Humeral head vascularity after proximal humerus fracture better preserved if (***) mm of (***) preserved attached to the articular surface.
8 mm, Calcar (or metaphyseal extension).
Other factors: disrupted medial hinge, displaced > 10 mm, complexity of fracture, angulation > 45 degrees.
Predictors of humeral head ischemia do NOT predict humeral head AVN.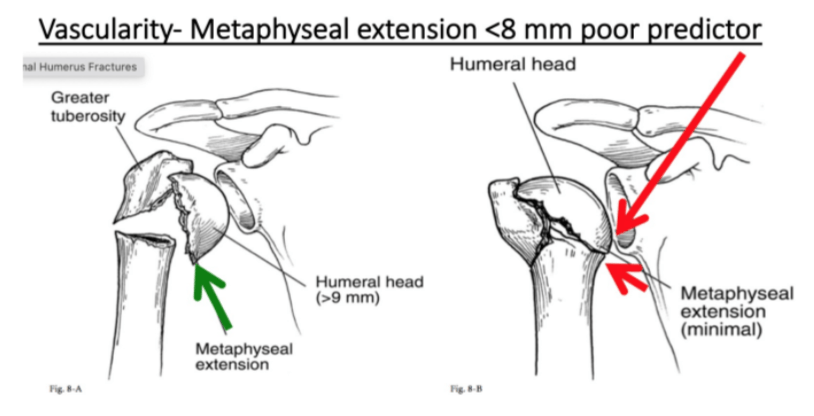
The AAOS clinical practice guideline, Treatment of Osteoarthritis of the Knee: Evidence-Based Guideline, 2nd Edition, strongly recommends which nonsurgical treatment to address knee osteoarthritis (OA)?
Tramadol
The dorsal medial nerve to the hallux can be damaged in hallux valgus surgery and is the terminal branch of this nerve.
SPN
Figures 1 and 2 are the radiograph and bone scan of a 53-year-old woman with right hip pain. She has a history of breast cancer with lymph node involvement. She completed her chemotherapy 1 year ago, at which time her staging studies were normal. The best next step is
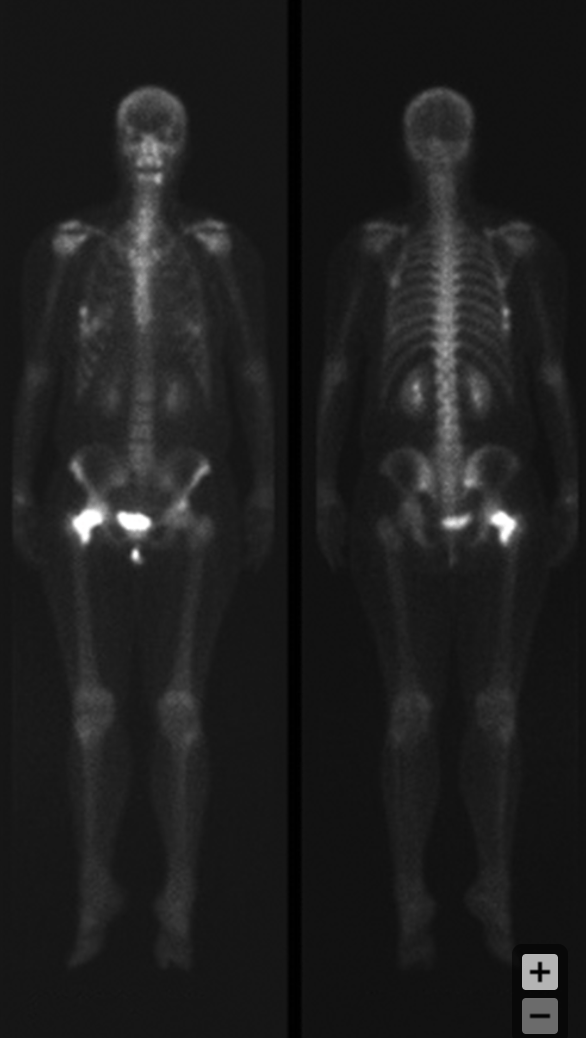
biopsy
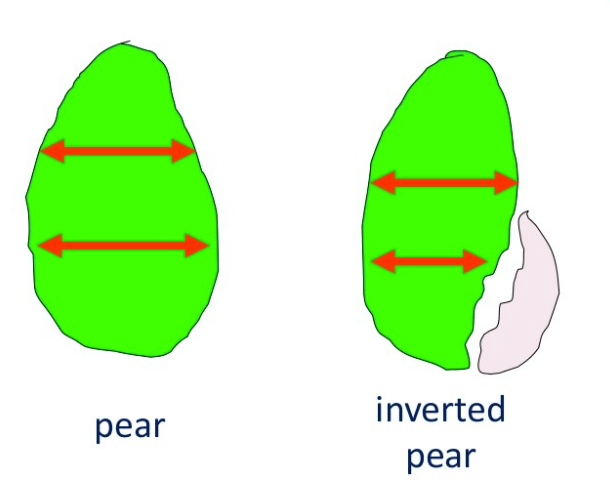
An "inverted" version of this fruit has been used to describe a glenoid that may be in need of a bony procedure.
What is a pear?
A mark of disaster in older osteopenic patients. What is this? What does it describe? And tell us why it's a harbinger of bad fixation/failure?
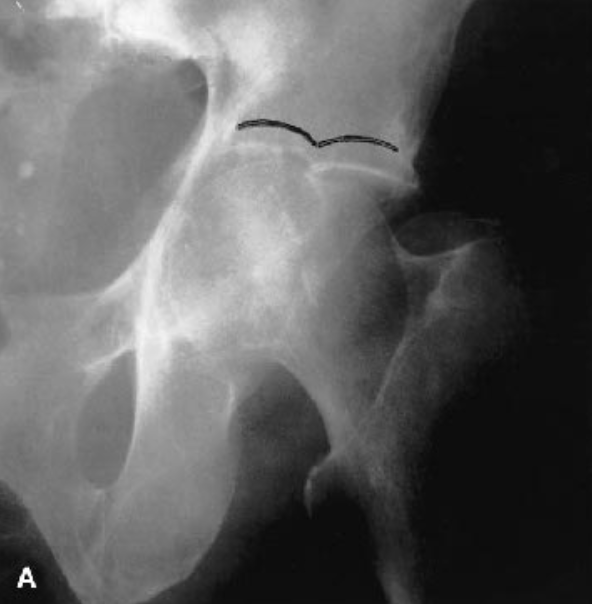
(1) Gull sign (or Seagull sign)
(2) Superomedial dome impaction
(3) Articular surface/subchondral bone gets impacted into poor cancellous bone. Hard to get reasonable reduction and KEEP IT HELD in place.
While planning acetabular cup placement and reconstruction options, how much uncoverage of a cementless acetabular cup is acceptable to prevent aseptic loosening?
30% to 40%
Talar fractures may be associated with this late-term complication, perhaps up to 100%.
PTA. 
Figures 1 through 4 are MR images of a 32-year-old man with a painless mass in his thigh. Radiographic findings are normal. He notes the mass does not bother him and he would like to avoid having surgery. The most appropriate treatment course should involve
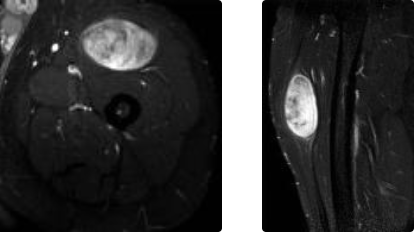
core needle biopsy
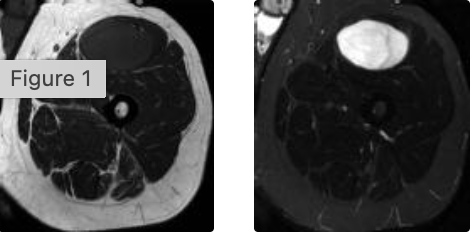
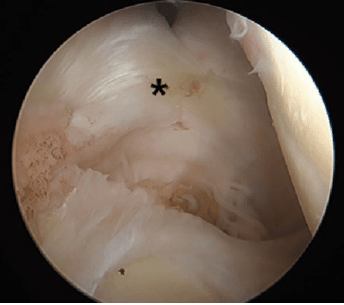
Repair of this anatomic variant, seen here from a posterior viewing portal, may result in decreased external rotation of the shoulder.
What is the Buford Complex (MGHL)?
An intertrochanteric fracture with lateral thickness less than this should NOT be treated with sliding hip screws. Further, how far distal to the vastus ridge (innominate tubercle) does one measure this wall thickness AND at what angle?
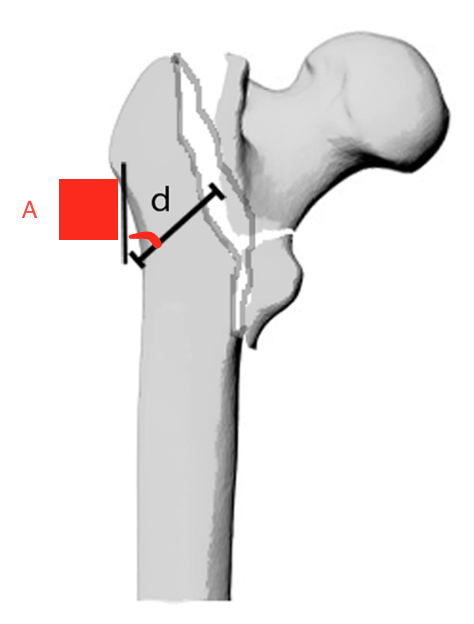
(1) 20.5 mm
(2) 3 cm
(3) 135 degrees
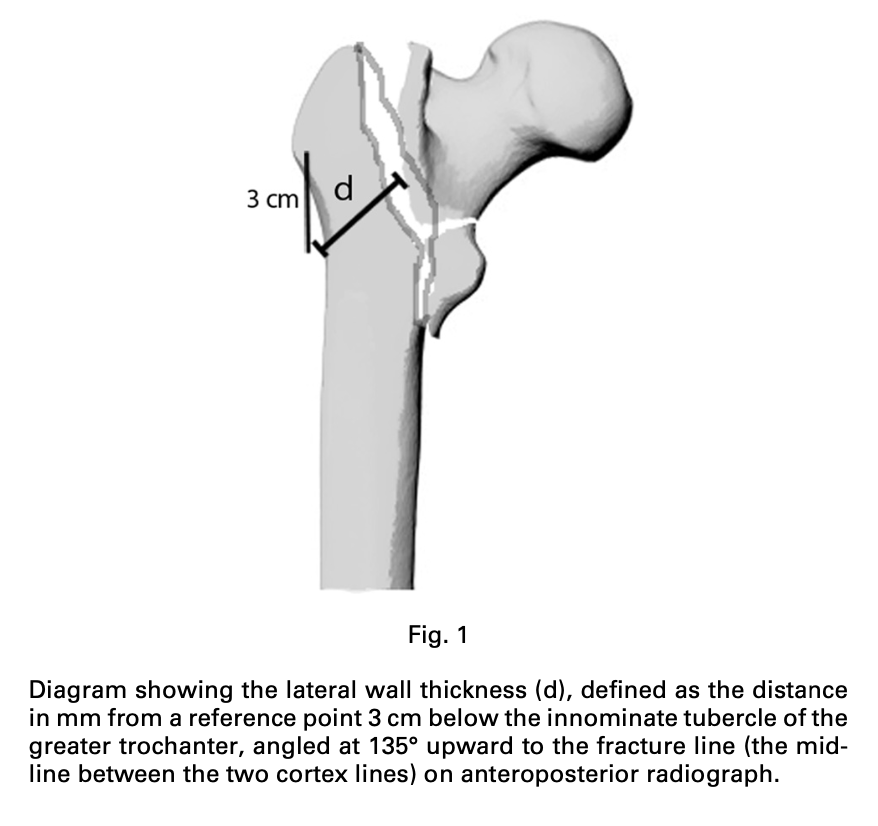
Figure 1 shows XRs obtained from a 68M who underwent left THA 6 years earlier with a titanium stem and a metal-on-poly articulation. He was asymptomatic until the previous 6 months. He denies any drainage from the hip but reports experiencing a "clunking" feeling while ambulating. His lab results are normal and the hip aspiration does not demonstrate infection. What is the most likely cause of the failure of this THA?
Trunnionosis
Ankle arthrodesis leads to compensatory increased movement at this joint, which can lead to possible degeneration and the relatively poor outcomes compared to total ankle arthroplasty.
What is the Talonavicular joint?
bonus: What patient risk factor is highly associated with TAA failure and an indication that arthrodesis is a better option?
A 32-year-old woman has a history of neurofibromatosis. She notes multiple tumors throughout her body and a recent increase in growth of a tumor in her right arm. She is experiencing worsening associated pain and tingling but denies any weakness. Which test will help determine malignant tumor transformation?
whole body PET CT
Provencher has shown that this surgical treatment option for Type 2 SLAP tears should likely be reserved for patients under the age of 36.
What is arthroscopic SLAP repair?
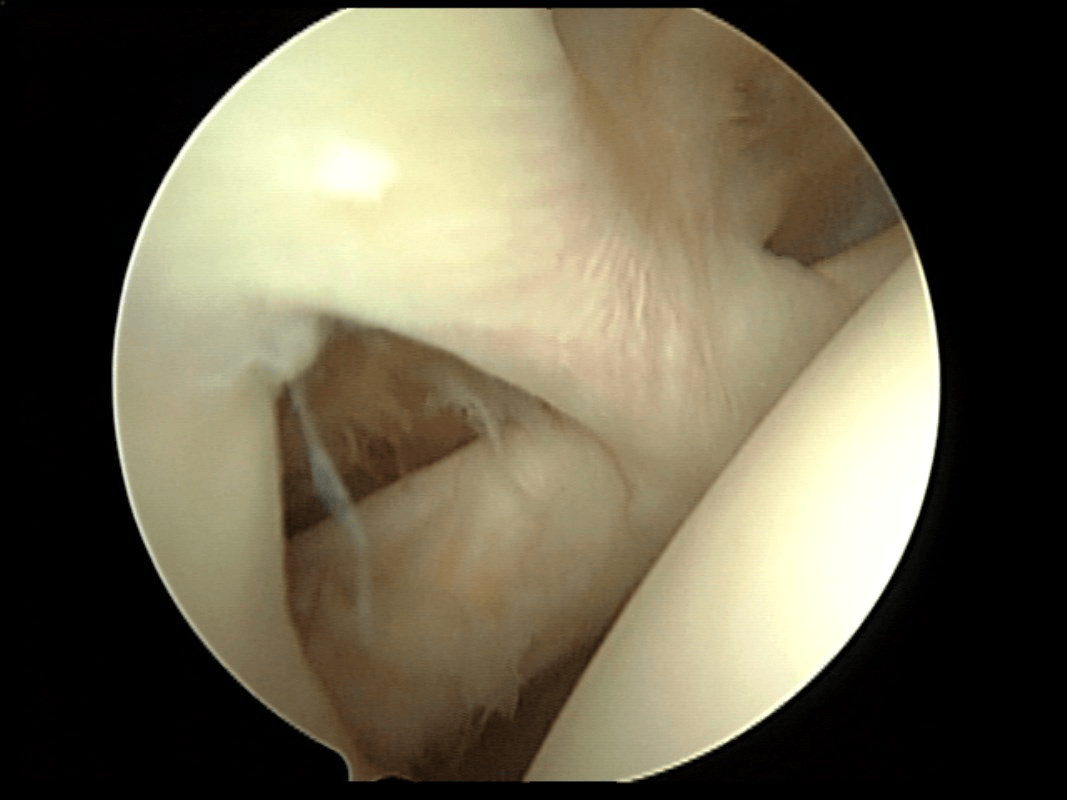
The rotational malalignment is...
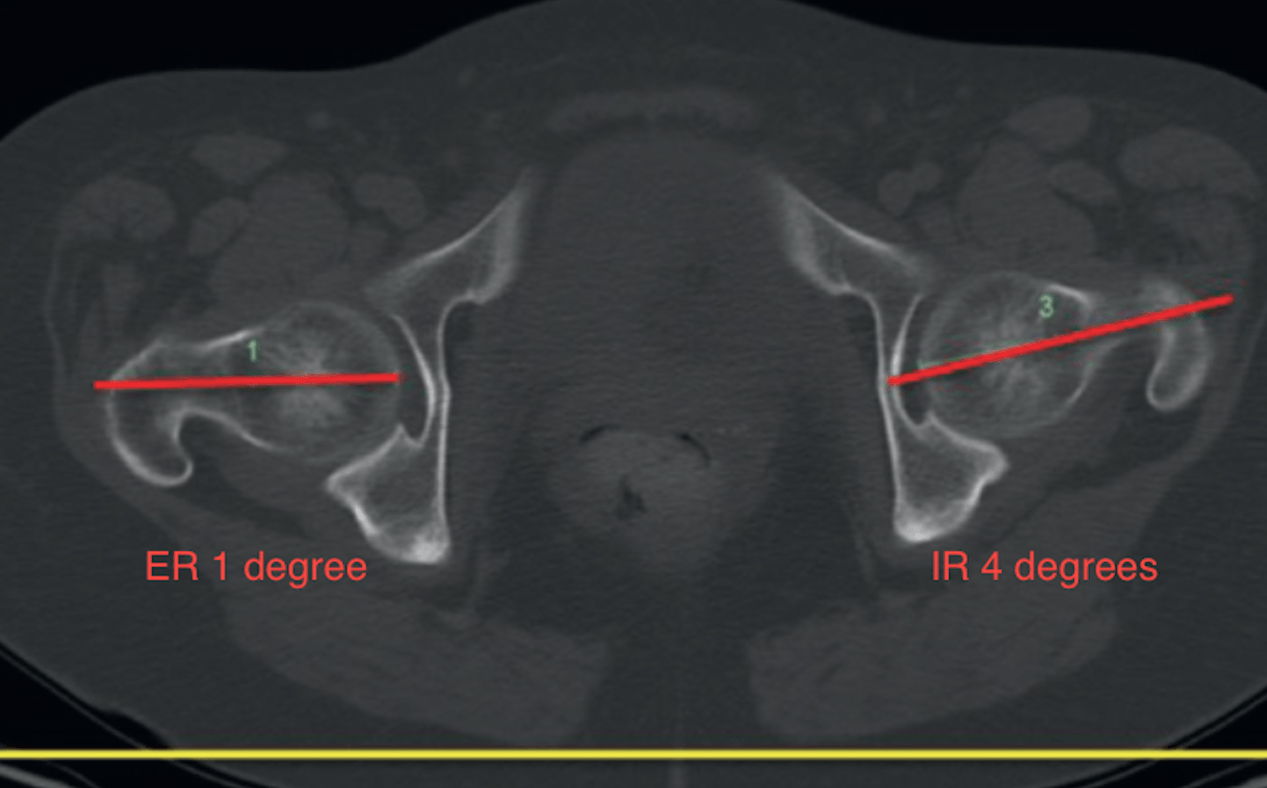
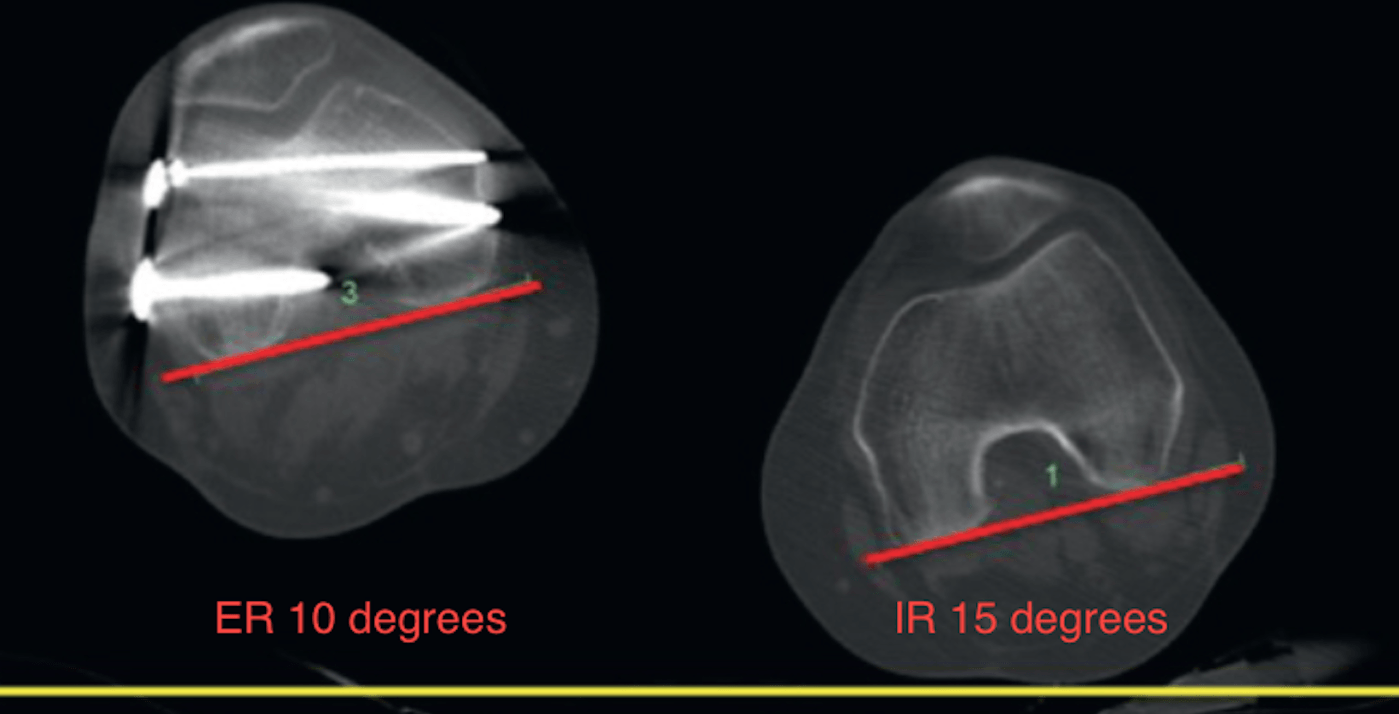
Right Side
A practical way to determine the deformity is to make the femoral neck line 0° relative to the reference line. On the right, one would need to rotate internally 1 degree. This would “remove” 1° of external rotation of the distal fragment. Therefore, the arithmetic would equate to 10° − 1° = 9° of external rotation of the RIGHT FEMUR OVERALL.
Left Side
Make the femoral neck line 0° relative to the reference line. On the left, one would need to rotate externally 4°. This would “remove” 4° of internal rotation of the distal fragment. Therefore, the arithmetic would equate to 15° − 4° = 11° of internal rotation of the LEFT FEMUR OVERALL.
RELATIVE MALALIGNMENT
In order to match the version of her right side (9 deg ER) to her normal left side (11 deg IR) one would need to internally rotate the right distal femoral segment 20° (9° + 11°).
During total knee arthroplasty with a resurfaced patella, the patella subluxates laterally during trialing. What is the most appropriate treatment?
Lateralize the femur or tibia; ER the femur or tibia; medialize the patella
AT least 3 level one studies have demonstrated that for Lisfranc injuries, the main benefit for primary arthrodesis versus ORIF is this...
ORIF group underwent more secondary surgical procedures, the vast majority of which were for the elective removal of instrumentation. Neither study demonstrated a significant difference in outcome scores, overall complication rates, or patient satisfaction.
Figures 1 through 3 are the postsurgical radiographs and biopsy specimen of an 86-year-old man who has left hip pain and a tumor in his proximal femur. Staging studies reveal a 4-mm lung nodule. He undergoes prophylactic fixation of the femur to reduce fracture risk. One month after surgery, he notes difficulty walking and continued pain. What is the most appropriate course of action?

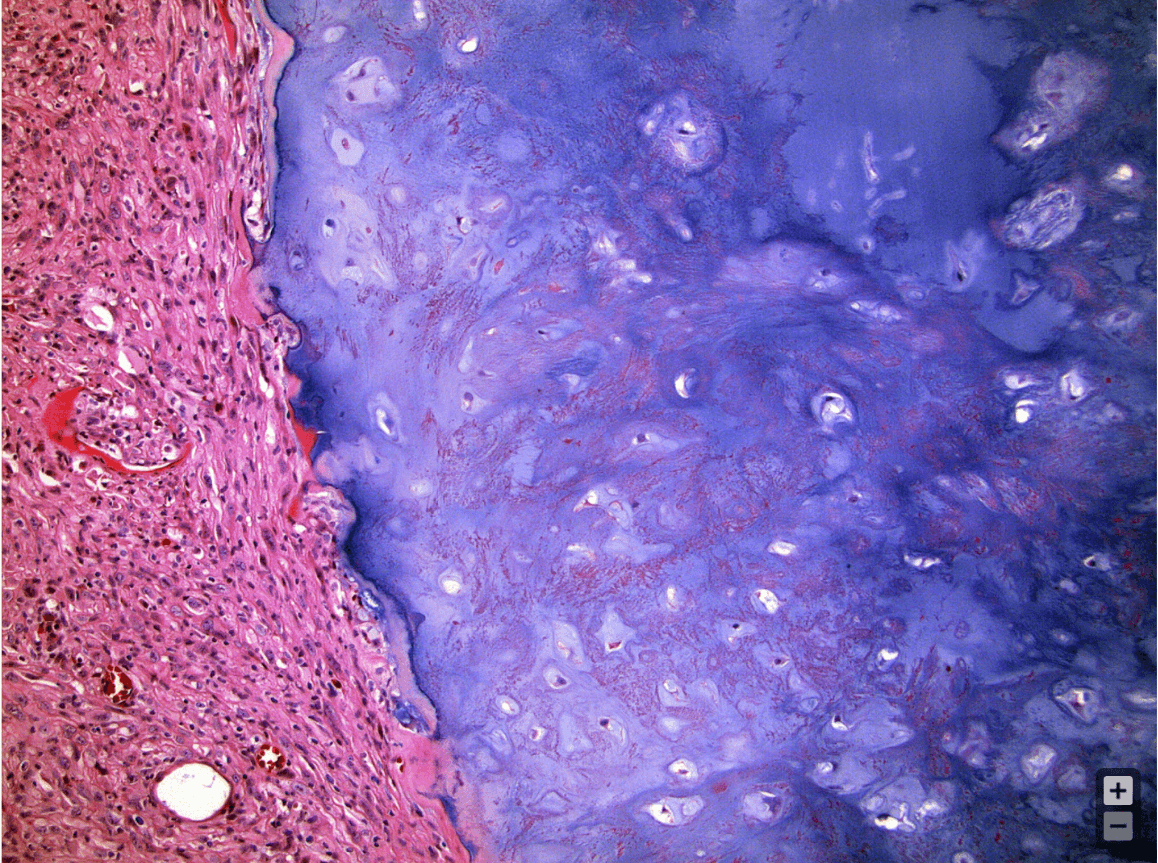
Amputation proximal to the surgical site
Pitchers with medial ulnar collateral ligament injuries in this location had a higher failure rate with non-operative management.
What are distal mUCL tears?
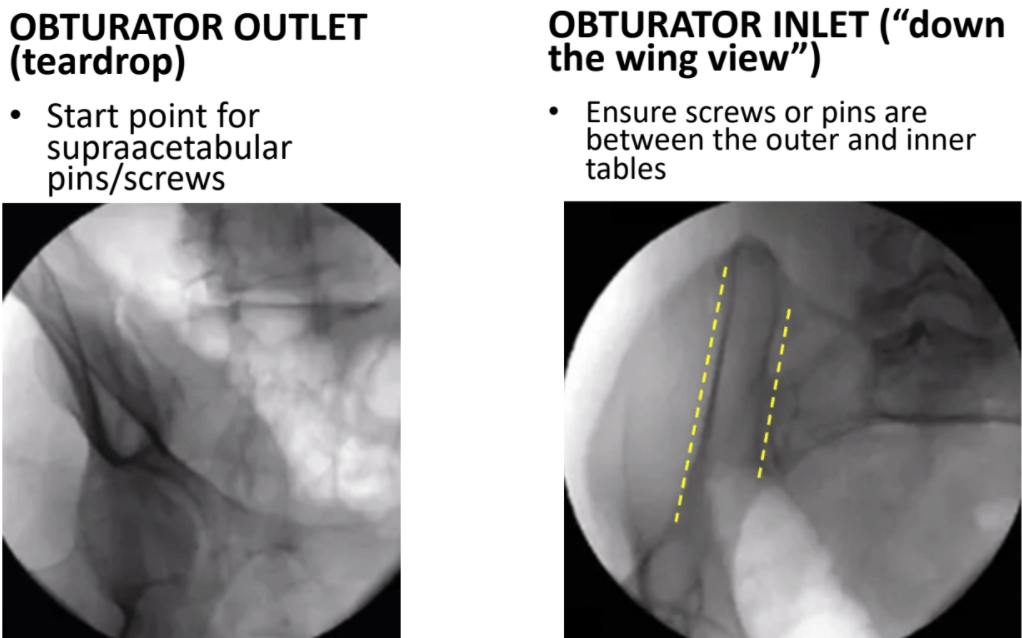
Best view for supraacetabular screw start point?
Best view to ensure screws "down the wing" or between inner & outer tables of the acetabulum?
During total hip arthroplasty, posterior instability is noted while trialing. What is the best component modification that improves stability but does not increase the joint reactive force or the length of the surgical limb?
High offset neck
What are considered moderate HVA and IMA (angles) in hallux valgus?
What is:
HVA: 25 - 40
IMA: 13 - 16
At these measurements, can consider a proximal osteotomy +/- a distal soft tissue procedure. Larger angles, think double osteotomy.
Figures 1 through 4 are the radiograph, MR image, bone scan, and biopsy specimen associated with a 42-year-old man who is experiencing right hip pain. Initial treatment should consist of
resection with a proximal femoral replacement
The comma sign, an anatomic landmark pictured here, is useful when repairing this structure.
What is the subscapularis tendon?