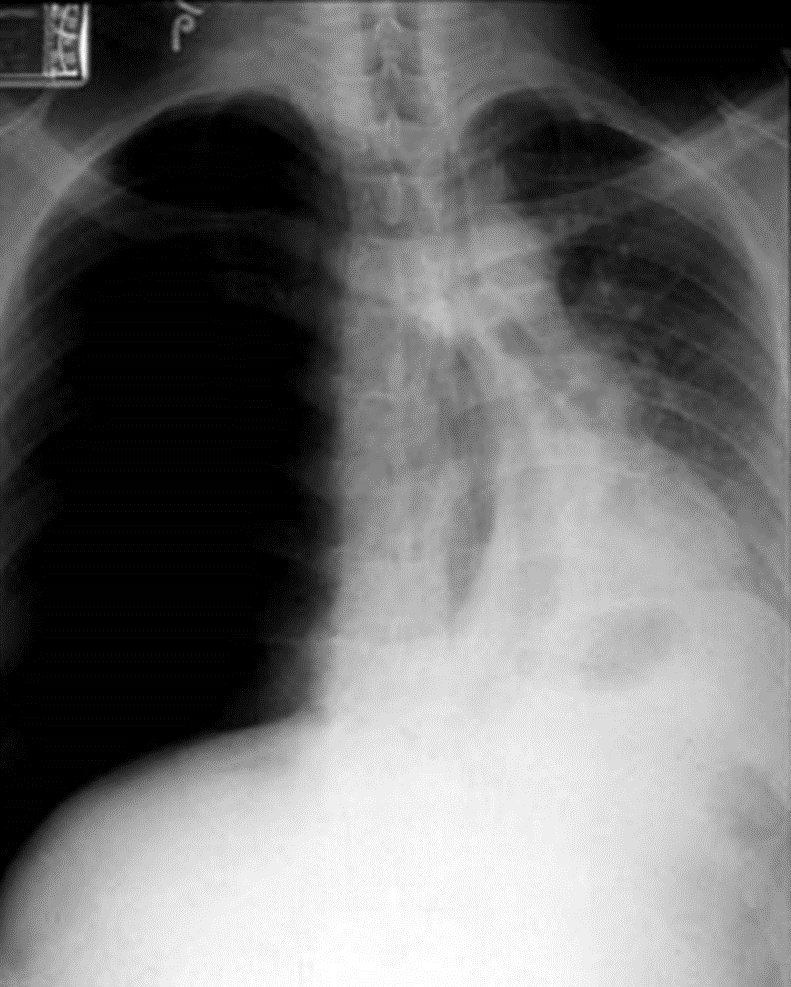
The presence of blood in the pleural space.
What is Hemothorax?
Remember a collection of (non-blood) fluid in the pleural space is called a pleural effusion.
Either condition may require a chest tube.
A procedure performed to remove fluid in the pleural space, obtain a specimen for diagnostic testing, and/or relieve dyspnea and improve respiratory compromise.
What is a thoracentesis?
These are at least two complications of ulcerative colitis.
What are:
-F&E imbalance
-Bowel perforation and peritonitis
-Toxic megacolon
-Colon cancer
S/sx: Abdominal pain/cramping (usually LLQ), bloody diarrhea with mucus, urgency and tenesmus, weight loss, fatigue, fever, rectal bleeding (more often than with Crohn’s)
Tx: low-fiber diet, mesalamine anti-inflammatory, colectomy
Prevention: colonoscopies for colon cancer screening
Hyperventilation related to anxiety is most likely to result in this acid-base disorder.
What is respiratory alkalosis?
ABG example: pH 7.52, PaCO2 25 mm Hg, HCO3- 24 mEq/L, and PaO2 95 mm Hg.
Terminology for accumulation of fluid in the pleural cavity.
Bubbling in the water seal chamber of the chest tube generally indicates one of these two possibilities.
What is slow, steady bubbling that indicates drainage of air from the pleural cavity?
or
What is rapid, continuous bubbling that indicates a leak in the chest tube system?
Patients receiving pharmacotherapy for tuberculosis need close monitoring of this organ due to possible toxicity.
What is the liver?
Combination drug therapy with strict adherence for 6-12 months includes:
-Isoniazid
-Rifampin
-Pyrazinamide
-Ethambutol
A patient with a history of peptic ulcers presents with anorexia and severe abdominal pain. The nurse notes that the abdomen is rigid and the patient's temperature is 101.1° F. The nurse is concerned about this serious complication.
What is peritonitis?
Life-threatening, acute inflammation of peritoneum
Causes: Bacterial, chemical (bile, gastric acid, digestive enzymes)
Infectious:
Bowel perforation: cancer, trauma, peptic ulcers, diverticulitis
Intra-abdominal infections (pancreatitis, cholecystitis), post-op, spontaneous (cirrhosis)
Chemical: bile, urine, blood, pancreatic enzymes
S/Sx: Abdominal Pain, Tenderness, High fever, Rigid board-like abdomen, Distended abdomen, N/V
Complications: Third spacing results, Hypovolemic shock, Septicemia, Respiratory problems, Death
Treatment: ABC, ABX, IV fluids, I+O, O2, Semi-Fowler position, surgery (for repair of perforation)
Unmanaged diabetes with hyperglycemia and Kussmaul's respirations can lead to this acid-base disorder.
What is diabetic ketoacidosis (DKA)?
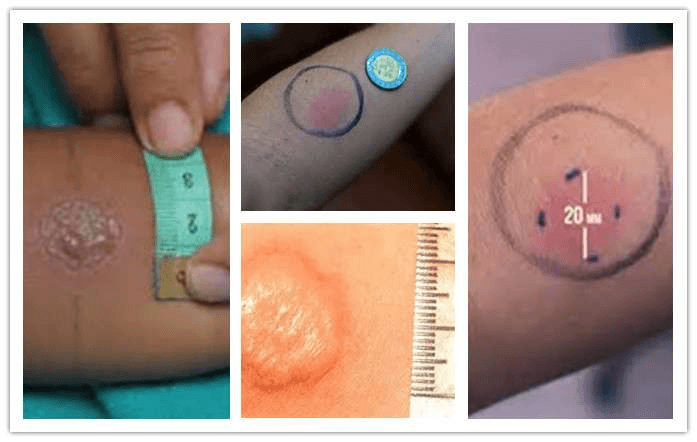
These types of patients with tuberculosis can have a negative PPD (purified protein derivative) skin test.
What is immunocompromised or elderly?
Tuberculosis (TB)? is a highly contagious disease transmitted through inhalation or swallowing of droplets contaminated with the TB Bacillus. Patients that are immunocompromised or elderly can get a sputum test or QuantiFERON Gold TB blood test.
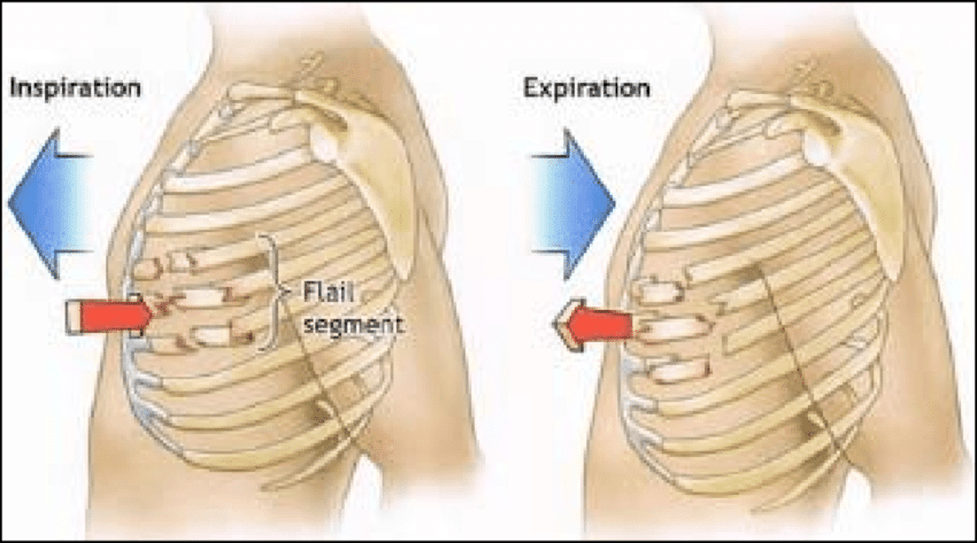
This term describes paradoxical chest wall movement, usually as a result of chest trauma.
What is flail chest?
Result of two or more contiguous rib fractures with two or more breaks in each broken rib.
Important interventions:
-Pain management
-Deep breathing and coughing
-Secretion management
-Frequent assessments
Stat ABG, supplemental oxygen, and CT scan with contrast are all common orders to diagnose and treat this serious medical condition.
What is pulmonary embolism?
A patient with gastric cancer has underwent a gastrectomy. To decrease risk of developing dump syndrome, the nurse educates the patient to follow this kind of diet.
What are small, frequent meals and no liquid with meals?
Early S/Sx (30 min)
•Fluid shift into the small intestine
•Hypotension: vertigo, tachycardia, syncope, sweating, pallor, palpitations
Late S/Sx (90 min to 3 hrs)
•Excessive amount of insulin --> rapid rise in blood glucose level from rapid entry of high carbohydrate food into jejunum
•S/Sx of hypoglycemia
How do we prevent it?
•Small frequent meals, no fluids with meals, no high carb meals
Regular insulin 10unit IV and dextrose 50% 25mL IV are common orders to treat this serious electrolyte abnormality.
What is hyperkalemia?
Additional questions:
What is the mechanism of action of these drugs to lower the potassium level in the blood?
Which medication would you want to administer first, why?
A patient with active tuberculosis needs to be placed in this type of isolation room to prevent spread of disease.
What is negative pressure room?
Remember that negative pressure rooms, the air is sucking into the room to prevent the tuberculosis bacteria in the room from escaping.
Whereas positive pressure rooms are pushing out of the room, for patients that are immunocompromised, to push out bacteria and other pathogens trying to get into the room that could possibly infect that patient.
This life threatening emergency develops when air becomes trapped in pleural cavity, causing complete collapse of affected lung and tracheal deviation.
What is tension pneumothorax?
Patient needs emergent decompression of trapped air, this would be performed with large bore needle by medical provider.
A patient is started on a heparin infusion for management of a large pulmonary embolism.
The order: heparin (25,000units/500mL) 850 units/hour IV starting now.
How many mL/hr should the nurse program into the IV pump?
What is 17mL/hr?
A patient presenting to the emergency department is vomiting copious amounts of bright red blood, this is the priority nursing intervention.
What is maintain the patient's airway?
Priority interventions: ABCs and stop bleeding
A patient with an obstruction or large or small airways, such as asthma or pulmonary embolism, is most likely to develop this kind of acid-base disorder.
What is respiratory acidosis?
Example ABG: pH 7.15, PaCO2 59 mm Hg, HCO3- 22 mEq/L, and PaO2 58 mm Hg