Special Treatments
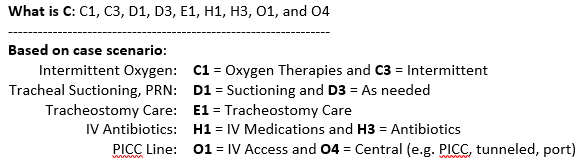
A patient is able to walk distances up to 20 feet with a walker and no human assistance.
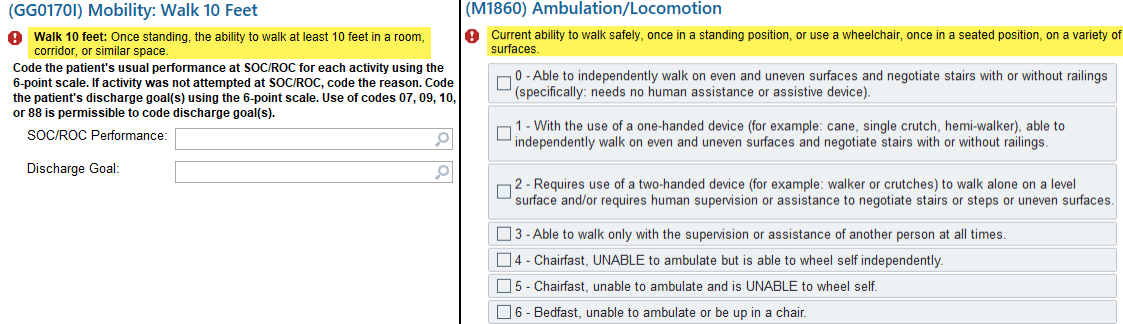
How should GG0170I – Walk 10 feet and M1860 Ambulation/Locomotion be coded? (Refer to GG Coding Handout for details)
A) GG0170I =06; M1860 =2
B) GG0170I =06; M1860 =1
C) GG0170I =04; M1860 =2
D) GG0170I =03; M1860 =3
What is A) GG0170I=06 Independent; M1860=2 Requires use of a two-handed device (for example, walker or crutches) to walk alone on a level surface and/or requires human supervision or assistance to negotiate stairs or steps or uneven surfaces.
-------------------------------------------------------
GG0170 I Coding Tip: Code based on the type and amount of assistance required to complete the walking activity, with or without the use of assistive devices or equipment.
Mr. T lives alone and sponge bathes daily. At SOC, you assess he is safe getting to the bathroom, needs standby assist to safely transfer in and out of the shower and then is able to wash his entire body safely using the handheld showerhead and bench with no need for human assist.
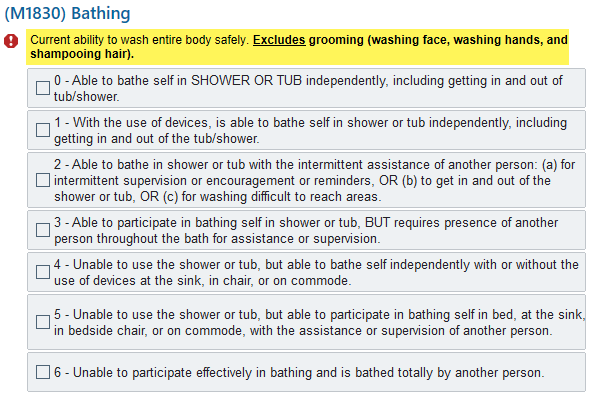
What is the correct response to M1830 Bathing?
What is 2 - Able to bathe in shower or tub with the intermittent assistance of another person: (A) For intermittent supervision or encouragement or reminders, OR (B) To get in and out of the shower or tub OR (C) For washing difficult to reach areas
--------------------------------------------------------
A135. The item addresses the patient’s ability to bathe in the shower or tub, not preference, regardless of where or how the patient currently bathes. Willingness and adherence are not the focus of the item. If assistance is needed to bathe in the shower or tub, then the level of assistance needed must be noted, and Response 2, or 3 should be selected.
In this scenario, the patient only needs assistance to get in and out of the shower = 2
How would you code M1740-Cognitive, Behavioral, and Psychiatric Symptoms, for a patient that has a hoarding disorder?
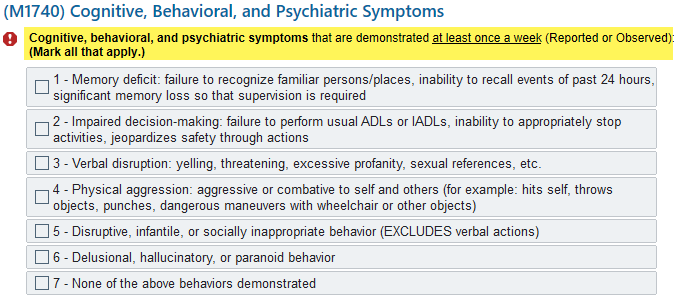
What is: Response 2 - Impaired decision-making: failure to perform usual ADLs or IADLs, inability to appropriately stop activities, jeopardizes safety through actions and/or Response 5 - Disruptive, infantile, or socially inappropriate behavior (excludes verbal actions)
-----------------------------------------------------------
M1740 - Cognitive, Behavioral, and Psychiatric Symptoms identifies specific behaviors associated with significant neurological, developmental, behavioral, or psychiatric disorders that are demonstrated at least once a week.
If the patient has a hoarding disorder, and you determined the associated behaviors resulted in concern for the patient and/or caregiver's safety or wellbeing, then it would meet the intent of M1740 and you would code the applicable items.
At SOC, the documentation reflects that the patient is taking Edoxaban and Glipizide. Per the documentation the patient has Type 2 Diabetes and is taking the Glipizide to control high blood sugar and there is no indication documented for the Edoxaban. Using Lexicomp you determine the drug classification for Edoxaban is an anticoagulant.
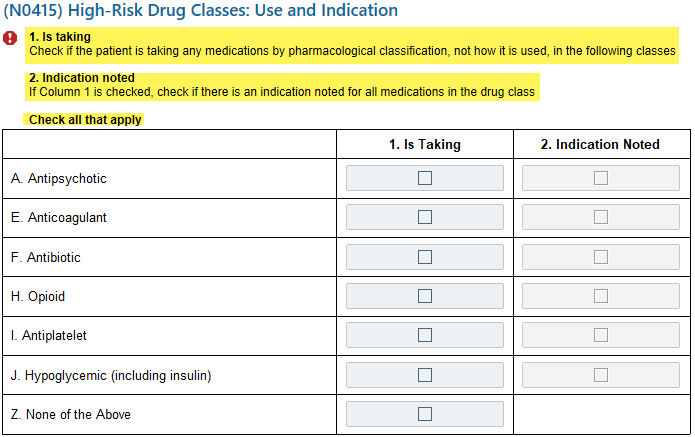
How would you code N0145?
What is: N0415 E, column 1 and N0415 J columns 1 & 2
-------------------------------------
Edoxaban: Column 1 (Is Taking) is checked as the patient is taking the medication and Column 2 (Indication Noted) is not checked as the medical record does not include an indication for why the patient is taking it
Glipizide: Column 1 (Is Taking) is checked as the patient is taking the medication and Column 2 (Indication Noted) is checked as the medical record includes an indication for why the patient is taking it (to control high blood sugar)
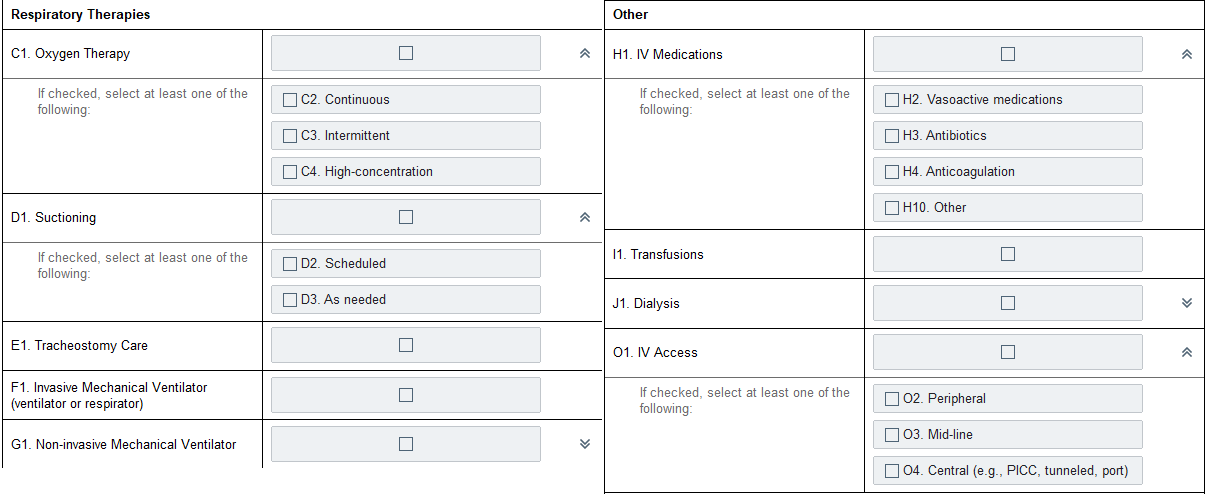
The patient’s referral information indicates that they were discharged from an acute care facility following an inpatient stay for bacterial pneumonia that required placement of a tracheostomy. At start of care, the patient requires intermittent oxygen and assistance with trach care. Their tracheal suctioning needs are PRN. The patient has orders for 1 more week of IV antibiotics, which are being delivered via a PICC line.
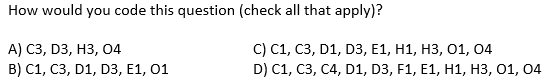
During the SOC assessment, the PT determines that even with hands-on assist and use of a walker, Mrs. Q is not safe walking. The PT orders Mrs. Q a wheelchair to use until she is stronger and can ambulate safely but the wheelchair will not be delivered for a week.
What is the correct code for M1860 Ambulation / Locomotion?
What is 5 - Chairfast, unable to ambulate and is UNABLE to wheel self.
-----------------------------------------------------
A155.3.1. A patient is considered chairfast if they cannot be made safe ambulating even with the combination of a device and the assistance of another person at all times. They are not bedfast unless they are medically restricted to the bed or cannot tolerate being out of bed. If there is no wheelchair in the home, the assessing clinician cannot make assumptions about their ability to propel it safely.
Mr. X can brush his teeth and wash his hands without assistance or set up, but requires some assistance with hair care, washing face, shaving and trimming nails.
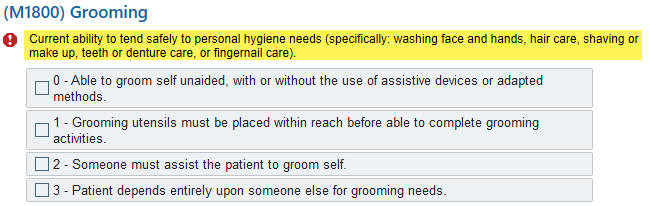
How should M1800 Grooming be coded?
What is 2 – Someone must assist the patient to groom self.
-------------------------------------------------------
In cases where a patient’s ability is different for various grooming tasks, enter the response that best describes the patient’s level of ability to perform the majority of grooming tasks.
Remember: “Assistance” in this item refers to assistance from another person by verbal cueing/reminders, supervision, and/or stand-by or hands-on assistance.
Your patient is alert and oriented, and does not use their cane because they think they do not need it (they are unsafe without it) and they decide they are not going to take their diuretic because they are going to the doctor and do not want to have an accident.
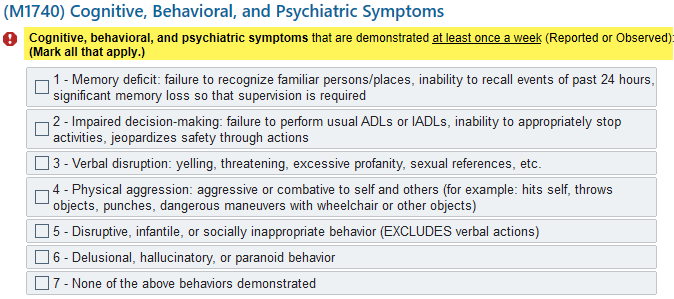
How would you code M1740?
What is 7-None of the above behaviors demonstrated
-----------------------------------------------------------
The intent of M1740, is to capture specific behaviors that are a result of significant neurological, cognitive, behavioral, developmental or psychiatric limitations or conditions. It is not the intent of M1740 to report non-adherence or risky choices made by cognitively intact patients who are free of the aforementioned conditions.
It is up to you, the assessing clinician, to determine if the patient has a disorder that is causing their non-adherence or is the patient making a choice not to comply completely with physician's orders, cognizant of the implications of that choice.
Which of the following is TRUE regarding N0415 High-Risk Drug Classes: Use and Indication?
A) Consider only medications taken by mouth (p.o.)
B) All herbal and alternative medicine products should be considered as high-risk medications
C) Medications are coded according to the therapeutic category and/or classification regardless of why the patient is taking the medication
D) Newly prescribed medications that are not yet in the home are not included
What is C: Medications are coded according to the therapeutic category and/or classification regardless of why the patient is taking the medication
-----------------------------------------
CMS Coding Tips
Include any of these high-risk medications used by any route in any setting (excluding IV flush medications)
Medications that have more than one therapeutic category and/or pharmacological classification should be coded in all categories/classifications assigned to the medication, regardless of how it is being used
Herbal and alternative medicine products are considered to be dietary supplements by the Food and Drug Administration (FDA). Therefore, they should not be counted as medications (e.g., melatonin, chamomile, valerian root) for N0415
Include newly prescribed medications that are part of the current drug regimen, even if the medication is not yet in the home and/or the first dose has not been taken
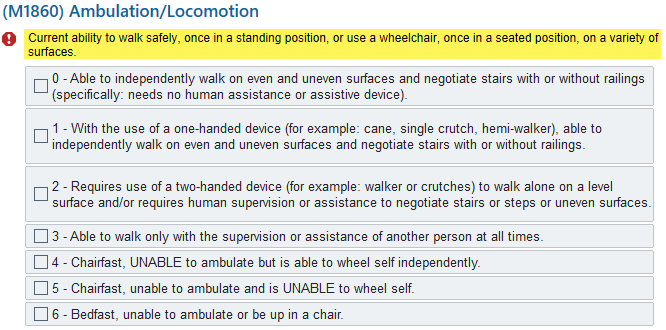
A patient has completed a course of IV antibiotics administered in the home via PICC line and is now being discharged from home health services. The PICC was discontinued one week prior to agency discharge. The patient remains on 2 liters of continuous oxygen via nasal cannula and is independent with the management of the oxygen tubing but requires assistance for the canisters when leaving the home.
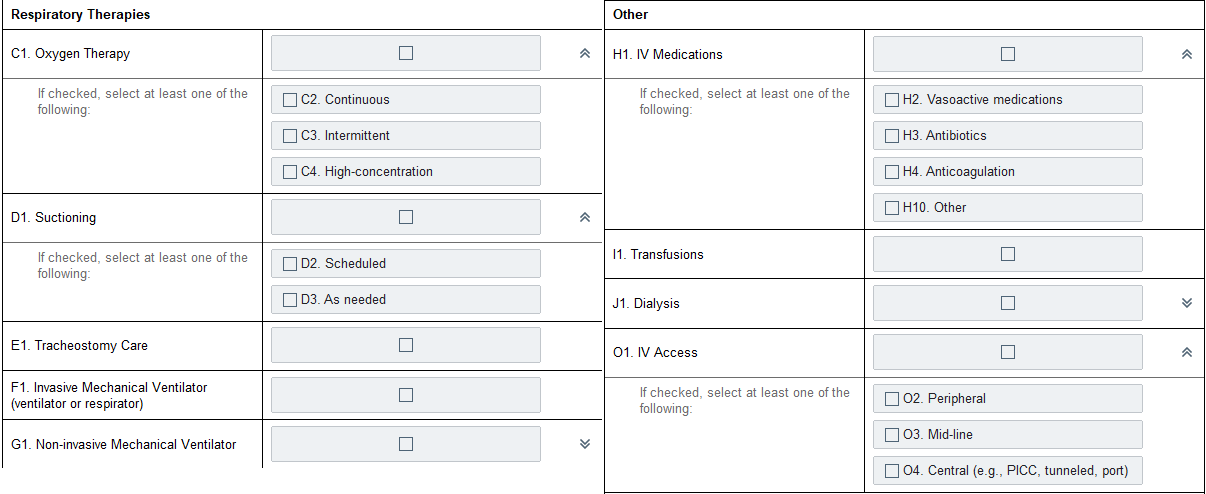
At time of discharge, how would you code O0110-Special Treatments, Procedures, and Programs (check all that apply)?
What is: C1, C2
--------------------------------------------------
Based on case scenario:
- Continuous Oxygen at 2L: C1 = Oxygen Therapies and C2 = Continuous
The Level of Ability refers to the level of assistance (if any) that the patient requires to safely complete a specified task.
Assistance includes:
A) Verbal Cues, Reminders, Supervision, Assistive Device
B) Verbal Cues, Reminders, Supervision
C) Stand by or Hands-on Assistance
D) Both B and C
What is D) Both B and C. Assistance includes verbal cues, reminders, supervision and/or stand-by or hands-on assistance.
---------------------------------------------------------
OASIS conventions defines assistance to include supervision/coaching/verbal cues and/or stand-by or hands-on assistance.
When an OASIS item refers to assistance, this means assistance from another person. Assistance is not limited to physical contact and can include necessary verbal cues and/or supervision.
Mrs. W had abdominal surgery last week and now has an open wound which requires daily dressing changes. You are completing your comprehensive assessment and note that she is wearing a housedress with slippers and no socks. She tells you that she hasn’t tried to put on her regular clothes (which she describes as her underwear, pants, shoes and socks) because she is “afraid something will break” referencing her open wound if she bends too much. You ask her if she would try to dress while you are there with her and she demonstrates that she is too afraid and uncomfortable for the mobility required to dress her lower body. The patient usually wears pants, underwear, socks and shoes with orthotic inserts.
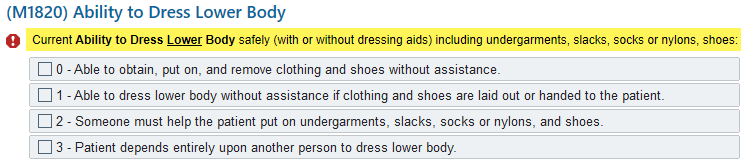
How would you code M1820 Ability to Dress Lower Body?
What is 3 – Patient depends entirely upon another person to dress lower body.
--------------------------------------------------------
Assess ability to put on whatever clothing is routinely worn.
The patient must be viewed from a holistic perspective in assessing ability to perform ADLs. Ability can be temporarily or permanently limited by:
• Physical impairments (for example, limited range of motion, impaired balance)
• Emotional / cognitive / behavioral impairments (for example, memory deficits, impaired judgment, fear)
• Sensory impairments, (for example, impaired vision or pain)
• Environmental barriers
M1745 - Frequency of Disruptive Behavior Symptoms is not completely based on behaviors identified and coded in M1740 - Cognitive, Behavioral, and Psychiatric Symptoms?
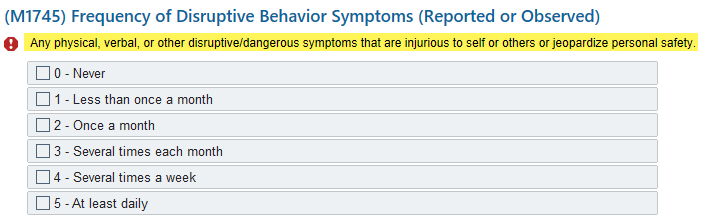
True or False?
What is: True
-----------------------------------------------------------
M1740 - Cognitive, Behavioral, and Psychiatric Symptoms, and M1745 - Frequency of Disruptive Behavior Symptoms are not directly linked to one another. There may be behaviors reported in M1740 that are not reported in M1745 and vice versa. Answer each question individually.
Example: The patient uses excessive profanity that causes considerable stress to the caregiver and is reported in M1740 (code-3). However, in the clinician's judgment, the behavior does not jeopardize the safety of the patient or caregiver, therefore it is not reported in M1745.
M1740 lists specific behaviors associated with significant neurological, developmental, behavioral or psychiatric disorders and asks if they are demonstrated by the patient at least once a week.
M1745 is not reporting on specific behaviors, but rather the frequency of any behaviors that are disruptive or dangerous to the patient or caregivers.
During the SOC, the clinician completes the drug regimen review and identifies a potential clinically significant medication issue. On that day of admission, the clinician calls and leaves a message with the physician’s office related to the medication issue. The physician does not return their call until after midnight of the next calendar day. No other medication issues arise during the episode, and the patient is discharged from home health.
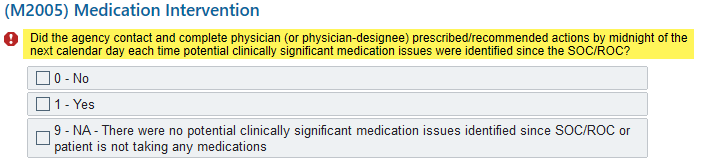
How should M2005-Medication Intervention be coded at Discharge?
A) 0- No
B) 1- Yes
C) 9- NA
D) Enter a dash (-)
What is A: 0-No
------------------------------
To complete M2005, the assessing clinician (alone or in collaboration with other agency staff) reviews the patient’s clinical record back to and including the most recent SOC/ROC, to determine if for each clinically significant medication issue identified, communication occurred AND, to the extent possible, physician/allowed practitioner (or physician-designee) prescribed or recommended actions were completed by midnight of the next calendar day
In this case scenario, the physician did not return the call by midnight the next calendar day in order for any prescribes or recommended actions to be completed.
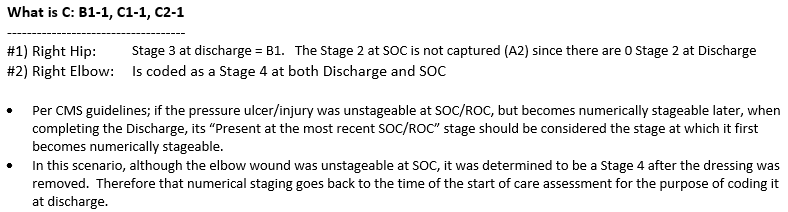
A patient is admitted to home health with referral documentation indicating the presence of a Stage 3 sacral pressure ulcer. This ulcer is covered with a non-removable dressing; and therefore, is unstageable at SOC. No other pressure ulcer/injuries are present. An order is obtained to change the dressing on Day 4 of the quality episode, and assessment reveals a Stage 3 pressure ulcer.
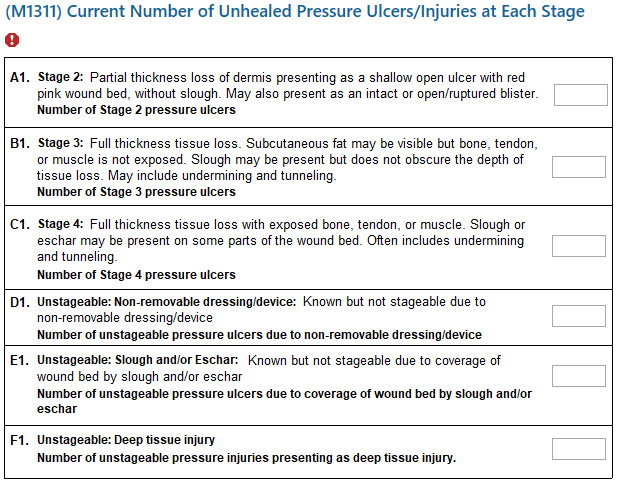
On the SOC Assessment, how should M1311-Current Number of Unhealed Pressure Ulcers/Injuries at Each Stage be coded?
A) M1311 A1 = 0, B1 =1, C1 = 0, D1 = 1, E1 = 0, F1 = 0
B) M1311 A1 = 0, B1 =0, C1 = 0, D1 = 1, E1 = 0, F1 = 0
C) M1311 A1 = 0, B1 =1, C1 = 0, D1 = 0, E1 = 1, F1 = 0
D) None of the above
What is B: M1311 A1 = 0, B1 =0, C1 = 0, D1 = 1, E1 = 0, F1 = 0
------------------------------------------------------
Although the patient has documentation indicating they have a Stage 3 pressure ulcer/injury, since we do not have orders to remove the dressing and assess the wound, D1 (unstageable, non-removable dressing/devise) is the appropriate response.
Mr. J has been referred to home care for monthly Foley changes. At his recertification visit the SN observes him sit up in bed, move to the edge, and stand safely using his walker. He reminds the nurse not to help him because "he can do this by himself." Mr. J is able to walk down the hall to the closest chair in the living room and sit in his recliner. The SN reminds him not to park his walker at the edge of the living room and to instead take it over to the chair. He reports he usually remembers to take it but is still getting used to having to walk with a device.
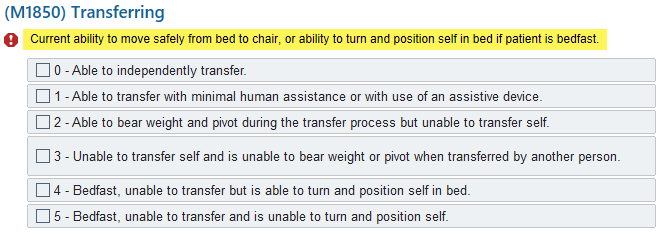
How would you code M1850 Transferring?
What is M1850=2 Able to bear weight and pivot during the transfer process but unable to transfer self.
-------------------------------------------------------
M1850-Transferring Response-Specific Instructions:
Code 2, if the patient:
- Requires both minimal human assistance AND an assistive device to transfer safely
- Can both bear weight and pivot, but requires more than minimal human assistance
Mrs. R is unable to eat or drink by mouth since she had a stroke 1 week ago. She received nutrition and fluids through a G-tube, which is administered by a helper. (Refer to GG Coding Handout for details)
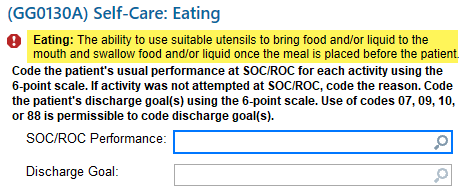
How should GG0130A – Self-Care Eating be coded?
A) GG0130A=01 Dependent
B) GG0130A=02 Substantial/Maximal assistance
C) GG0130A=09 Not applicable
D) GG0130A=88 Not attempted due to medical condition or safety concern
What is D. GG0130A=88 Not attempted due to medical condition or safety concern
----------------------------------------------------
Code 88, Not attempted due to medical condition or safety concerns, if the activity was not attempted due to medical condition or safety concerns, and the activity was completed prior to the current illness, exacerbation, or injury.
Code 09, would not be applicable, as the patient did perform this activity (Eating) prior to the current illness (CVA), exacerbation, or injury.
Since you have arrived in the home for the Start of Care visit, your patient has refused to answer any questions. They have either deferred to a family member or responded “what does it matter, just get this over with”.
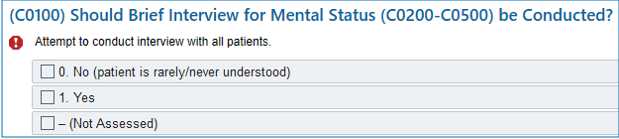
How would you code C0100-Should Brief Interview for Mental Status be Conducted?
A) 0. No
B) 1. Yes
C) Dash – (Not Assessed)
What is: B. 1 - Yes
--------------------------------------------------------
Remember; Code 1-Yes, the interview should be conducted because the patient is at least sometimes understood verbally, in writing, or using another method, and if an interpreter is needed, one is available.
When completing C0200-C0400C: Code refusals as incorrect/no answer or could not recall. If the patient chooses not to answer a particular item, accept their refusal and move on to the next question.
Mr. B, who is legally blind, has been taking 3 once daily medications p.o. each am. Recently, he was ordered to take a benzodiazepine wafer at bedtime sublingually. On the day of the assessment, he stated he had no problems taking his regular once a day medications as long as his nephew comes over on Sunday and fills his medi-planner for him which was supported by medi-planner examination. Mr. B confessed he hadn’t started his new medication for his panic attacks because he didn’t understand what the doctor meant by the word “sublingual.”
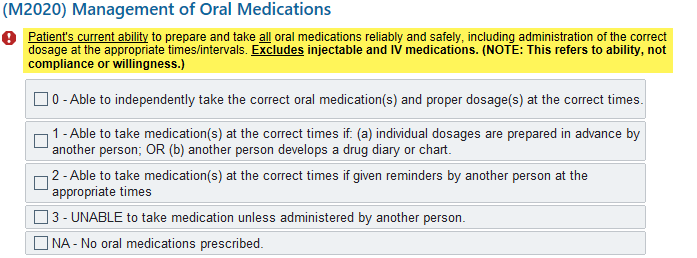
How should M2020 – Management of Oral Medications be coded?
What is 1 – Able to take medication(s) at the correct times if; (a) individual dosages are prepared in advance by another person; OR (b) another person develops a drug diary or chart
-----------------------------------------------------
CMS Response Specific Instructions:
Only medications whose route of administration is p.o. should be considered for this item. Medications are considered to be p.o. if they are placed in the mouth and swallowed, with absorption occurring through the gastrointestinal system.
Medications administered by other routes, including sublingual, buccal, swish and expectorate, or administered per gastrostomy (or other) tube are not to be considered for this item.
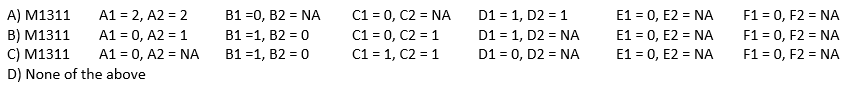
At the Discharge visit, you assess that Mrs. Richardson has two pressure ulcers: (1) Right Hip: A Stage 3 that was a Stage 2 at SOC and (2) Right Elbow: A Stage 4 which is fully granulated now
Your record review shows that at SOC, the Rt Elbow was unstageable due to a non-removable dressing. Three days after the SOC, the dressing was changed and the ulcer was observed to have 50% slough with a tendon visible.
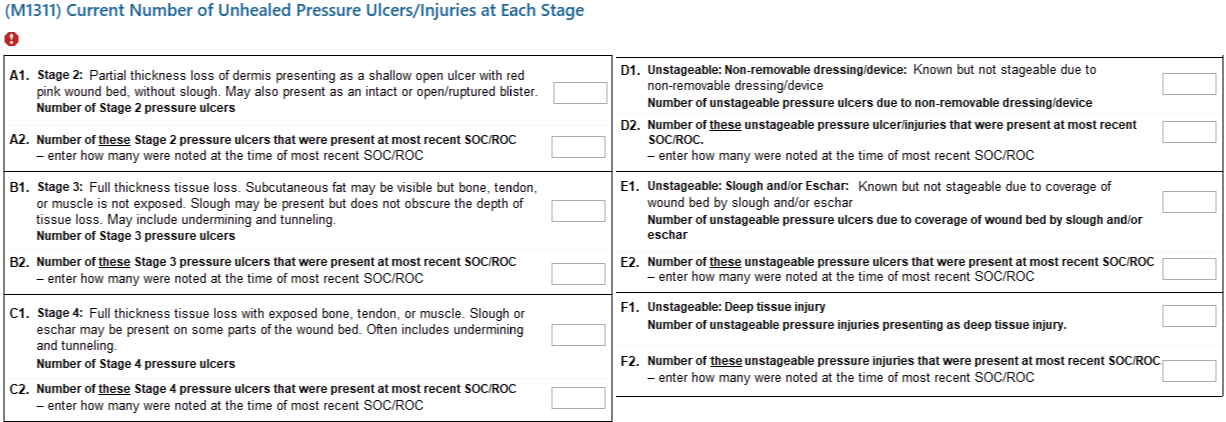
At Discharge, how do you complete M1311?
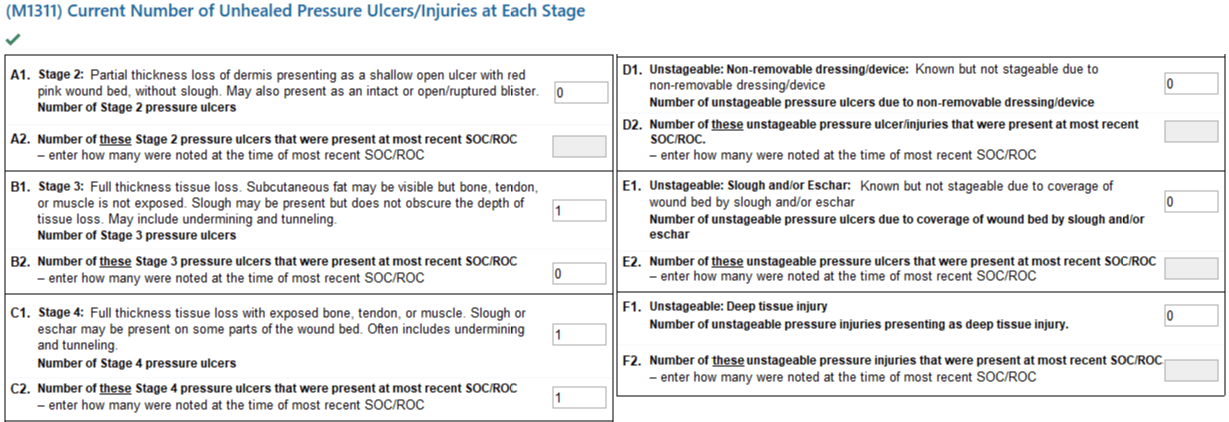
Mr. A suffered multiple vertebral fractures due to a fall off a ladder. At SOC, he requires assistance from a therapist to get from sitting to lying flat on the bed because of significant pain in his lower back. The therapist supports his trunk and lifts both legs to assist Mr. A from sitting at the side of the bed to lying flat on the bed. Mr. A assists himself a small amount by raising one leg onto the bed and bending both knees while transitioning into a lying position. (Refer to GG Coding Handout for details)
How should GG0170B-Sit to lying be coded?
A) GG0170B=04 Supervision or touching assistance
B) GG0170B=03 Partial/moderate assistance
C) GG0170B=02 Substantial/maximal assistance
D) GG0170B=01 Dependent
What is C) GG0170B=02 Substantial/maximal assistance
------------------------------------------------------
Code 02, Substantial/maximal assistance, if the helper does more than half the effort. Helper lifts or holds trunk or limbs and provides more than half the effort.
Mrs. P has urinary urgency. She requires a helper to lift her nightgown and pull down her underwear due to balance problems. After voiding, Mrs. P wipes herself and pulls her underwear back up. (Refer to GG Coding Handout for details)
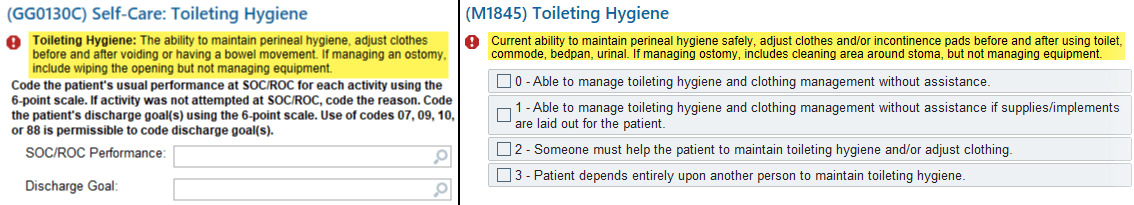
How do you code GG0130C-Toileting Hygiene and M1845 Toileting Hygiene?
A) GG0130C=05; M1845=1
B) GG0130C=04; M1845=2
C) GG0130C=03; M1845=2
D) GG0130C=02; M1845=3
What is C. GG0130C=03 Partial/moderate assistance and M1845=2-Someone must help the patient to maintain toileting hygiene and adjust clothing.
-------------------------------------------------------
Code 03, Partial/moderate assistance, if the helper does less than half the effort for the patient’s toileting hygiene.
Ms. K had a total knee replacement yesterday, and was approved by Physical Therapy to go home, 8 hours after surgery, with Home Health to start the next day.
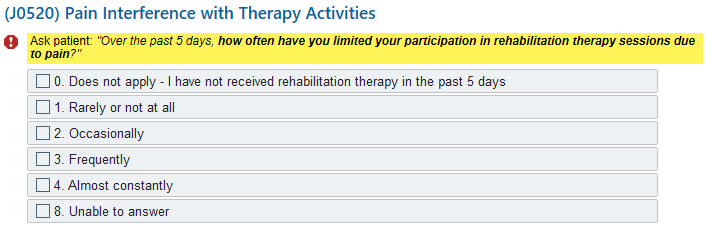
J0520 – Pain Interference with Therapy Activities, is coded as 0-Does Not Apply. True or False?
What is: False
-----------------------------------------------------------
Since the patient worked with Physical Therapy at the outpatient facility, prior to being discharged home even though it was for a short time, they have received “therapy” services in the past 5 days.
Rehabilitation therapies may include treatment supervised in person by a therapist or nurse or other staff, or the patient/family/caregivers carrying out a prescribed therapy program without agency staff present, regardless of the rehab focus or goal(s).
During your SOC assessment, Mrs. Hatfield reports that she had never been in the hospital until she fell off a curb 5 months ago and broke her ankle. She was taken to the ER and then hospitalized for surgical repair of her ankle and several days of antibiotics. In the last month, she has noticed that she can’t do what she used to every day. She tires easily and recently started napping in her chair while watching her game shows in the afternoon. Her doctor is running tests. She takes a vitamin, a laxative and an occasional over the counter pain reliever for headaches.
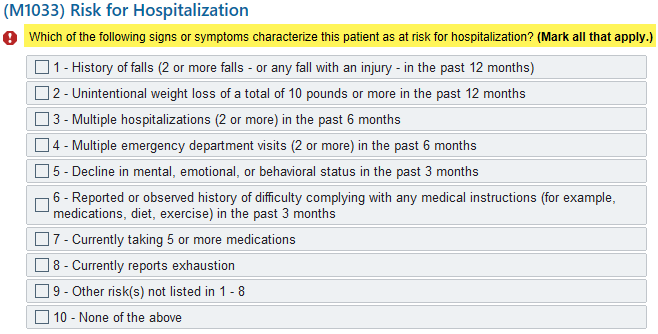
How should M1033 – Risk for Hospitalization be coded?
A) Code 1 and 8
B) Code 3 and 4
C) Code 1, 3, and 4
D) Code 3, 4, and 8
What is A: Code 1 (History of falls [2 or more falls – or any fall with injury – in the past 12 months]) and 8 (Currently reporting exhaustion)
Mr. Adams had a cholecystectomy performed via laparoscopic surgery 10 days ago and you are admitting him to home care following exacerbation of his CHF post-op. His 1 cm incision was closed with a chemical bonding agent and is assessed to be completely closed, clean and dry with no signs of infection. Additionally, Mr. Adams has an implanted Baclofen infusion pump and the puncture site where the reservoir was filled in the hospital is reddened and tender.
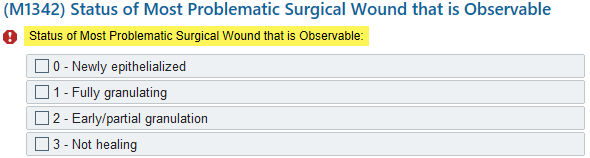
How do you complete M1342 Status of Most Problematic Surgical Wound that is Observable?
A) 0 – Newly epithelialized
B) 1 – Fully granulating
C) 2 – Early/partial granulation
D) 3 – Not healing
What is D: 3 – Not healing
------------------------------------
Primary Intention = Two edges are held together and closed with sutures, staples, steri-strips or chemical bond
Surgical wounds healing by primary intention Do Not granulate, therefore the only applicable responses are either 0-Newly Epithelized or 3-Not Healing
Note: If staples, sutures, chemical bond, etc. are still in place code 3-Not Healing