- Protein Status
- CBC Panel
Standards
History
Which of the following would be the strongest evidence of malnutrition?
A. Visible collar bone in 26 yo female patient
B. 2+ BLE edema in CKD patient
C. Dark circles apparent in orbital region of N/V/D pt
D. Hollowing of orbital, temporal, and buccal region of dysphagia pt
D. Hollowing of orbital, temporal, and buccal region of dysphagia pt
In an acute care setting, low albumin is most likely an indicator of...
A. Malnutrition
B. Inflammation
C. Hydration Status
B. Inflammation*
*Acute phase response protein - plasma concentration increases or decreases at least 25% during inflammation, illness, and/or metabolic stress
Name one lab that would be found on a CBC panel

What is the most appropriate estimated energy needs formula for a 78 year old ventilated pt with a BMI of 31.2 kg/m2?
a. 22-25 kcal/kg
b. Modified Penn State 2010
c. Penn State 2003b
d. Mifflin St. Jour
b. Modified Penn State 2010
Used for ventilated patients that are obese (BMI > 30 kg/m2)
When assessing diet history, advantages of a 24h recall include minimal cost and short administration time. What is one disadvantage of a 24h recall?
Reliance on client memory
Potential social desirability bias
May not be reflective of usual intake
Potential inaccuracy of portion sizes
Which of the following criteria help RDs to identify malnutrition in a nutrition focused physical exam?
A. Loss of muscle mass
B. Loss of subcutaneous fat
C. Localized or generalized accumulation of fluids
D. All of the above
D. All of the above
For example, dementia patient who is a poor historian and cannot tell you their usual intake or usual body weight. We would most likely use our NFPE as evidence for malnutrition
T/F: Albumin levels will be higher with dehydration and when individuals are prescribed anabolic hormones and corticosteroids
True
i.e. Hydrocortisone, Methylprednisolone, Prednisolone
Double or Nothing: What is the risk of long term corticosteroid use?
What does CBC stand for?
Complete Blood Count
Name one estimated energy equation that is appropriate for use in pediatrics?
Schofield Equation
FAO/WHO Equation
DGAs
When assessing diet history, advantages of a food diary include little reliance on client memory and good representative of actual intake over time. What is one disadvantage of a food diary?
Low validity (underreporting is common)
Social Desirability Bias
Heavy burden on the client
You have a pt with a below-the-knee amputation (BKA). To estimate his adjusted weight in order to calculate BMI, you would divide his current weight by:
A. 70%
B. 99%
C. 81.4%
D. 92.9%
Below the knee is typically considered 6-7% (remember this is just an estimation and different for everyone)
D. 92.9%
Double or nothing: When calculating nutritional needs using a kcal/kg method, should the RD use actual body weight or adjusted/estimated body weight?
Name one somatic protein assessment lab that requires accurate 24h urine collection?
Creatine Height Index
Nitrogen Balance
How likely is it in an acute care setting that we will be able to order and accurately assess these labs for the purpose of nutrition assessment?
When iron status is low, which of the following indices would be elevated?
A. Transferrin Saturation
B. TIBC
C. Serum Iron
D. Ferritin
TIBC - Total Iron Binding Capacity
A stable, non-ICU 52 YOF patient with a BMI of 21.2 kg/m2 would likely require:
A. 25 - 30 kcal/kg and 1.5 g/kg protein per day
B. 20 - 30 kcal/kg and 0.8-1.5 g/kg protein per day
C. 30 - 35 kcal/kg and 1.6 g/kg protein per day
B. 20 - 30 kcal/kg and 0.8-1.5 g/kg protein per day
Most commonly, you will see simplistic weight based equation (kcal/kg) rather than HBE or MSJ.
What type of patient or intervention is it most likely that we would calculate EER?
What would we monitor to ensure that our EER is sufficient for the patient?
If your patient reports that he/she has nausea after eating and vomits one time per day, this type of data is considered to be:
a. objective.
b. subjective.
c. clinical.
Subjective
100pt Bonus: How would you document this information in your chart note?
T/F: The rationale for using adjusted body weight for obese pt is based on the assumption that 20-25% of fat mass is metabolically inactive. There is little to no research to support adjusted body weight calculations for estimating energy needs in obese adults.
True
May use adjusted body weight in renal due to fluid accumulation, but in an acute care setting, ideal body weight is often used when BMI > 30 because the risk of initially overfeeding the critically ill is far greater than the risk of underfeeding. Adjusted body weight has no evidence for use.
Which of the following acute phase proteins has a half life of 2 days?
A. Albumin
B. Pre-albumin
C. Transferrin
D. Retinol Binding Protein (RPB)
Pre-albumin
Pre-albumin is a more expensive test than albumin, but research has indicated that if it were used routinely during admission, approx. 44% more hospitalized pts would be identified as being at nutritional risk
An elderly patient’s lab results show:
Hemoglobin of 10.5 g/dL, MCV of 105 fL, MCHC of 33 g/dL
His family reports the patient presents w/ fatigue, irritability, and forgetfulness. A likely nutrition dx is
A. Iron Deficiency
B. Folic Acid Deficiency
C. Alzheimer's
D. Anemia of Chronic Disease
B. Folic Acid Deficiency
T/F: Protein requirements are higher in the older adult, hospitalized, and critically ill population
True
A patient is admitted to the hospital after 3 days of n/v and diarrhea and has lost 4% of his body weight. Which of the following labs are likely to be elevated?
BUN
GFR
Glucose
Calcium
Blood Urea Nitrogen (BUN)
Remember our kidneys excrete urea, and with dehydration we have less fluid to aid in excretion, causing accumulation of urea in the blood
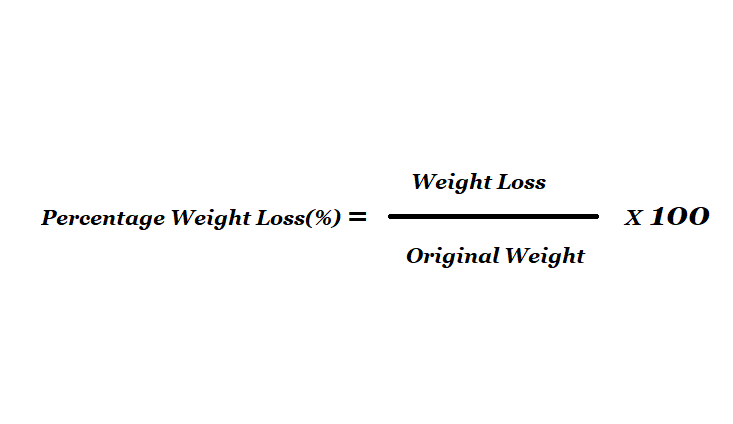
You receive a consult for the following oncology pt: 5’10” male weighing 179#, who weighed 230# one year prior. His weight loss may be classified as:
A. Mild
B. Moderate
C. Severe
C. Severe
Double or nothing: His weight loss/malnutrition is most likely in the clinical context of
A. Acute injury/illness
B. Chronic Illness
C. Social/Behavioral/Environmental Circumstances
When albumin is low (hypoalbuminemia), which of your common lab values must be corrected?
Calcium
Corrected calcium* = (4.0 gm/dL – measured serum albumin) x 0.8 + measured serum Ca
*Less accurate when the albumin is <2.5 g/dL.
A client has been diagnosed with hypochromic, microcytic anemia. Which TWO nutrients would you advise she increase in her diet?
Iron & Vitamin C
Your patient is a 42 YOM placed on the ventilator following a MVA. He is 5'9" and weighs 182#. His EMR displays temperatures since admission as 37, 38.2, 38.7, 37.9. His ventilator screen displays the following. Calculate his estimated energy needs (+/- 100 kcals) using the Penn State formula
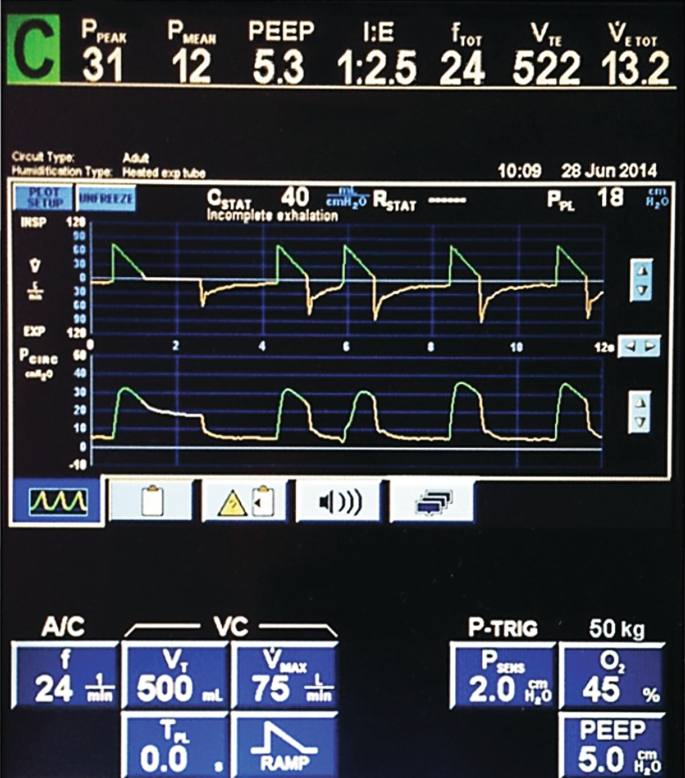
What is 2311 kcal/day
BMI = 26.9 kg/m2
Penn State 2003b:
Mifflin(0.96) + VE (31) + Tmax (167) - 6212
Mifflin = [10 x 82.7 kg] + [6.25 x 175.26] - [4.92 x 42] + 5 = 1720
1720 (0.96) + 13.2 (31) + 38.7 (167) - 6212 = 2311 kcal/day
You gain the following information for your patient's EMR regarding food and nutrition history. What are three questions you would ask the patient upon assessment?
Nutrition Screening: Poor appetite > 5 days, weight loss <10 lbs
Diet order: Adult Cardiac Diet
Allergies/Cultural Restrictions: shellfish
Documented meals since admission 48h: Dinner: 75%, Breakfast: 50%, Lunch: 50%, Dinner: 75%, Breakfast: 25%
Examples:
Can you tell me about what you would usually eat in a day before coming into the hospital?
Do you have any problems chewing or swallowing?
Have you had any recent GI issues - nausea, vomiting, diarrhea, etc?
I saw some recent weight loss in your chart note. Can you tell me about that?
Are there any foods on the menu that you particularly like or dislike? I can document those for you so we make sure you receive meals you enjoy and are eating enough to get yourself healthy!