A&B
What are the three stages of the General Adaptation System?
Alarm, Adaptation, and Exhaustion
The three successive stages of the General Adaptation Syndrome Response include: 1 - Alarm: Recognition of environmental change and trigger of HPA and SNS. 2 - Adaptation (or Resistance): Action of adrenal hormones (cortisol) and SNS neurotransmitters (epi and NE). 3- Exhaustion stage: The body can not successfully adapt to stress anymore.
Of the total body water, about ⅓ is:
Extracellular fluid.
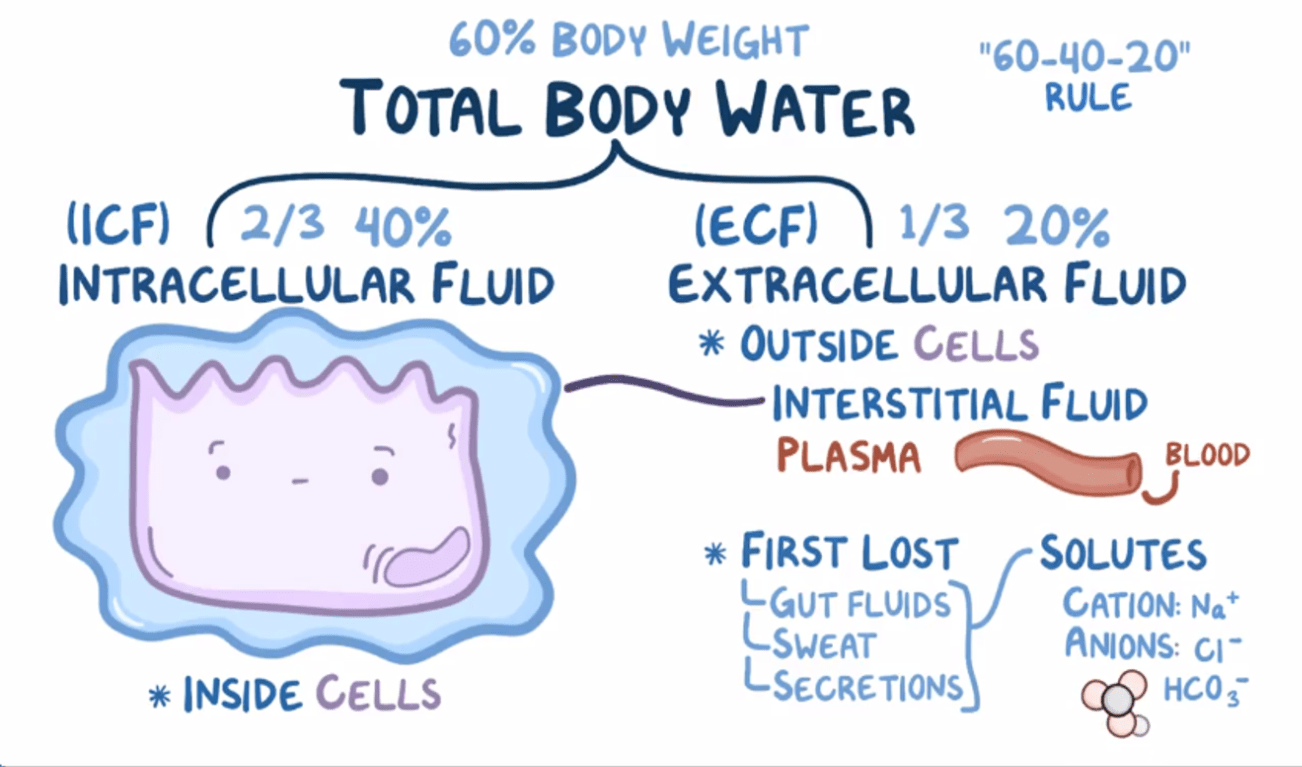
60% of our total body weight is made up of water. Of that 60%, 1/3rd is extracellular fluid. This is the fluid that is outside the cells and it includes intravascular fluid, interstitial fluid, and transcellular fluid. The other 2/3rds consists of the intracellular fluid (the fluid inside cells).
This gland located in the brain regulates the release of hormones from the anterior and posterior pituitary
What is the hypothalamus?
The hypothalamus serves as the control center for the endocrine system. It releases both releasing and inhibiting hormones that control the anterior pituitary’s secretion of hormones, while directly influencing the posterior pituitary by storing and releasing hormones
What is the normal range for WBCs? What would high (leukocytosis) or low (leukopenia) indicate?
5,000 - 10,000
Leukocytosis (high WBCs) is a result of infection but it is also a normal result of other physiologic stressors including strenuous exercise, emotional changes, temperature changes, anesthesia, surgery, pregnancy, and some drugs, hormones, and toxins. It can also result from malignancies and hematologic disorders.
Leukopenia (low WBCs) is never normal and leads to a high risk of infection. It can be a result of radiation, anaphylactic shock, autoimmune disease (e.g., systemic lupus erythematosus [SLE]), immune deficiencies, and certain drugs, such as glucocorticoids and chemotherapeutic agents.
What is the formula for cardiac output?
CO = HR * SV
Cardiac output is equal to the amount of blood pumped out of the heart in each beat (SV) multiplied by the times the heart beats each minute (HR).
This is normally 5 L / min (assuming HR=70 bpm and SV=70 mL).
Cardiac output is determined by preload, afterload, contractility, and heart rate.
This term describes chronic overactivation of adaptive regulatory physiologic systems that may lead to pathophysiology and onset of disease
Allostatic Overload.
When the body is under stress in the adaptation stage, the physiologic regulatory systems (sympathetic nervous system, hypothalamic-pituitary axis, and inflammatory system) are constantly activated and working to maintain homeostasis. This constant stress has the potential to lead to diseases and disorders. Think about how some people get sick after a stressful finals season. Psychological stress is being increasingly recognized as a precipitating factor (trigger) and contributor to behavioral (anxiety), physiologic (chronic pain, asthma), and metabolic disorders (obesity, DM T2)
A 75 year old male presents to a family medicine clinic. He complains of several days of increasingly productive cough with green sputum. He also complains of increasing shortness of breath. He has a long history of COPD and is on a 2L/min baseline. Here is his ABG. What is your interpretation?
pH: 7.30
pCO2: 62
pO2: 60
HCO3: 25
pH: 7.30 (7.35-7.45)
pCO2: 62 (35-45 mmHg)
pO2: 60 (80-100 mmHg)
HCO3: 25 (22-26 mEq/L)
Interpretation: Respiratory acidosis
The strongest drive for us to breathe when we hold our breath is not hypoxia. It is hypercarbia – the buildup of CO2 in our bodies. When our brain senses that the pH is dropping it makes us ventilate. People who have long terms cardiopulmonary conditions like CHF and COPD lose their drive to breath from a rise in CO2. They fall back on the secondary drive to breathe – low oxygen
This hormone is secreted by the adrenal cortex and helps regulate Na+ and water balance; acting on the kidneys
What is aldosterone?
Aldosterone is a key mineralocorticoid produced by the adrenal cortex that helps regulate blood pressure by increasing sodium reabsorption in the kidneys, which also increases water retention, helping to maintain blood volume and pressure.
Aldosterone works on the neprhons in the kidney to favor sodium and water reabsorption and potassium excretion. It does this by influencing sodium-potassium pumps and other cellular transporters.
Angiotensin II also regulates fluid balence but it starts out as angiotensinogen (from the liver) and is converted by renin and ACE to AT II.
Antiduretic Hormone (ADH) also regulates fluid balence but it is released by the posterior pituitary gland after osmoreceptors in the hypothalamus recognize increased serum osmolality
A 6 yo white male patient presents with bone pain, night sweats, and increased bruising. You suspect leukemia. What kind of leukemia is most likely?
Acute Lymphoblastic Leukemia (ALL)
ALL is most common in early childhood (2-4 yrs), boys, and Hispanic and white children.
Immature B (pre-B) or T (pre-T) (lymphoblasts) are produced at an inappropriately fast rate which replaces the bone marrow causing bone pain and disrupting normal function.
Sort descriptors into "Right Heart" and "Left Heart"
- Receives blood from body
- Receives blood from lungs
- Receives oxygenated blood
- Receives deoxygenated blood
- Pumps blood to body
- Pumps blood to lungs
- Low pressure system
- High pressure system
- Tricuspid valve
- Mitral valve
- Pulmonic valve
- Aortic valve
Right Heart:
Receives blood from body
Deoxygenated blood
Pumps blood to pulmonary arteries, capillaries, and veins
Low pressure system
Tricuspid and pulmonic valves
Left Heart:
Received blood from lungs
Oxygenated blood
Pumps blood to body
High pressure system
Mitral and aortic valves
The sympathetic nervous system releases epinephrine and norepinephrine to assist in the fight or flight response. List at least three physiological effects of catecholamines (epinephrine and norepinephrine).
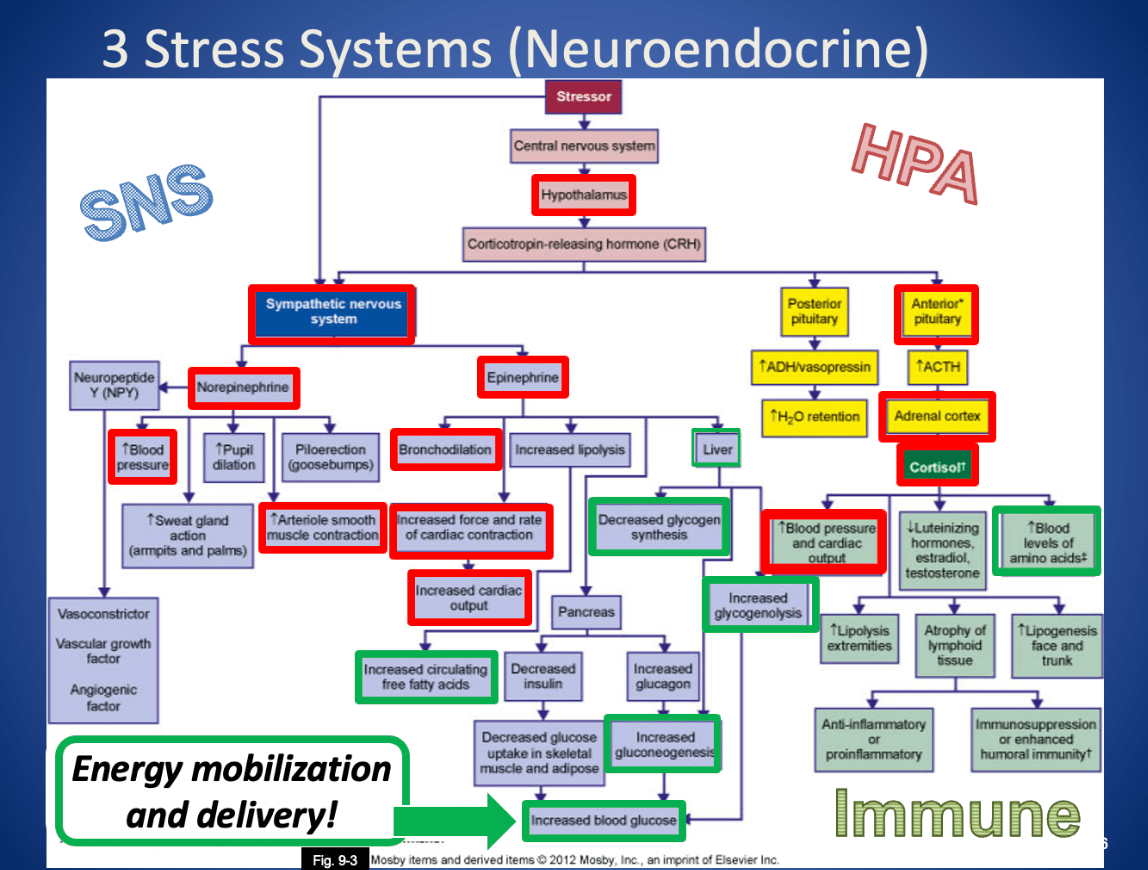
Increase glucose metabolism, increase HR and contractility of heart, peripheral vasoconstriction, bronchodilation, increased glucogenolysis in skeletal muscles, dilation of vessels in muscles, increased glycogenolysis in the liver, increased lipolysis
A patient is admitted to the hospital with edema in the lower extremities. Which of the following factors is likely contributing to the accumulation of fluid in the interstitial space? SATA
a. Hydrostatic pressure in the interstitial space
b. Oncotic pressure in the capillaries
c. Hydrostatic pressure in the capillaries
d. Oncotic pressure in the interstitial space
a. Hydrostatic pressure in the interstitial space
b. Oncotic pressure in the capillaries
c. Hydrostatic pressure in the capillaries
d. Oncotic pressure in the interstitial space
C and D contribute because an increase in capillary hydrostatic pressure pushes fluid out of the capillaries into the interstitial space, and a decrease in capillary oncotic pressure reduces the pull of fluid back into the capillaries, both favoring edema formation.
A and B would do the opposite because hydrostatic pressure in the interstitial space would oppose movement of fluid out of the capillaries and oncotic pressure in the interstitial space exerts a pulling force on fluid out of the capillary, drawing fluid back in from the surrounding tissues.
Name a process that is regulated by positive feedback
Labor, ovulation, some thyroid regulation
Positive feedback occurs when a neural, chemical, or endocrine response increases the synthesis and secretion of a hormone.
Low thyroid hormone levels stimulates the hypothalamus to release thyrotropin-releasing hormone (TRH). The TRH stimulates the anterior pituitary to release of thyroid-stimulating hormone (TSH). TSH stimulates the thyroid gland to release thyroid hormones (T3, T4).
Negative feedback occurs when a changing chemical, neural, or endocrine response to a stimulus decreases the synthesis and secretion of a hormone.
Increasing levels of thyroid hormone (T3,T4) act on the hypothalamus and pituitary to inhibit TRH and TSH synthesis which decreases the production of thyroid hormones.
- Estrogen is one of the few hormones regulated by positive feedback, particularly during ovulation, where increased estrogen levels trigger a surge in luteinizing hormone (LH), which promotes ovulation.

What is the primary hormone that regulates erythropoiesis and describe how it works
Erythropoietin uses a feedback loop to keep the concentration of red blood cells at a constant level (hematocrit, or percentage of blood that is RBCs, is around 40%). The kidneys “screen” the blood to determine if the oxygen carrying capacity needs to be increased. If it determines this must happen, the peritubular cells of the kidneys secrete EPO. This causes an increase in erythrocyte production.
You are a red blood cell. You are in the inferior vena cava and about to enter the heart. Describe your journey through the heart going chamber by chamber and listing the valves.
Right atrium, tricuspid valve, right ventricle, pulmonic valve, pulmonary arteries, lungs, pulmonary veins, left atrium, mitral valve, left ventricle, aortic valve
This function of the immune system is initially beneficial in the stress response but is harmful when chronic.
Inflammation.
Norepinephrine, epinephrine, and cortisol stimulate immune cells to produce IL-1, IL-6, and TNF alpha. These are all proinflammatory cytokines. The constant high levels of cortisol cause the glucocorticoid receptor (GR) to become downregulated and limit the antiinflammatory effects of cortisol. Together, these cause high levels of inflammation and decreased immune function.
A 68-year-old patient presents with confusion, muscle cramps, and mild nausea. Laboratory tests reveal a serum sodium of 128 mEq/L. Urinalysis shows very concentrated urine with a low output. Which condition best explains these findings?
a. Syndrome of Inappropriate Secretion of ADH (SIADH)
b. Diabetes Insipidus
c. Fatigue
d. Excessive Water Intake
Syndrome of Inappropriate Secretion of ADH (SIADH)
In SIADH, excessive ADH leads to water retention, diluting the serum sodium (resulting in hyponatremia at 128 mEq/L) while the kidneys produce very concentrated urine with low output. In contrast, Diabetes Insipidus would cause large volumes of dilute urine, excessive water intake would also produce dilute urine, and "Fatigue" is a symptom rather than a condition.
Fill in the blanks: In ______________ (or Hashimoto’s Disease), loss of thyroid function leads to decreased production of ________ and subsequent increased secretion of ______ and ________ by the hypothalamus and pituitary glands respectively.
In primary hypothyroidism, loss of thyroid function leads to decreased production of TH and increased secretion of TRH and TSH.
The most common causes of primary hypothyroidism in adults include autoimmune thyroiditis (Hashimoto disease), iatrogenic loss of thyroid tissue after surgical or radioactive treatment for hyperthyroidism or after head and neck radiation therapy, medications (e.g., lithium and amiodarone), and endemic iodine deficiency. Infants and children may present with hypothyroidism because of congenital defects. Central (secondary) hypothyroidism is caused by the pituitary's failure to synthesize adequate amounts of TSH or a lack of TRH. Pituitary tumors that compress surrounding pituitary cells or the consequences of their treatment are the most common causes of central hypothyroidism. Other causes include traumatic brain injury, subarachnoid hemorrhage, or pituitary infarction. Hypothalamic dysfunction results in low levels of TH, TSH, and TRH.
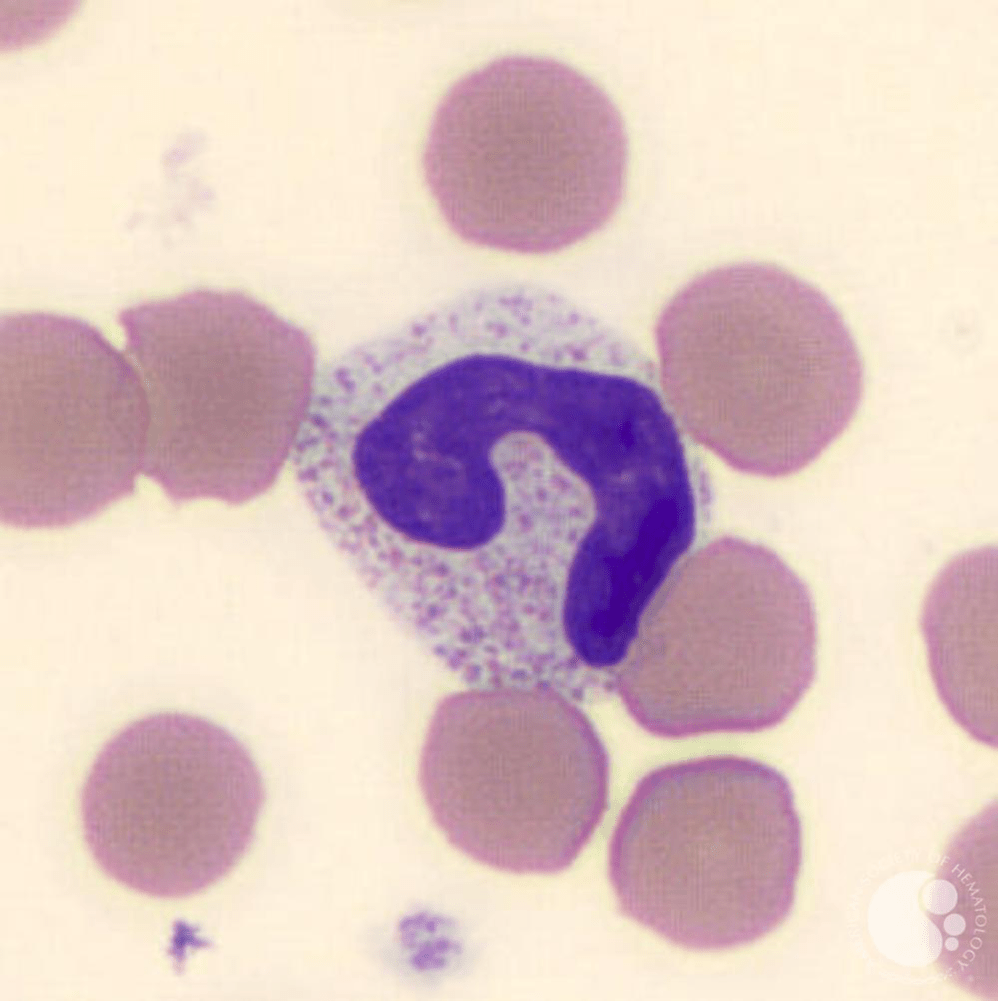
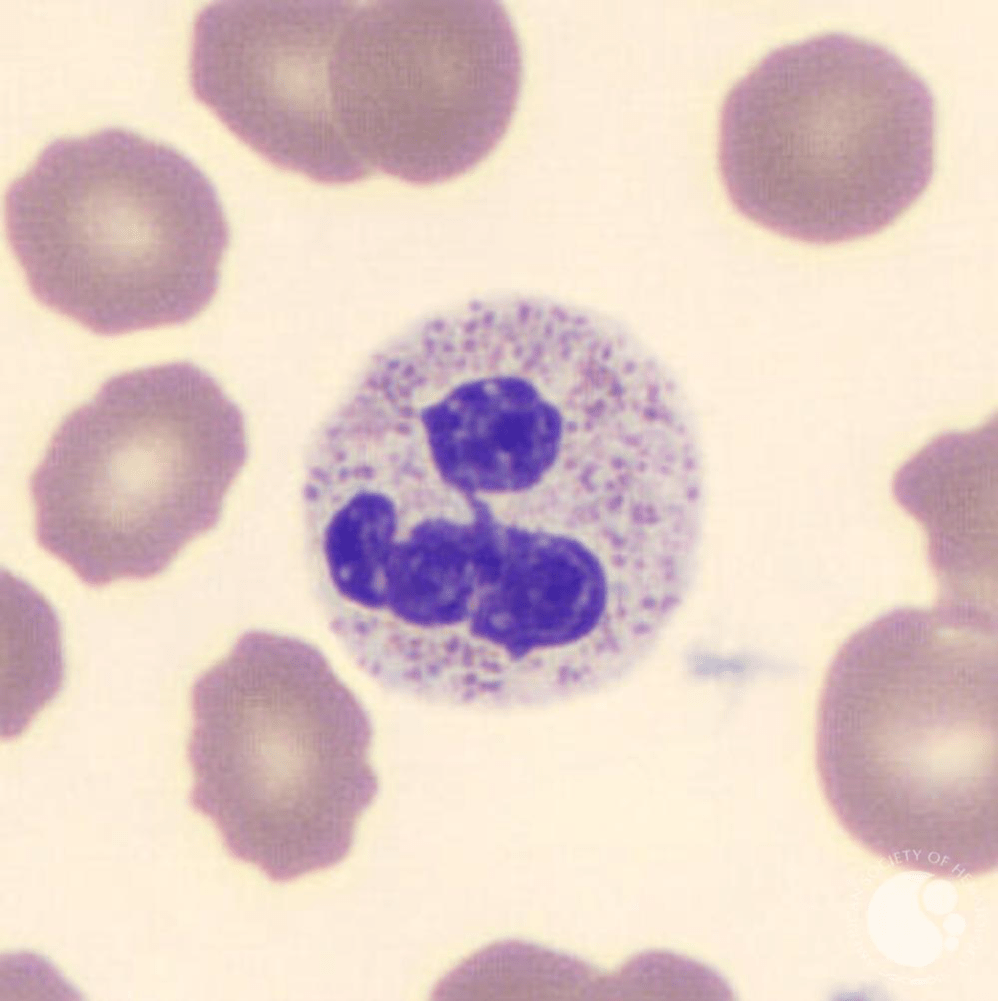
Identify the following white blood cell and explain a possible cause for seeing an increase of these types of cells within the blood.
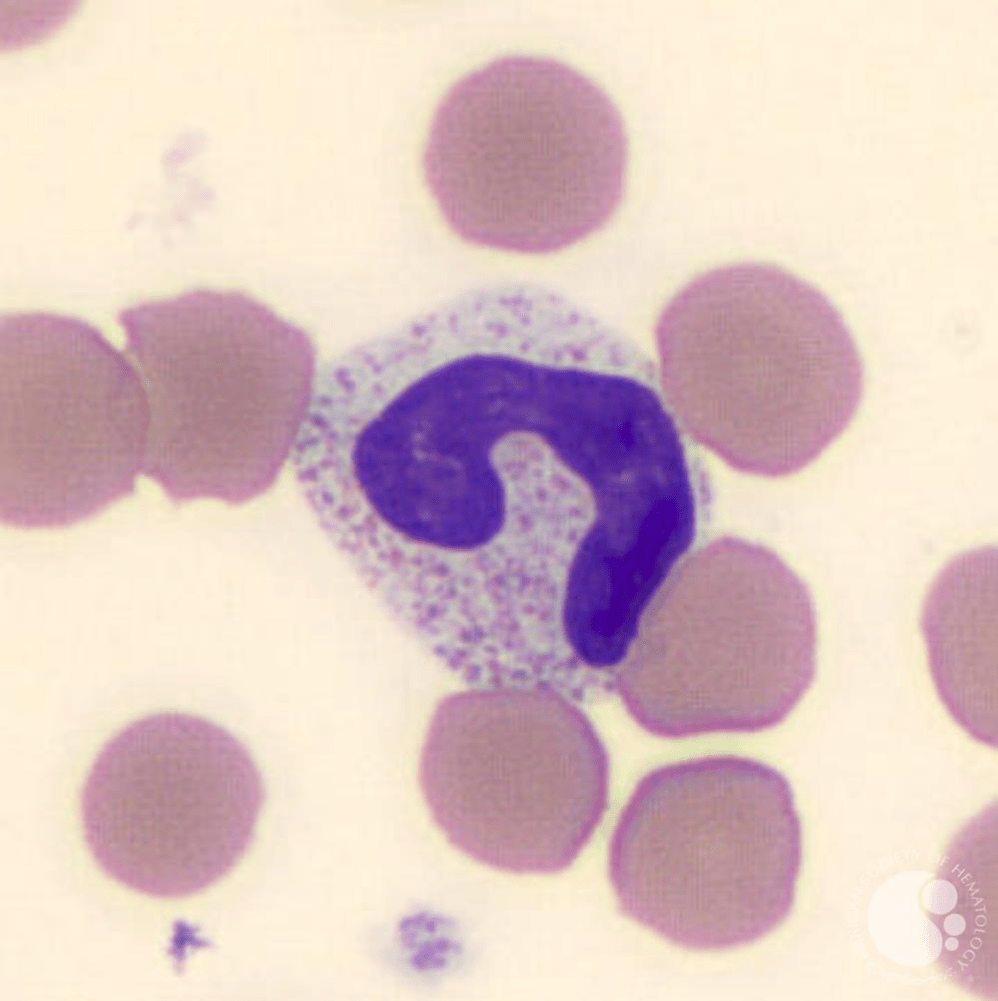
Unsegmented or band neutrophil. In cases of high demand for white blood cells like infection, WBCs are released before they can mature. This leads to a “shift to the left”
"Band neutrophils are slightly less mature than segmented neutrophils and have indented, unsegmented "C" or "S" shaped nuclei. Band neutrophils normally account for approximately 5-10% of peripheral blood leukocytes. An increased proportion of band neutrophils can be seen in infectious and inflammatory conditions." - American Society of Hematology
A patient is diagnosed with deep vein thrombosis (DVT). Which factors from Virchow's Triad are most likely contributing to thrombus formation?
Stasis of blood flow, endothelial injury, and hypercoagulability
Virchow's Triad describes three primary factors leading to thrombus formation:
Stasis of blood flow: Reduced or stagnant blood flow promotes clot formation.
Endothelial injury: Damage to the vessel lining triggers the clotting cascade.
Hypercoagulability: Increased clotting activity due to conditions like cancer or genetic factors.
In the Hypothalamic Pituitary Axis, stress activates the hypothalamus to release corticotropin-releasing hormone (CRH) which binds to anterior pituitary cells and stimulates them to release this hormone
Adrenocorticotropic Hormone (ACTH)
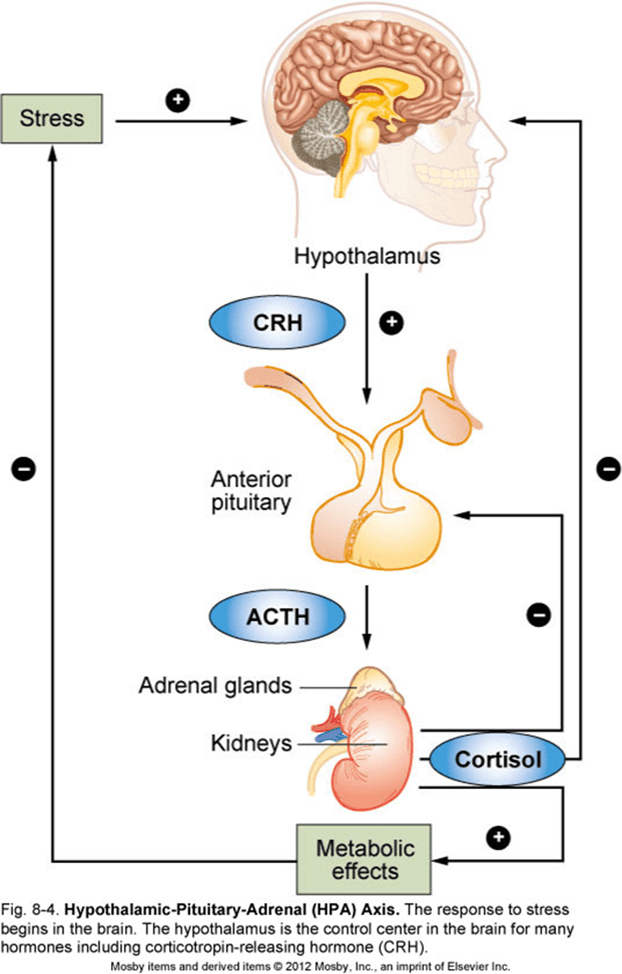
ACTH then travels through the bloodstream to the adrenal glands atop the kidneys and stimulates them to release cortisol which acts to mobilize energy (by releasing glucose) for the fight or flight response. In the negative feedback loop, the hypothalamus will adjust the level of CRH it releases based on the cortisol level in the blood.
Describe the RAAS pathway
The RAAS (Renin-Angiotensin-Aldosterone-System) regulates fluid balance within the body.
Stimulus -> Kidney -> Renin -> AT -> AT 1 -> ACE -> AT 2 -> Adrenal cortex -> aldosterone -> Kidney -> sodium retention, water retention -> increased BP
-> AT 2 -> vessels -> vasoconstriction -> increased BP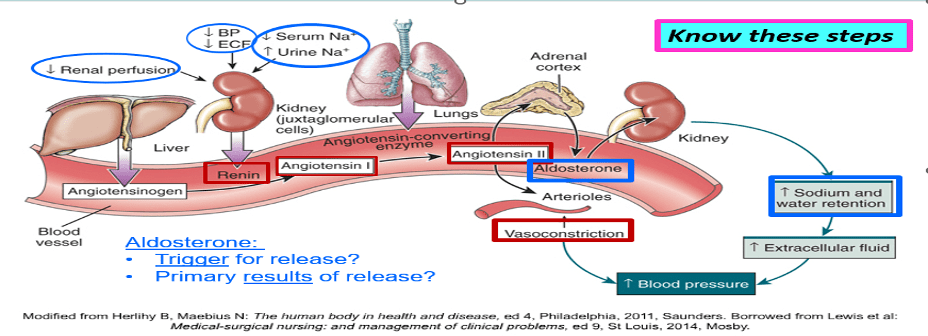
How are calcium and phosphorous levels typically related, and which hormone plays a key role in regulating calcium levels in the blood?
a. Directly proportional; Thyroxine (T4)
b. Inversely related: Parathyroid hormone PTH)
c. Directly proportional; Insulin
d. Inversely related; Thyroid-stimulating hormone (TSH)
Directly proportional; Thyroxine (T4)
Inversely related: Parathyroid hormone PTH)
Directly proportional; Insulin
Inversely related; Thyroid-stimulating hormone (TSH)
Calcium and phosphorus levels are inversely related—when calcium levels increase, phosphorus levels decrease and vice versa. PTH is the primary hormone responsible for regulating calcium levels by increasing calcium reabsorption in the kidneys, stimulating calcium release from bones, and increasing calcium absorption in the intestines.
List a macrocytic-normochromic anemia, microcytic-hypochromic anemia, and a normocytic-normochromic anemia.
Macrocytic-normochromic: B-12 deficiency/pernicious, folate deficiency. In these the DNA is misfolded and not condensed as it should be. Think of a suitcase that is trying to be stuffed with unfoleded clothes.
Microcytic-hypochromic: IDA, thalassemia, sideroblastic. In these the hemeoglobin is missing something. Think of a suitcase with not quite enough clothes.
Normocytic-normochromic: Sickle cell, posthemorrhagic, aplastic, hemolytic, anemia of chronic inflammation/disease. This typically results from loss or destruction of appropriately made RBCs.
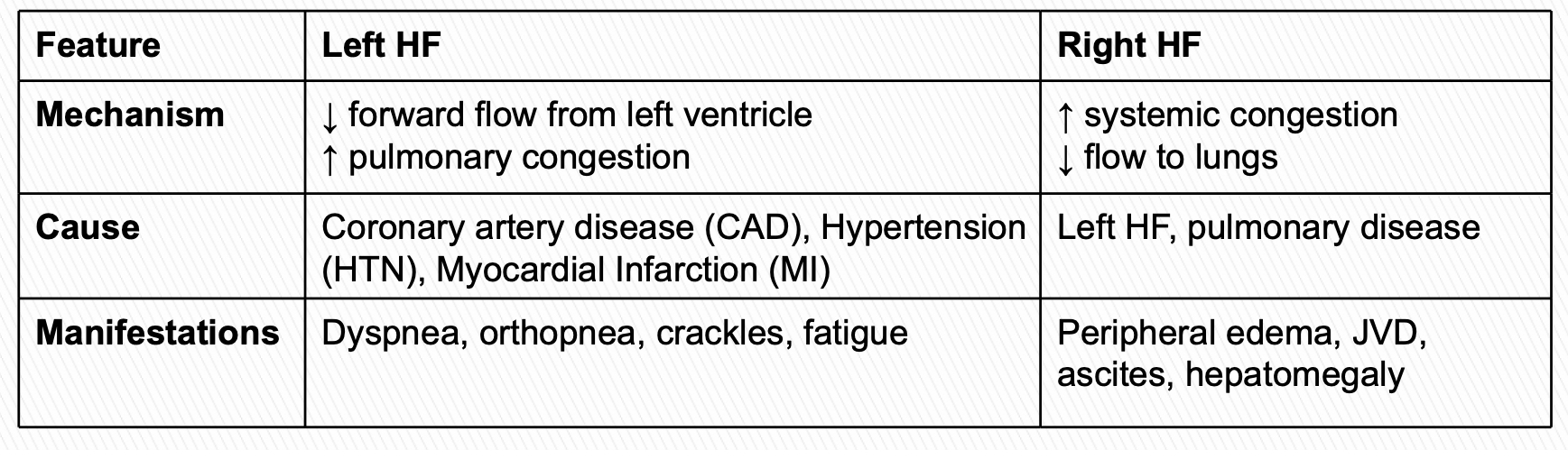
Describe one mechanism, cause, and manifestation of both left and right sided heart failure.