Name the the clinical purpose of the “Evaluate–Identify–Intervene” sequence when applied dynamically in a deteriorating child.
What is It enforces continuous reassessment and rapid prioritization—prevents fixation error and ensures deterioration is detected early?
These three key assessment findings help you identify when a child in distress has progressed to failure — and require immediate intervention with bag-mask ventilation or intubation.
What are inadequate oxygenation (SpO₂ <90%), inadequate ventilation (rising CO₂, shallow respirations), and altered mental status?
Which type of shock presents with bounding pulses and warm extremities?
What is Early distributive shock (septic/anaphylactic) — vasodilation and increased cardiac output create bounding pulses?
Name the most common reversible cause of pediatric bradycardia, and how does that shape your first action?
What is Hypoxia depresses pacemaker automaticity—correct oxygenation before drugs or pacing?
Name the three parameters that confirm high-quality CPR and how can you monitor these during a code.
What is depth, rate, and recoil and feedback on the zoll and ECTO2 >10?
A stable child now shows increased WOB, delayed cap refill, and altered tone. Name the component of the systematic approach should guide your next targeted intervention.
What is Circulation (C) — the delayed refill + hypotonia suggest perfusion failure, requiring intervention before further airway manipulation.
Name this lung sound and provide one likely causes and treatment.
https://drive.google.com/file/d/1aUYac__3qSzM8_mIfH4H1FSVPdZIBDpo/view?usp=sharing
What is wheezes and asthma (albuterol)?
Name the value that determines compensated v non-compensated shock.
What is SBP?
This is your EKG with poor perfusion despite oxygen—describe your medication sequence and doses.
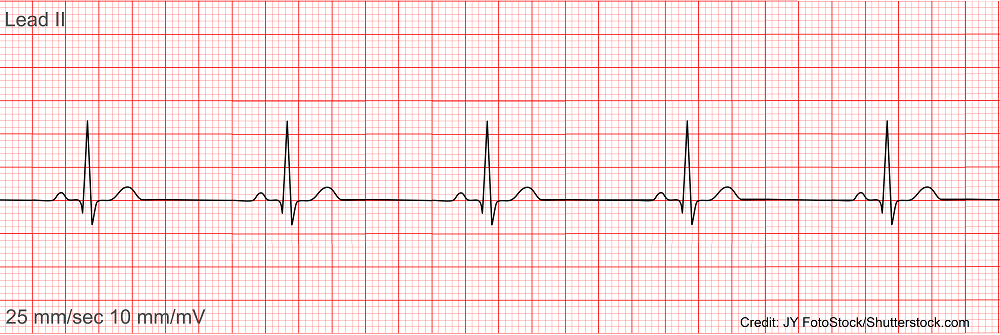
What is Epinephrine 0.01 mg/kg IV/IO q3–5 min → if vagal/AV block, Atropine 0.02 mg/kg (min 0.1 mg, max 0.5 mg) → prepare for pacing.
Treatment for this rhythm
What is 1-2 GM of Magnesium?
HR 50 with poor perfusion despite effective ventilation—describe your immediate sequence of actions.
What is Begin CPR immediately, provide oxygen/ventilation support, and administer epinephrine 0.01 mg/kg IV/IO; reassess every 2 min?
Identify the sound, list two causes, and give two immediate treatments
https://drive.google.com/file/d/1LFx2JK7jJTn2bBWDXxHPeobypDjOVvG5/view?usp=sharing
What is stridor and croup, foreign body, anaphylaxis, and racemicepi, nebulized epi, corticosteroids, and airway management?
Explain the reasoning behind fluid challenge and reassessment timing in suspected septic shock.
What is give 20 mL/kg isotonic boluses with reassessment after each; reassess for rales, hepatomegaly, or worsening perfusion q5–10 min?
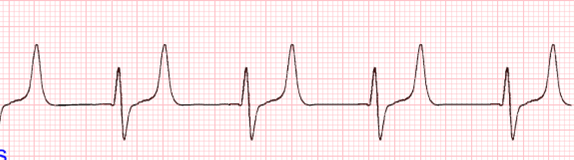
Name this rhythm

What is second degree type II heart block?
A 14-year-old patient with metastatic osteosarcoma and a tunneled central line suddenly becomes pale, hypotensive, and tachycardic during chemotherapy.
You note JVD, and weak pulses.
The monitor shows narrow QRS complexes with low voltage.
Despite a fluid bolus, the patient’s blood pressure continues to drop, and the rhythm deteriorates into PEA.
Name the “T” is the likely cause of this arrest, and what are the immediate interventions.
What is:
Tamponade (cardiac) → Pericardiocentesis to remove fluid?
HR 50 with poor perfusion despite effective ventilation, you begin CPR.
HR improves but perfusion remains poor. Name the next advanced step or diagnostic should you consider next.
What is Persistent poor perfusion with improved HR → consider shock (distributive, cardiogenic, obstructive); evaluate rhythm, perfusion pressures, and preload?
Name the respiratory emergency and two treatments.
https://drive.google.com/file/d/1TCqc6pOJR2qHsff74olUriZhMUvSOcne/view?usp=sharing
What is coarse crackles and lung tissue disease, goal to culture and start antibiotics?
Distinguish obstructive vs cardiogenic shock using bedside findings in a patient.
What is:
Obstructive: JVD + muffled sounds + clear lungs → tamponade
Cardiogenic: crackles, hepatomegaly, low output.
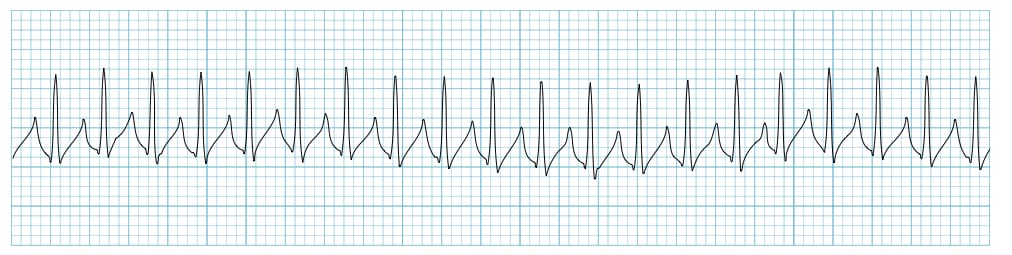
Name this rhythm and treatment.

What is Monomorphic VT: wide QRS > 0.09 sec, regular rhythm; treat with synchronized cardioversion 0.5–1 J/kg, escalate if needed?
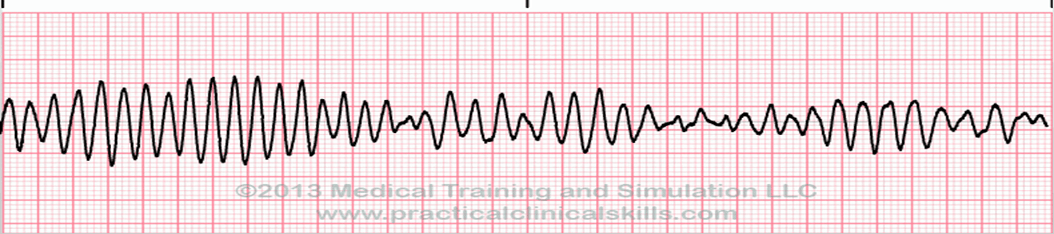
You’re called to evaluate a 12-year-old oncology patient with acute lymphoblastic leukemia who became suddenly unresponsive and lost pulse during chemotherapy. Monitor shows this strip, what is the likely cause of cardiac arrest and what are your priority medications.
What is peaked T waves due to hyperkalemia caused by tumor lysis syndrome and IV insulin, dextrose and calcium?
This process helps you tell the difference between sustained recovery and short-lived stabilization in a compensating child.
What is ongoing reassessment after intervention? Sustained improvement shows normalization of perfusion parameters (HR, pulses, mental status), not just transient vitals?
Name the respiratory emergency and one cause where the body can't regulate breathing, pattern is often slow and shallow
What is disordered control of breathing, neurological disorder (head trauma, brain tumor) and support airway?
Name all four shock states and a primary cause and treatments.
What is
Hypovolemic – bleeding, n/v - if bleeding give blood, otherwise give fluids.
Distributive – sepsis, anaphylaxis - fluids + vasopressors
Obstructive – PE, tamponade, tension pneumothorax - relieve obstruction: thrombolytics, pericardiocentesis, needle decompression
Cardiogenic – congenital heart disease, myocarditis, and other cardiomyopathies -inotropes, cautious fluids
Name this rhythm, treatment and what three assessments determine stable v. unstable.
What is SVT (narrow QRS, no P-waves) — attempt vagal maneuvers → adenosine 0.1–0.2 mg/kg rapid IV push → if unstable, synchronized cardioversion, acutely altered mental status, signs of shock, and hypotension?
A 15-year-old patient with Hodgkin lymphoma and a large mediastinal mass is in the PICU receiving positive-pressure ventilation after a central line placement.
Suddenly, the patient’s heart rate drops, SpO₂ falls to 70%, and the ventilator peak pressures climb sharply. Name the “T” is the likely cause of this cardiac arrest, and what immediate interventions should be performed.
What is tension pnx and Immediate needle decompression in the affected side’s 2nd intercostal space, mid-clavicular line (or 4th–5th intercostal, anterior axillary line)?