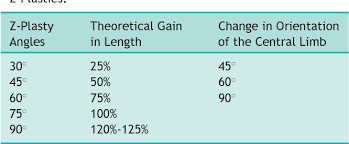
A 47-year-old woman undergoes a superficial parotidectomy for a pleomorphic adenoma. She returns to clinic 2 weeks after surgery with persistent drainage from her incision that is most notable after eating. Sialocele was diagnosed and botulinum toxin A was injected into the parotid gland. What is the mechanism of action for botulinum toxin in decreasing saliva production?
Prevents Pre-Synaptic release of Acetylcholine
Botulinum toxin is an effective treatment for sialoceles and salivary fistulae. The mechanism of action is binding the SNARE protein complex pre-synaptic neurons. This prevents acetylcholine release and inhibits salivary production in the gland.
A 61-year old female presents with bilateral, bothersome ringing tinnitus over the last 3 months. She denies aural fullness, hearing loss or vertigo. Her otoscopic exam and imaging are shown below. What is the origin of this tumor?


The tumor is of neuroendocrine origin and arises from the tympanic plexus along Jacobsen’s nerve (CN IX).
The pathology demonstrated is a paraganglioma. More specifically, it is a glomus tympanicum confined to the middle ear space. It is important to note that there is no connection to the jugular bulb, which helps to differentiate it from a glomus jugulare.
Glomus tympanicum tumors arise from Jacobsen’s plexus on the cochlear promontory (CN IX). These tumors are often associated with succinate dehydrogenase (SDH) mutation and surgical removal is recommended, particularly while they are small. Glomus tumors are very vascular tumors and the feeding vessel is the inferior tympanic branch of the ascending pharyngeal artery, which can be embolized prior to surgical removal in larger tumors
You plan to do an anterior ethmoid ligation via an external approach. Using the lacrimal crest as a landmark, where would you expect to find the anterior ethmoid artery?
24 mm posterior to the lacrimal crest

A 65 yo male presents with gradually worsening dysphonia. Videostroboscopy revealed what is shown in the image below. His pulmonary and GI workup was negative. Patient denies hemoptysis, otalgia, odynophagia, dysphagia. What is the best next step in management?

Trial of voice therapy
Vocal fold nodules by definition are opposing vocal fold lesions that resolve with voice therapy. The treatment of choice for vocal fold nodules is voice therapy.
A 56-year-old female status post vestibular schwannoma resection 12 months ago presents with House-Brackmann grade VI facial paralysis, present since surgery. Which procedure should be performed first?
Lateral tarsal strip
In flaccid facial palsy, regardless of duration, the most important structure to evaluate and manage is the cornea; the only response that addresses the eye is the tarsal strip. Patients with facial paralysis after acoustic neuroma extirpation can be at a higher risk for keratopathy due to corneal hypesthesia from trigeminal nerve involvement or injury. Additionally, irreversible muscular atrophy and fibrosis occurs after 12-18 months of denervation; axons regrow at ~1 mm/day. Reanimation techniques, like temporalis transfer, are viable options, but the primary priority remains protection of the eye.
A 43 yo woman presents with a single 2.5 cm thyroid nodule. She undergoes FNA with molecular testing which reveals a Bethesda III nodule (AUS) with a positive KRAS mutation. What is the recommended management for this patient?
Lobectomy
In a recent study of 231 patients with AUS Bethesda III result on preoperative FNA and molecular testing, isolated KRAS mutations were only associated with a 33% change of malignancy, which was much lower when compared to all other mutations
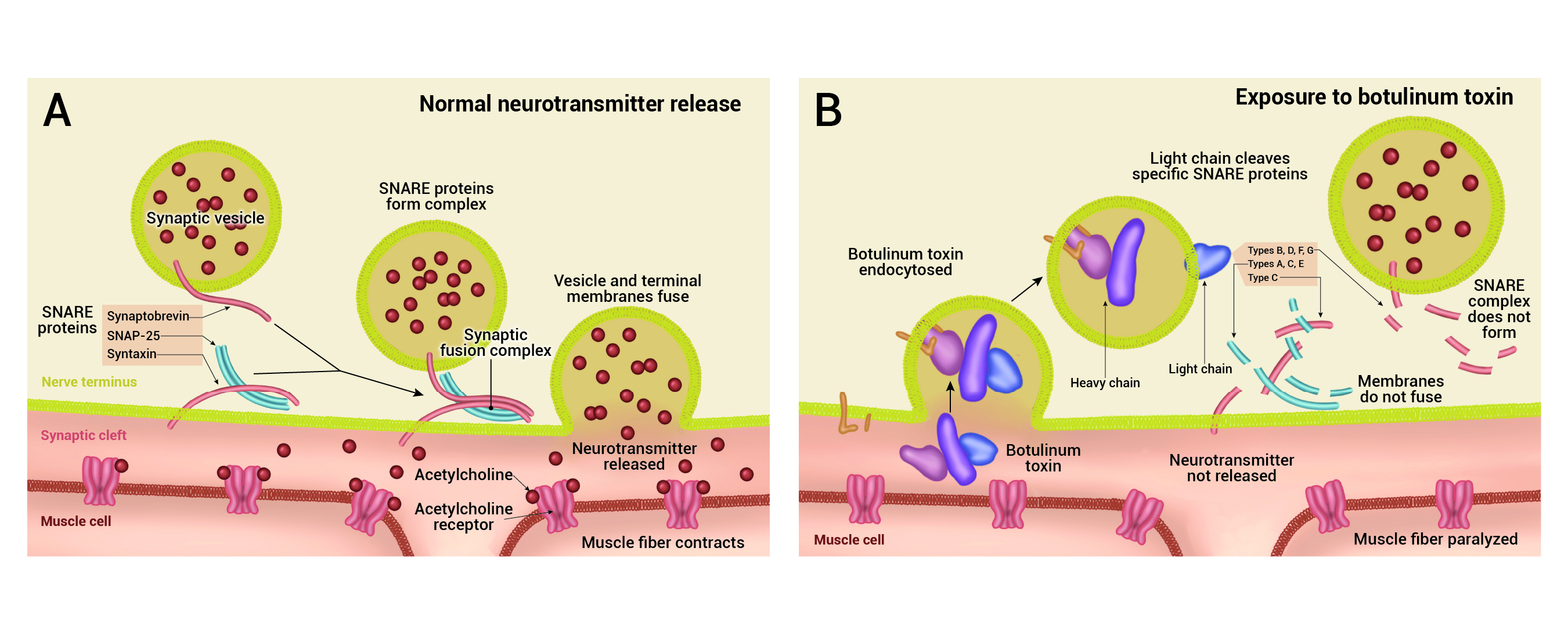
A 58 year-old female with a history of hypertension presents 5 days after sudden drop in hearing on the right (see audiogram). She has no prior otologic history. She experienced acute vertigo with the episode and was hospitalized for nausea and dehydration. During her hospitalization, she had an MRI performed. What is the best initial treatment course and work up for this patient?



Oral Corticosteroid therapy
This patient presents with an idiopathic sudden sensorineural hearing loss (SSNHL). The audiogram shows profound right SNHL and mild to moderate left SNHL, likely presbycusis. MRI of the IACs is normal. According to AAO-HNS clinical practice guidelines, MRI is a recommendation to evaluate for retrocochlear pathology and oral corticosteroids initiated within the first 2 weeks of symptom onset is an option
The guidelines recommend against laboratory evaluation and antiviral therapies. There has been little evidence to support these therapies despite the hypothesized role of viral reactivation in SSNHL and association with systemic and rheumatologic disorders. It should be noted that there is also a recommendation to use IT corticosteroid therapy as an option for salvage therapy if no response to po corticosteroids.
A Cochrane review, first pub-lished in 2006 and most recently updated in 2013, found only 3 trials that met their inclusion criteria of RCTs of steroids versus placebo or no treatment. All looked at oral steroids versus placebo, and all were found to have high-risk of bias. Two of the included trials demonstrated no significant benefit between steroids and placebo, while 1 trial showed improvement of hearing in 61% of patients in the steroid group as compared with 32% in the control group. Because of the contradictory outcomes and small number of patients in the 3 trials reviewed, the role of steroids ‘‘[remained] unclear.’’
A patient is in your office obtaining intradermal dilutional testing. The following results are seen: How would you interpret this result?

Dilution #4 is endpoint, #3 is confirmatory
The endpoint of titration is the first dilution where the wheal is at least 2 mm larger than a previous negative wheal. The confirmatory wheal comes after the endpoint wheal and is a wheal that is 2 mm larger than the endpoint wheal.
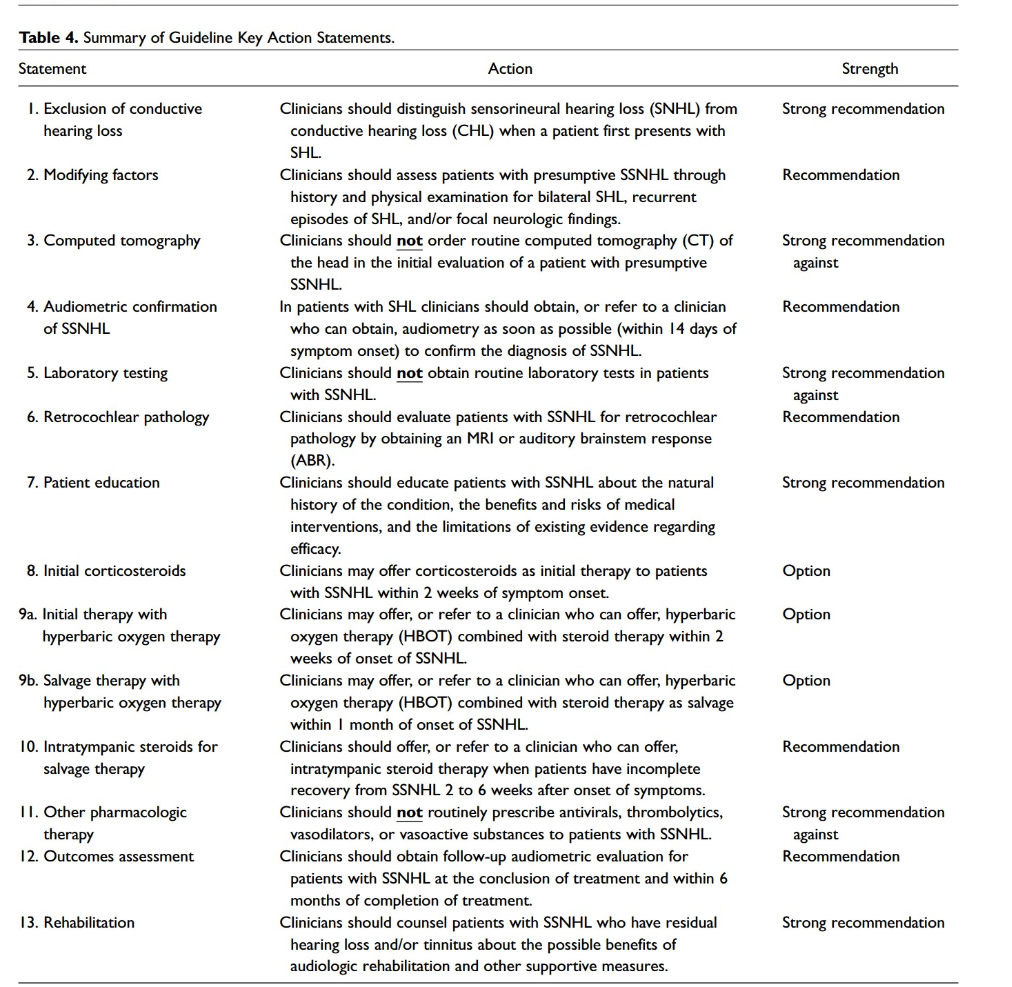
A 52 yo female presents with dysphonia characterized as lowered speaking pitch. There was no inciting event and the patient reports that her symptoms have gradually worsened over the past several years. Videostroboscopy showed the below examination. The most likely cause of the below condition is:

Smoking
Reinke's edema is the polypoid degeneration of one or both vocal folds within Reinke's space. The viscoelastic properties of the mucosal folds are characteristically altered by the edema of the subepithelial space. Most frequently, patients present with dysphonia, with women being more affected than men. The primary risk factor is cigarette smoking. Voice overuse and laryngopharyngeal reflux are also considered to be contributory.
An 11 month old, 6 kg infant presents to your operating room for cleft lip repair. How much 1% lidocaine with 1:100,000 epinephrine can be injected?
4.2ml
Maximum Dosing for lidocaine w/epinephrine is 7 mg/kg.
So: 7 mg/kg×6kg=42mg
And a 1% solution contains 10 mg/mL,
Which means that 42 mg÷10 mg/mL=4.2mL
A 32 yo man presents with an isolated 2.5 cm superficial, well circumscribed parotid mass. He undergoes an extracapsular parotidectomy. The final pathology is a low-grade acinic cell carcinoma with negative margins (closest < 2mm) and no lymphovascular or perineural invasion. What is the recommended course of action for this patient?
Observation
While the question of whether to re-excise with a superficial parotidectomy vs observe remains controversial in this setting, an aggressive approach is not warranted. Acinic cell carcinoma has a largely indolent course with minimal recurrence rate. A retrospective study of 45 pateints showed that even with close margins <1 mm there was no demonstrated benefit to locoregional control or disease free survival (in the absence of any other adverse features - advanced T category, nodal disease, lymphovascular or perineural invasion, high-grade, or positive margins).
Additionally, extracapsular dissection (ECD) of incidentally-found, low grade malignancies on final path has been shown to be an oncologically safe choice with no major increase in recurrence rates. In a study by McGurk et al of 503 patients with ECD vs 159 with superificial parotidectomy (SP) , 32 (5%) clinically benign cases were subsequently revealed as malignant histologies (ECD, 12; SP, 20). For each group, 5- and 10-year cancer-specific survival rates were 100 and 98%, respectively.
There were no differences in recurrence rates when subanalysed by surgical groups, but ECD was associated with significantly reduced morbidity (P < 0.001). This study demonstrates that ECD is a viable alternative to superficial parotidectomy for the majority of parotid tumours, associated with reduced morbidity without oncological compromise.
These data should be interpreted with caution as they are both retrospective. However, given the overall indolent nature of the disease, in the absence of adverse features, observation is the most prudent option.
An 83-year-old woman presents with bilateral sensorineural hearing loss, having worn hearing aids for over 35 years. The patient desires a cochlear implantation evaluation. Which audiologic test is most appropriate at determining cochlear implantation candidacy?
AzBio Sentence Testing
For adults in the United States, determining adult candidacy is based on sentence recognition test scores. Of the above listed options, only AzBio sentence testing are sentence recognition test scores. The remaining three options are obtained with routine audiometry, with the speech reception threshold, also known as the speech recognition threshold, is the minimum hearing level for speech at which an individual can recognize 50% of the speech material.
A 65yo male presents with gradually worsening chronic headaches. A workup including a MRI revealed what is shown in the image below. He denies any other issues aside from occasional blurry vision. What other consultations and workups will you consider?


A neurosurgical, endocrine (with full endoscrine workup) and ophthalmological evaluation for the large sellar mass and consideration of surgical resection.
The MRI reveals a contrast enhancing lesion in the sella with no other tumors. The patient likely has a pituitary macroadenoma. However, the patient will benefit from an endocrine workup to determine if the tumor is secreting. In addition, an ophthalmologic exam is useful to determine the state of the vision given that the tumor is pressing the optic chiasm. Finally, surgery should be coordinated with neurosurgery. An ophthalmological consultation and schedule for surgical resection of the tumor is incorrect as an endocrine and neurosurgical consultation will benefit the patient.
A 26 yo male presented with 6 weeks of progressive dysphonia. Patient does not have a history of smoking. Denies dysphagia, odynophagia. Videostroboscopy revealed the following. The most common cause of this pathology is:

Human Papilloma virus 6 and 11 are the most common subtypes of human papilloma virus that cause recurrent respiratory papillomatosis seen in the image above.
Which structure is most likely to be injured during rhytidectomy?
The Great Auricular Nerve
The great auricular nerve is the most commonly injured nerve in rhytidectomy, occurring in 6-7% of cases. It lies 1-2 cm posterior to the external jugular vein. The most commonly injured facial nerve branch in facial rejuvenation is the marginal mandibular branch; frontal branch injury is also described, but tends to occur along with zygomatic and occasionally buccal branch injury.

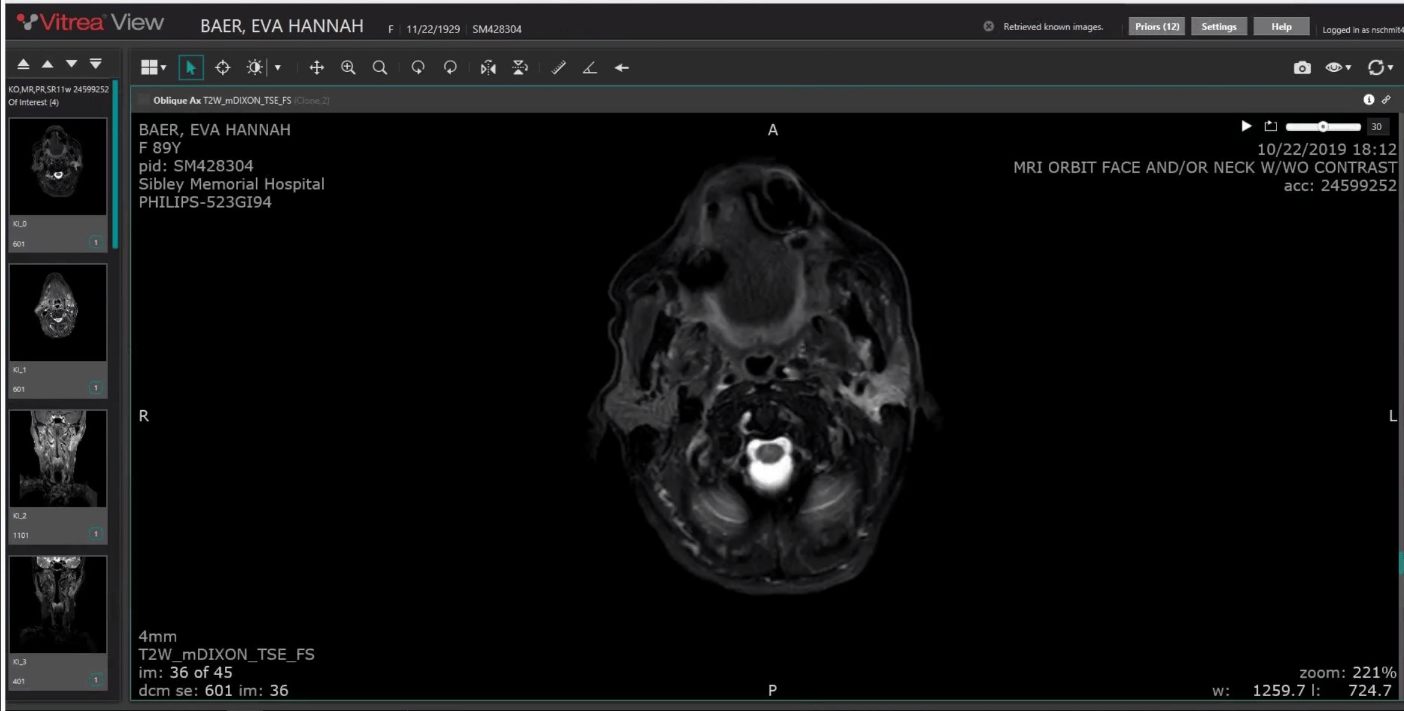
57 yo patient presents with a 3.5 cm parotid mass that appears to be growing outside the capsule on imaging, but no evidence of lymph node metastases. Preoperative FNA reveals an adenoid cystic carcinoma. What is the recommended treatment plan for this patient?
Parotidectomy + Neck Dissection + Adjuvant Radiotherapy
Elective Neck dissection has been associated with significantly extended overall survival in patients with advanced (T3-T4) ACC of the major salivary glands when compared with those who had resection alone. There is a significantly increased risk of occult nodal metastasis among patients with clinically negative nodal disease of the major salivary glands in this group.
US National Comprehensive Cancer Network guidelines have suggested that adjuvant radiotherapy should be offered to patients with risk factors for recurrence such as intermediate or high-grade tumors, close or positive margins, perineural invasion, lymph node metastases, lymphovascular invasion, and T3-4 tumors.
65-year-old woman presents with a known right internal auditory canal mass. The following audiogram is obtained below. After discussion observation was decided as management plan. What is most accurate about counseling the patient regarding the prognosis of her hearing loss?

Increased chance that her hearing will continue to deteriorate
Hunter et al. sought to characterize the risk of progression to non-serviceable hearing in patients with sporadic vestibular schwannomas who elected observation at the time of diagnosis. They found that each 10-dB increase in pure-tone averages at diagnosis is associated with a 2-fold increased likelihood of developing non-serviceable hearing.
After endoscopic transsphenoidal hypophysectomy for a large pituitary macroadenoma. Assuming the olfactory cleft was not injured, what reconstruction method of the sellar defect is most frequently associated with prolonged olfactory disturbance?
Reconstruction with a nasoseptal flap that was harvested with electrocautery
There are several ways to reconstruct the sellar defect following a transsphenoidal hypophysectomy. Some techniques will utilize a free mucosal graft or synthetic graft, Others will use a nasoseptal flap. However, one study have shown consistent olfactory impairment with the use of a nasoseptal flap. The flap has shown to worsen hyposmia for at least 6 months after surgery.
A 78 yo diabetic male presented to the laryngologist with a 3 week history of worsening solid food dysphagia. Patient denied any abdominal discomfort or weight loss. Patient reports that his blood sugar readings have been “high” over the past year. In-office transnasal esophagoscopy which revealed the findings below. The most likely cause of the below diagnosis is?

The most common causative organism for candida esophagitis is Candida albicans, Candida glabrata, and .Candida tropicalis
What are the Major Nasal Tip Supports? (3)
Major tip supports:
1. Size, shape, resilience of lower lateral cartilages
2. Attachment of lower lateral cartilages to upper lateral cartilages (scroll region)
3. Attachment of lower lateral cartilages to caudal septum
Minor tip supports:
Interdomal ligaments
Sesamoid cartilages
Skin-soft tissue envelope
Membranous septum
Dorsal quadrangular cartilage
Nasal spine
A 90-year-old woman presents with a several-week history of a firm, painless left parotid mass. MRI demonstrates an enhancing nodularity of nearly the entire parotid gland, and fine needle aspiration biopsy yields oncocytic cells. What is the most likely diagnosis?
Nodular oncocytosis of the parotid gland, also know as nodular oncocytic hyperplasia
Rare, benign condition seen most often in elderly patients. It is often confused with benign oncocytoma or oncocytic carcinoma. Fortunately, it does not progress to malignancy, therefore surgery is not usually required. However, the diagnosis is often made after parotidectomy to rule out neoplasm.
A 10-year-old boy is referred for unilateral hearing loss and the following imaging findings. He is otherwise asymptomatic without otorrhea and his otoscopic exam is unremarkable. How would you counsel his parents regarding hearing outcomes after surgery?

Hearing outcomes are comparable between single stage and two-stage ossicular chain reconstruction.
Mean pure-tone averages are 30db after canal wall up procedures compared to 45db for canal wall down procedures.
Recidivism rates are higher after canal wall up procedures for cholesteatoma compared to canal wall down procedures. The increased visualization afforded by removal of the canal wall decreases recidivism from 16-61% to 0-13%. The addition of adjunctive techniques, such as the use of endoscopes may reduce this rate further.
A 65yo male presents with gradually worsening chronic headaches. A workup including a MRI revealed what is shown in the image below. His endocrine and ophthalmologic workup was negative. Your neurosurgical colleague would like to proceed with a transsphenoidal hypophysectomy. The neurosurgeon notes that he will have to dissect in the lateral and superior aspects of the tumor. What potential cranial neuropathies (3) may arise from the surgical excision?


Potential Injuries to CN4,5,6
The patient may develop blindness and diplopia
The MRI reveals a contrast enhancing lesion in the sella with no other tumors. The patient likely has a pituitary macroadenoma. Given that the tumor is in the cavernous sinus and pushing on the optic chiasm, potential injuries to the cranial nerves (4, 5, 6) in the cavernous sinus in addition to the optic nerve may occur. It is less likely that the lower cranial nerves (7, 9, 10, 12) are injured due to the location of the tumor.
A 31-year-old woman presents with arthritis and swelling of the hands and evidence of bilateral cricoarytenoid joint ankylosis on laryngoscopy. Which serologic test is most specific for this patient’s systemic disorder?
Anti-cyclic citrullinated peptide (anti-CCP)
This patient’s systemic symptoms suggest rheumatoid arthritis. Rheumatoid arthritis can present as bilateral joint ankylosis in the larynx but can also present as bamboo nodules or erythema and inflammation. In this case, testing must include RF and anti-CCP antibodies. Anti-CCP is considered more specific.
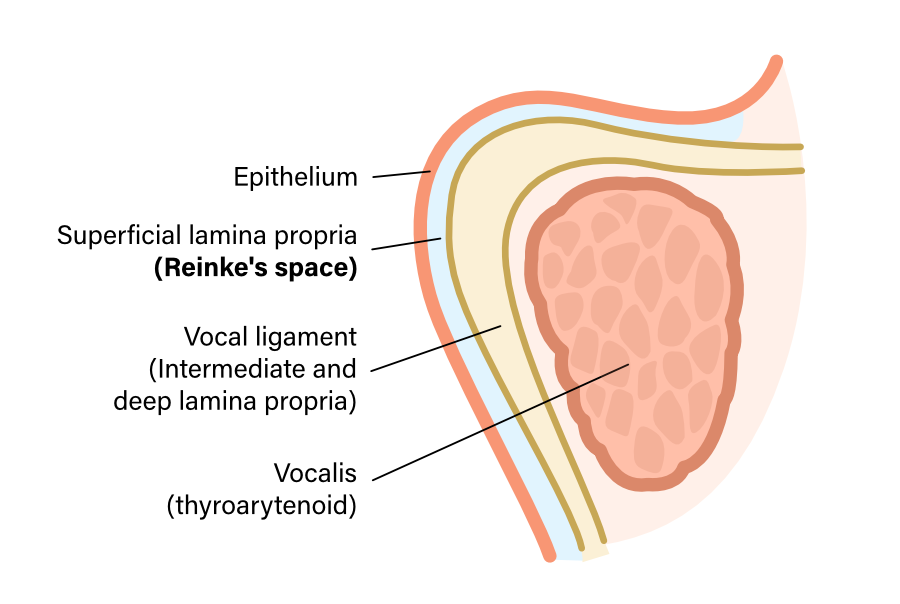
What will occur to the length and rotation of the scar in the following picture?

Lengthen by 75% and rotate by 90 degrees