Anything that concerns you when you walk into your patient room who is on restraints.
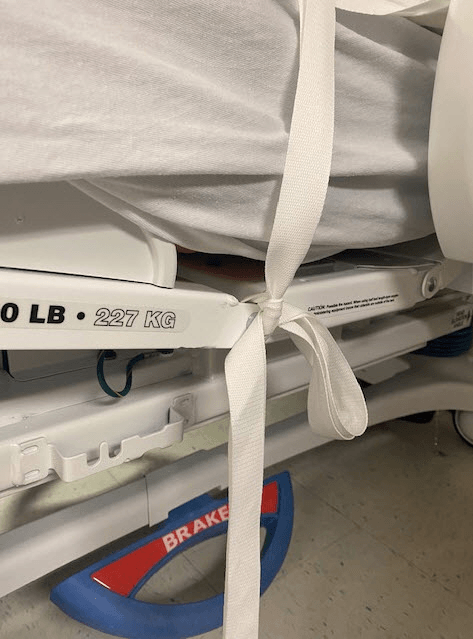
Slip knot must be tied to the hook on the bedframe. NEVER to a siderail or a joint in the bedframe.
Everyone: Demo Slip Knot on your chair.
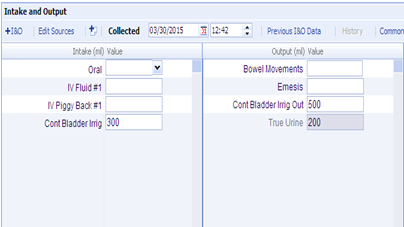
How often is Continuous Bladder irrigation monitoring and documentation of Intake and Output is required?
Every hour
•Assess for amount & color of return, absence or presence of clots, abdominal distention, patient reports of pain
•Never use a pump to regulate flow
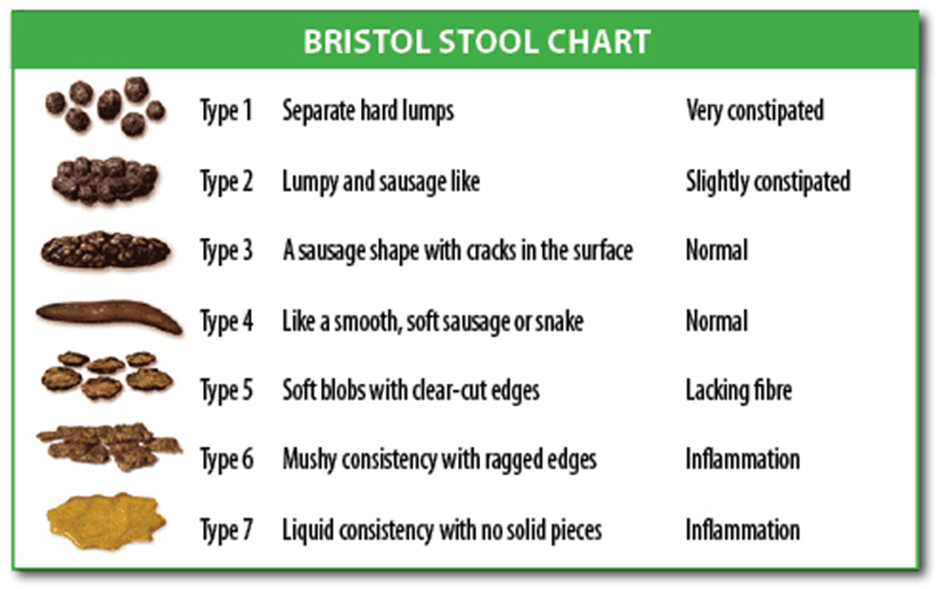
Your CNA notifies you that the patient in Bed 208 had 3 loose brown stools already this shift with strong smell. You consult the C.diff Algorithm to determine if we should consider sending the stool for C. diff. Patient has been admitted for 5 days with resolving hepatic encephalopathy. Ammonia levels & LOC are stabilizing. She is on lactulose, no prior history of C. diff.
Contact MD to discuss adjustment to lactulose and continue to monitor bowel pattern
Team BONUS: Lab will reject the sample for C. Diff unless it is what Bristol Stool type?
Patient admitted for COVID pneumonia is alert and oriented, able to ambulate to the bathroom with assistance. Patient has orders to titrate oxygen to maintain O2 levels greater than 95%. Patient is able to maintain oxygen on 4 liters NC. What nursing intervention is most important to maintain oxygen levels?
Proning.
Proning is not designed to treat complications. Proning is prevention for intubation and respiratory compromise. Even on RA, all COVID + patients are to be instructed to self prone.
Wound VAC screen shows air leak. You seal around the dressing with the VAC drape, but continues to show leak and is not reaching suction. What is the maximum amount of time that VAC therapy can be off before you need to remove the dressing and reapply?
2 hours
Patient is admitted s/p Lap Appy.
History includes: asthma and HIV +. What precautions are required for this patient?
Standard precautions.
If the patient is immunocompromised then may need reverse Isolation (Neutropenic precautions)
Patient has G-Tube feeding at rate of 100ml/hour. They are having soft BMs and abdomen is soft nontender. No c/o Nausea or vomiting. The patient had 150ml of residual. Should you stop the feeding?How often show you monitor the tube feeding tolerance and check the residual?
Continue with feeding. It is less than 250ml with no signs of intolerance. Continue to check residual every 4 hours.
If initial GRV is between 0-500 mL proceed with feeding
If GRV is greater than or equal 250 mL after a second GRV check, notify physician and recommend gastric motility agent
Hold feeding if GRV is greater than 500 mL and call physician
Note: No residual will be obtained for enteral tube with intestinal placement i.e. jejunostomy
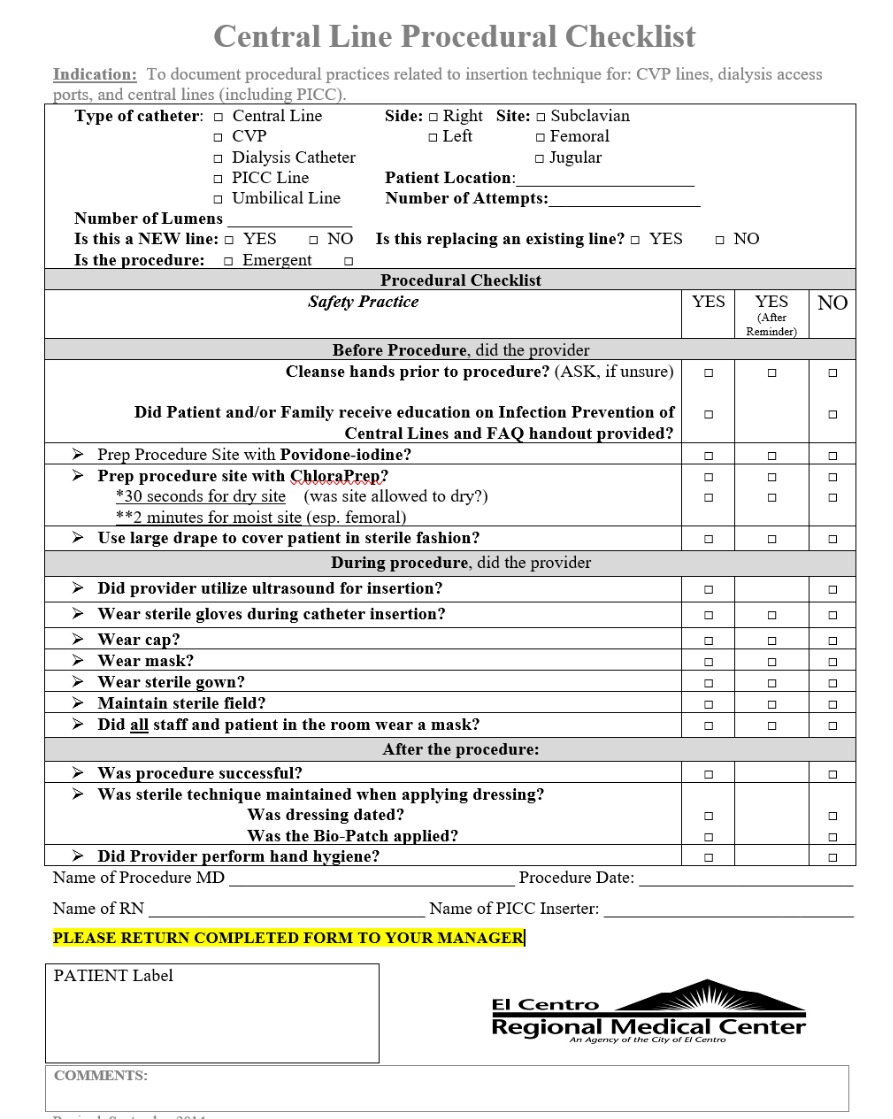
Patient renal function continue to decline. Physician decides to start dialysis. You gather the supplies for dialysis catheter placement and assist Dr. Afshar at the bedside. He completes the procedure with perfect sterile technique. What paperwork guides to your remember the technique and needs to be turned in to the charge nurse or Unit Manager?
CLIP sheet (Central Line Insertion Procedural Checklist)
Your 44 yo patient is post op day 2 s/p Lap Chole. Oxygen saturation level drops to 90% on room air. Patient has cough, but denies Shortness of breath. Breathing is irregular without retractions. Lungs diminished to the bases. You place the patient on 2L NC and the oxygen level improves to 96%. What is your next step?
Notify the physician of patient status change and obtain an order for oxygen titration. Patient teaching on Incentive spirometer.
Oxygen is a medication. Anytime a patient needs to be placed on oxygen is a change in condition. We must inform the MD to obtain an order and clarify the parameters for use of the oxygen.
BONUS: What are your differential diagnosis? Why did the patient 02 drop?
You are changing a wound VAC to the foot and notice tendon exposed. What needs to be applied in the wound bed before placing the black foam?
Adaptic (Non adherent oil emulsion) dressing. This protects the organ/delicate tissue from the black foam
BONUS ???:
Black foam should also never be in contact with ___________ skin.
You are assigned to the COVID unit. You have a patient on BiPAP, one on HighFlow oxygen, and rest on nasal cannula. You select your PAPR at the beginning of the shift. What checks are necessary prior to using the PAPR?
check the battery power & verify machine is working properly by using the Airflow Indicator
Turn PAPR on for about 1 minute prior to checking Airflow.

Your patient has a Thoracic Vent for a simple pneumothorax. The red valve is deflected downward. Patient has lungs sounds equal bilaterally. What are your care priorities for this patient & what will you discuss with the physician when they round?
Assess function of the chest tube & respiratory status. Assess area around tube for crepitus. pain management
Educate patient on Incentive Spirometer use
Discuss with MD: clamp chest tube & obtain Chest xray to determine if chest tube can be removed
TEAM TIME Bonus: How do you clamp a Thoracic Vent?
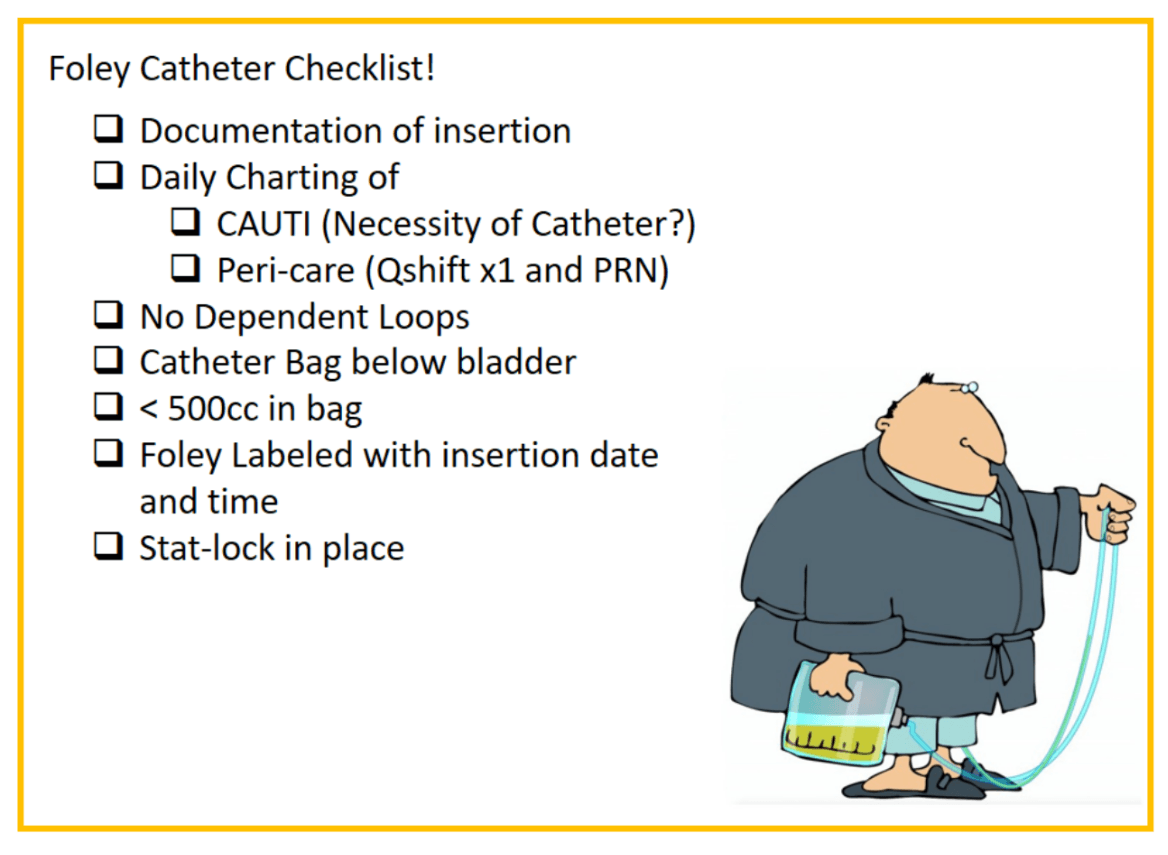
There are several measures in the ECRMC CAUTI Prevention Bundle. Name 4.
Catheter Care (use Foley wipes or Soap & Water ONLY never foam cleanser)
Foley off the Floor
Remove ASAP
in reviewing the paper post-op orders, you find the below orders. State 3 nursing interventions/ assessments required.
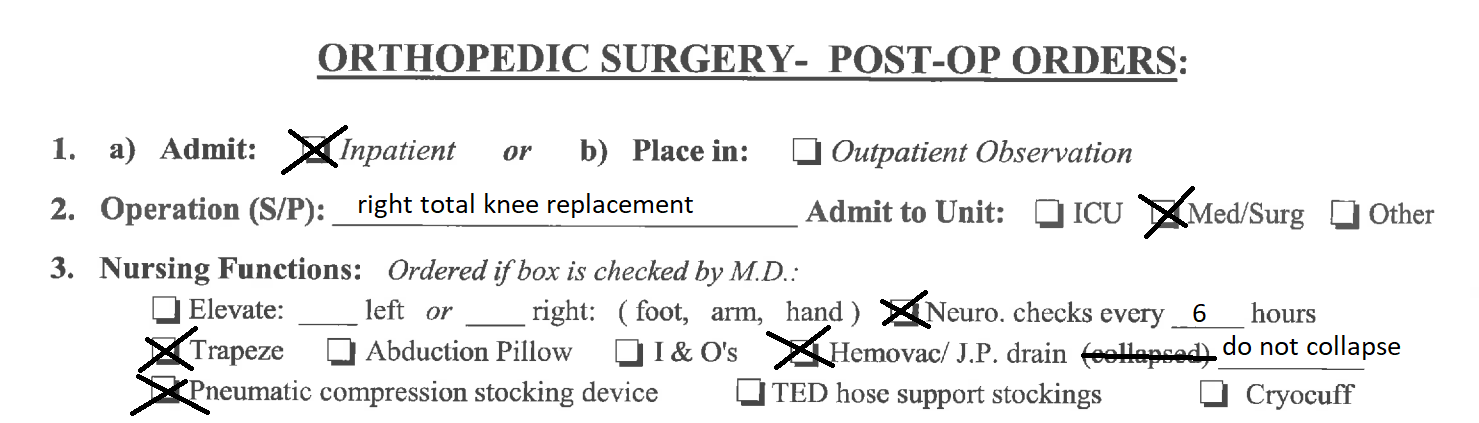
1. Neurovascular checks
2. speak to CNAs about NOT collapsing the JP
3. Ensure SCDs pump is turned on and working anytime patient is in bed.
Patient arrives to MedSurg from the ER. Upon your initial assessment, find a diabetic ulcer on the left 5th toe. You obtain a wound ruler from the supply room and write the date and patient MR # to display the perspective in the picture. Five specific pieces of information required on the wound picture that is placed in the patient's chart.
Wound labeling must include:
Patient label with name blacked out, Wound location, Date, Time, & Initials with title of RN
Example:
left foot 10/24 @ 1500, M. Mouse, RN
Today is Tuesday, 10/26. The physician orders D5 1/2 NS + 20 mEq KCL at 100ml/hour. What date/type of label do you place on the tubing so the next shift knows when it needs to be changed?
Friday IV Label (or White/Red Label and write the expiration date of 10/29)
TEAM TIME BONUS ???
Name the frequencies for the below tubing:
Vancomycin IVPB
TPN
Blood tubing
Patient has has zero output for the shift in suction cannister. Further nursing interventions required when find NGT as in picture
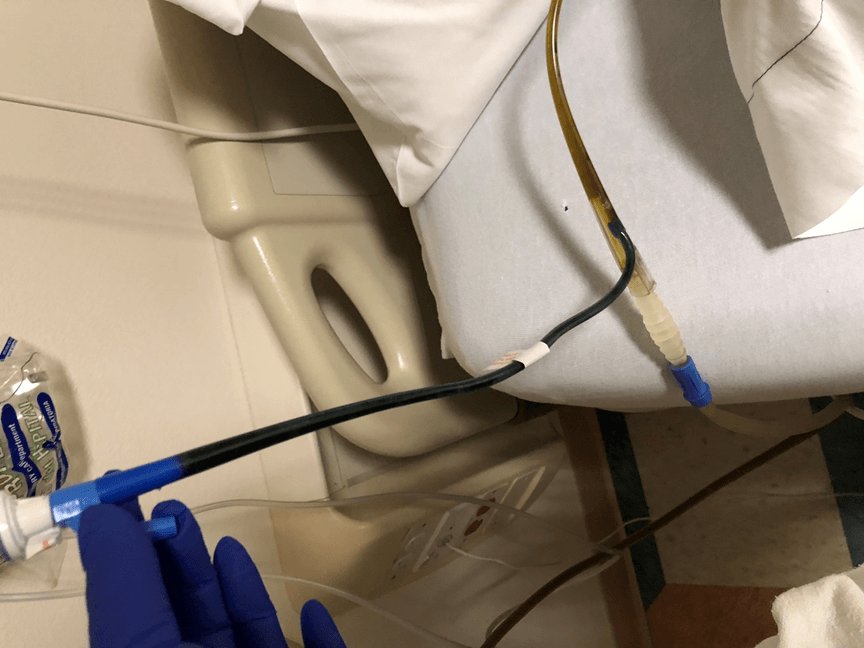
1. Verify connected to clear NGT port with 5-in-1 connector
2. Verify suction connected correctly, Suction monitor at 80. Flush blue vent with 15ml or more of air, change air vent filter if wet, Listen for whistle to confirm suction function when filter removed. Blue Vent should be placed above the level of the stomach.
3. Verify patency & placement of NGT. Tube marking still at correct place at the nose. Flush main clear port with water (unless MD order prohibits flushing tube as with s/p bowel surgery)
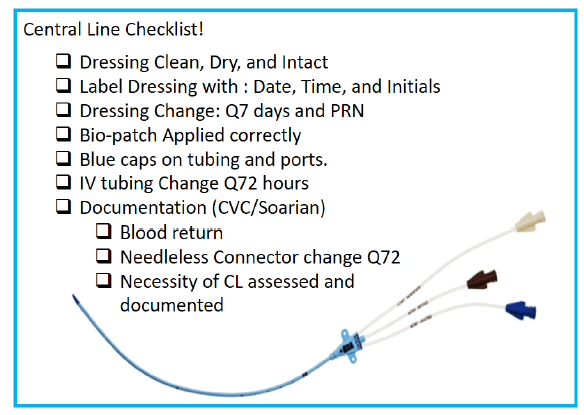
The Dialysis RN notifies you that she changed the dressing on the right jugular dialysis catheter today. You receive the patient in the room and notice that she did not put a date/time on the dressing. What are 4 measures we utilize for CLABSI prevention?
CVC & PICC Maintenance Log guides you to CLABSI prevention measures
Your patient is anxious about her dogs that she left alone at home. She doesn't have anyone to watch them, so she tells you she needs leave this morning. The patient was admitted for weakness & UTI. She still has an elevated WBC level and is on IV Antibiotics every 8 hours. You try to assist the patient but she is adamant about leaving, so you notify the physician. Physician comes to speak with the patient, but cannot convince them to stay. What documentation is required when a patient leaves AMA?
AMA form signed by the patient, nurse witness, and physician
Document DISCHARGE NOTES in Soarian including your assessment of patient neuro status
Complete MIDAS
TEAM BONUS: What will you do differently if the patient leaves before the MD can speak with them?

What is Stage 2 pressure ulcer?
Skin is intact but non-blanchable & fluid filled blisters indicate partial thickness loss of skin integrity.
if ever in doubt, ask for a second opinion to confirm your staging.
Your 55 yo patient is high risk for falls/ SAFE patient. You instruct your CNA in your beginning of shift report that the patient is alert and oriented, on Go-lytly bowel prep for a colonoscopy tomorrow,& needs assist to transfer to bedside commode
What are 5 specific fall prevention interventions that you will you reinforce to your CNA and verify are in place everytime you leave the room?
Never leave patient alone while using the commode or in the bathroom
Bed Exit, nonskid sock, yellow bracelet, frequent rounding (empty commode), hallways clear, items within reach
Patient Fall Prevention Education
Fall Care Plan
TEAM TIME!! each team will demo proper technique for manual bladder irrigation
Manual Irrigation is aseptic procedure (use new sterile kit every time)
Only input 30-50ml of NS with each irrigation
Continue until clot cleared & easy flow of urine
If unable to get urine return, reposition patient, ask pt to relax as if trying to urinate, use quick fast plunging motion with syringe. STOP... ask for assistance if fluid going in and cannot get return.
Lab posted in Soarian that your patient is positive for MRSA nares. What are the documentation requirements & nursing interventions needed?
State of CA, federal and CDC regulations all guide our management of patients positive for MRSA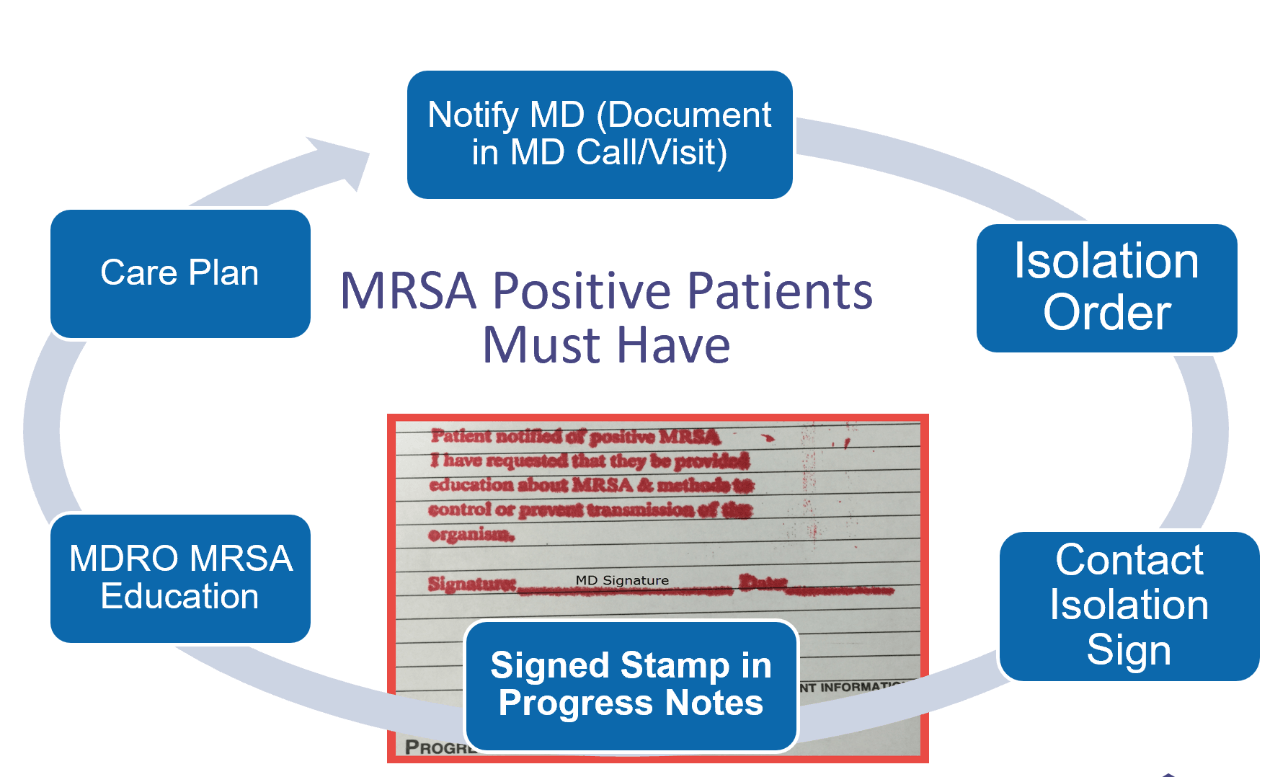
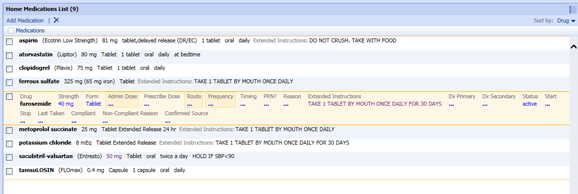
Patient admitted from the ER by the prior shift. The family brought in the list of medications, so you are completing the Home Med List. Before you save as complete what is missing from your Med Recon?
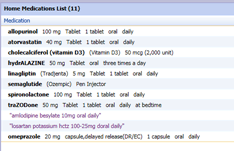
Meds did not cross over correctly with all required fields, which gives error when physician e-prescribes on D/C.
Effective 1/1/2022 CA law AB 2789 will require e-prescribing of medications unless certain exceptions apply.
Patient is post-op Day 2 for bowel resection. Wound dressing is intact but bloody strike through noted to upper part of the dressing with warmth around the insertion site. Dr. Cajas did not write instructions for dressing changes on the post op order. What is the Nursing intervention required?
Contact the physician to report the change & obtain dressing change instructions. Even if the dressing with clean dry and intact (C/D/I), ensure there is always an order that gives instructions regarding dressing changes.
Demo the SBAR call to the physician