True or False: Oxygen Tanks are heavy. You can transport by rolling, dragging, or sliding.
False
Nasal Cannula: What size tubing (small or large bore), how many liters/min can it accommodate, and what oxygen requirements is it best for?
small bore tubing
2-6L/min (greater than 6L/min the patient swallows air and FiO2 level does not increase)
best for minimal oxygen requirements
>4L/min
What are you noting in your oxygenation assessment of the skin & mucous membranes?
Color. Note whether cyanosis is present, presence of mucus, sputum production, and impedance of airflow.
What can result from shallow respirations?
inhibit both diaphragmatic excursion and lung distensibility. The result of inadequate chest expansion is pooling of respiratory secretions, which ultimately harbor microorganisms and promote infection. Additionally, shallow respirations may potentiate alveolar collapse, which may cause decreased diffusion of gases and subsequent hypoxemia.
How do you store oxygen tanks?
Upright, secured in a carrier or stand. Out of traffic areas
Simple Face Mask: What size tubing (small or large bore), how many liters/min can it accommodate, and what oxygen requirements is it best for?
small bore tubing
8-12L/min
moderate oxygen requirements
Where should you avoid attaching a pulse oximeter?
edematous or if skin integrity is compromised
hypothermic
Do not place the sensor on an extremity with an electronic blood pressure cuff
Do not place a reusable clip-on finger sensor on the thumb; it is not designed for the thumb
If capillary refill is prolonged, select an alternative site
leave the sensor in place until the oximeter readout reaches a constant value and the pulse display reaches full strength during each cardiac cycle
What are you noting in your assessment of breathing patterns?
Note depth of respirations and presence of tachypnea (increased respirations), bradypnea (decreased respirations), or orthopnea (shortness of breath that happens when you're lying on your back. Sitting or standing up relieves this symptom).
Name 3 interventions by the nurse to maintain normal respirations
Positioning the client to allow for maximum chest expansion
Encouraging or providing frequent changes in position
Encouraging deep breathing (pursed-lip breathing, may help alleviate dyspnea. The client is taught to breathe in normally through the nose and exhale through pursed lips as if about to whistle, and blow slowly and purposefully, tightening the abdominal muscles to assist with exhalation) & coughing (Normal forceful coughing is highly effective, but some clients may lack the strength or ability to cough normally. Normal forceful coughing involves the client inhaling deeply and then coughing twice while exhaling. Alternative cough techniques such as forced expiratory technique, or huff coughing, may be taught as alternatives for those clients who are unable to perform a normal forceful cough. A client with a pulmonary condition (e.g., COPD) is instructed to exhale through pursed lips and to exhale with a “huff” sound in mid-exhalation. The huff cough helps prevent the high expiratory pressures that collapse diseased airways
Encouraging ambulation
Implementing measures that promote comfort, such as giving pain medications & hydration.
Medications (bronchodilators, anti-inflammatory drugs, leukotriene modifiers, expectorants, and cough suppressants are some medications that may be used to treat respiratory problems)
Percussion (clapping, is forceful striking of the skin with cupped hands - Percussion is avoided over the breasts, sternum, spinal column, and kidneys)
Vibration (series of vigorous quiverings produced by hands that are placed flat against the client’s chest wall.
During the exhalation, tense all the hand and arm muscles, and using mostly the heel of the hand, vibrate (shake) the hands, moving them downward. Stop the vibrating when the client inhales.
Vibrate during five exhalations over one affected lung segment.
After each vibration, encourage the client to cough and expectorate secretions into the sputum container)
Postural Drainage (drainage by gravity of secretions from various lung segments - The sequence for PVD is usually as follows: positioning, percussion, vibration, and removal of secretions by coughing or suction. Each position is usually assumed for 10 to 15 minutes, although beginning treatments may start with shorter times and gradually increase)
kinetic therapy beds with modalities such as vibration and percussion therapy are available. These beds provide continuous lateral rotational therapy (CLRT) along with vibration and percussion modules that are programmed to perform for a specific amount of time
True or False: You can drop an O2 tank without issue
False.
Partial Rebreather: What size tubing (small or large bore), how many liters/min can it accommodate, and what is important to remember about the bag?
small bore tubing
6-10L/min
that it doesn't deflate! increase the liter flow of O2 if it does
Can you administer oxygen in an emergency situation without a providers order?
YES!
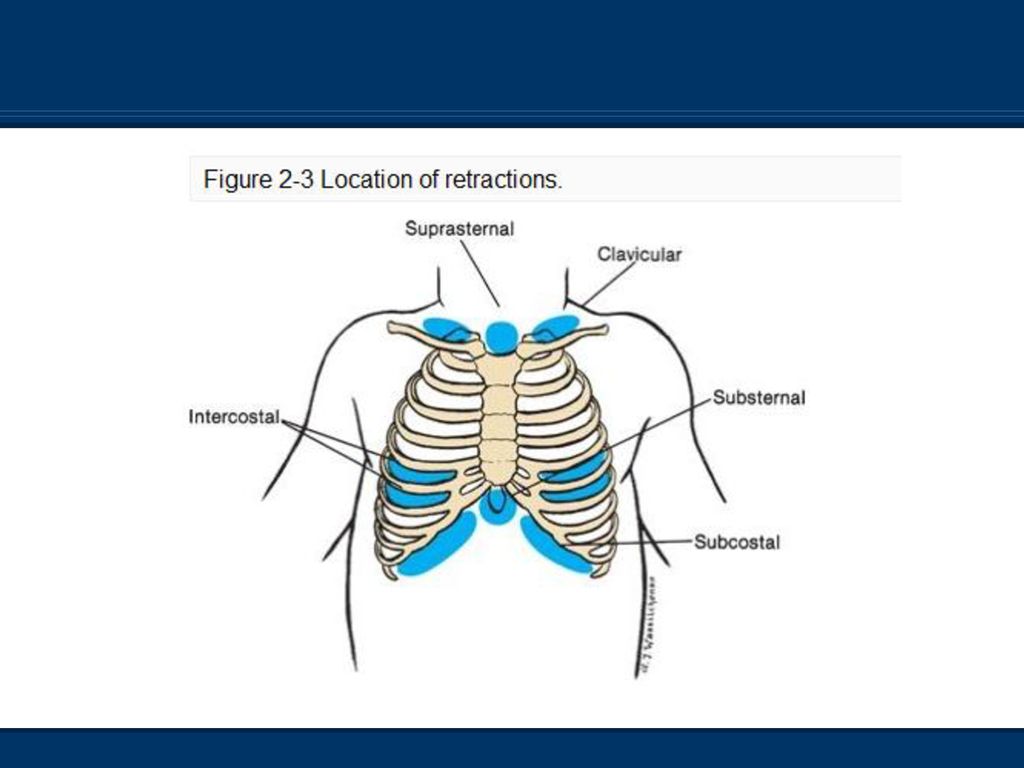
What are you noting in your assessment of chest movements?
Note whether there are any intercostal  substernal, suprasternal, supraclavicular, or tracheal retractions during inspiration or expiration.
substernal, suprasternal, supraclavicular, or tracheal retractions during inspiration or expiration.
Which positions are best for dyspnea?
The semi-Fowler’s or high-Fowler’s position allows maximum chest expansion in clients who are confined to bed, particularly those with dyspnea.
The nurse also encourages clients to turn from side to side frequently, so that alternate sides of the chest are permitted maximum expansion
Dyspneic clients often sit in bed and lean over their overbed tables (which are raised to a suitable height), usually with a pillow for support. This orthopneic position is an adaptation of the high-Fowler’s position. Some clients also sit upright and lean on their arms or elbows, which is called the tripod position
What should be avoided when oxygen is being used by a patient?
Smoking, static electricity, short circuit devices, flammable materials, make sure things are electronically grounded
Oxygen Tent: What type of humidity does it deliver (low or high), how many liters/min can it accomodate, and can you control the concentration of oxygen delivered (yes or no)
high humidity
8-12L/min
no you can't control the concentration
What vital signs are associated with oxygenation?
Pulse rate and quality, and respiratory rate, rhythm, and depth, pulse oximetry.
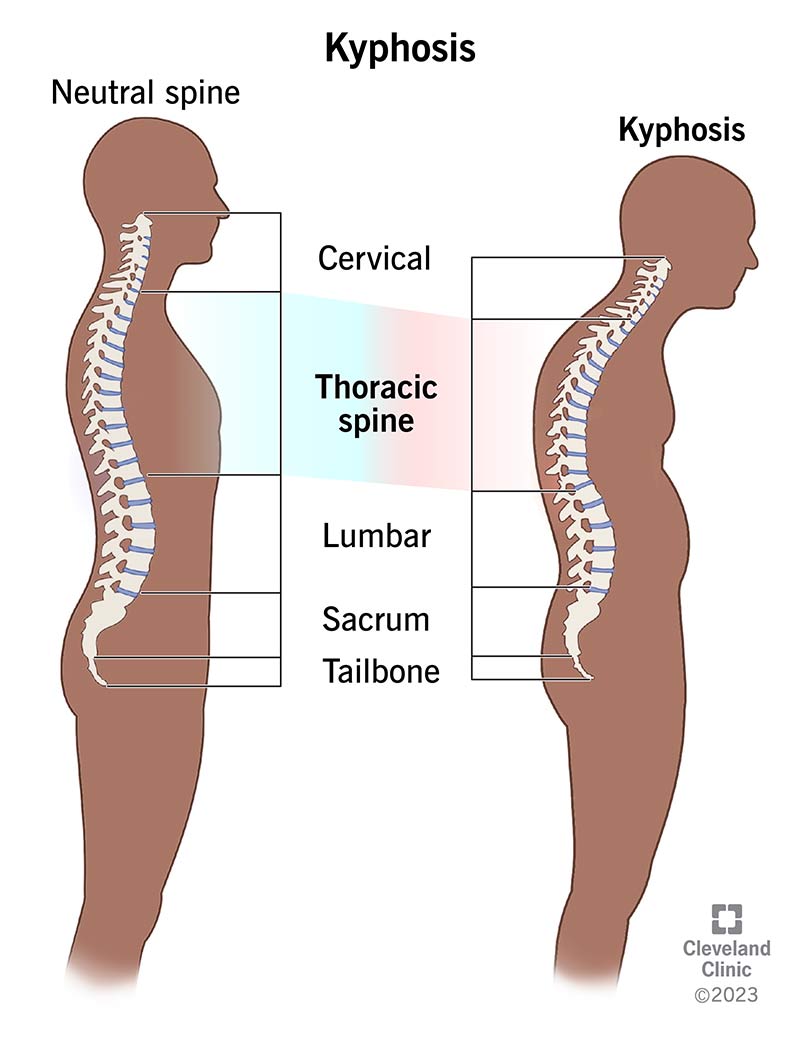
What are you noting in your assessment of chest wall configuration?
kyphosis
unequal chest expansion, barrel chest
How do you teach a patient to use an incentive spirometer?
Instruct the patient to take a slow, deep breath and maintain a constant flow, as if the patient were sucking air through a straw. When the patient cannot inhale any more or when the patient reaches the target volume on the incentive spirometer, instruct the patient to hold a breath for at least 5 seconds and then to exhale normally. Be aware that chronic obstructive pulmonary disease (COPD) may inhibit the patient’s ability to hold a breath. If the patient has COPD, encourage the patient to hold a breath as able and allow the patient to rest between IS breaths to prevent hyperventilation and fatigue.
Ensure that the patient performs IS exercises at least 10 times an hour while awake or as directed by the practitioner
High flow: Venturi Mask
What size tubing (small or large bore), how many liters/min can it accommodate, and what does it allow for oxygen delivery wise?
large bore tubing
4-10L/min
more precise control over delivered oxygen
What device delivers the highest possible concentration of oxygen (60-100%, 6-15L/min) by means other than intubation or mechanical ventilation?
Non-rebreather mask
Why is it important to determine if a client has COPD when administering and monitoring oxygen saturation?
A high carbon dioxide level in the blood is the normal stimulus to breathe. However, people with COPD may have a chronically high carbon dioxide level, and their stimulus to breathe is hypoxemia
What are the clinical signs of hypoxemia?
tachycardia, tachypnea, restlessness, dyspnea, cyanosis, and confusion. Tachycardia and tachypnea are often early signs. Confusion is a later sign of severe oxygen deprivation.
Clients with severe pneumonia or other pulmonary disease in one lung, if positioned laterally, should be generally positioned with which lung down to improve diffusion of oxygen to the blood from functioning alveoli?
good lung down