Which antibiotics affect the bacterial cell wall? And which ones have a beta lactam ring?
Penicillins, cephalosporins, carbenems, Vancomycin
What is bioavailability?
The term for how much of a drug reaches systemic circulation after administration.
The Cholinergic receptors mediate the response to which neurotransmitter? The Adrenergic receptors mediate the response to which neurotransmitter?
Cholinergic - Acetylecholine
Adrenergic - Epinephrine/ Norepinephrine (adrenaline)
What is Erythropoiesis?
Production of red blood cells in the body.
What is the difference between affinity and intrinsic activity?
Affinity is the strength of attraction between a drug and its receptor (how easy it gets there). While intrinsic activity is the ability of a drug to activate a receptor after binding (what it does when it gets there).
What is a sign of a systemic infection?
Bonus: Where is the Thermoregulatory center? What does it regulate?
Fever, malaise, fatigue
Bonus: Thermoregulatory center (TRC) is in the hypothalamus. (regulates core body temp)
Which solution would you use to treat cerebral edema? Which for dehydration/ loss of fluid? Which for treating hypernatremia?
cerebral edema- hypertonic solution (shrink cells)
dehydration- isotonic solution
hypernatremia- hypotonic solution (cells swell)
A patient reports an allergy to penicillin. Which antibiotic class would the nurse need to be most cautious about administering? Which antibiotic would they most likely administer instead?
cautious of cephalosporins and likely to administer a macrolide instead.
Grapefruit juice inhibits the cytochrome P450 enzyme for several days after ingestion.
what would the nurse teach the client about the problem that drinking grapefruit juice can cause when taking medications? and why?
Excess levels of drug in the blood. Increased toxicity risk because the cytochrome P450 enzyme enhances hepatic metabolism. So there will be a lack of metabolism-too much drug.
What is the difference between a direct acting and indirect acting cholinergic drug?
Direct-acting cholinergic drugs bind to and activate cholinergic receptors, while indirect-acting cholinergic drugs increase acetylcholine levels by inhibiting the acetylcholinesterase, therefore inhibiting the breakdown of acetylcholine.
Test to monitor heparin therapy effectiveness?
Test to monitor Warfarin efficacy?
aPTT for heparin.
INR for warfarin.
What are two characteristics of Modified Occupancy Theory that help explain differences in drug reaction?
Bonus: What is single occupancy theory and what does it fail to account for?
Affinity and Intrinsic Activity.
-higher affinity = higher potency
-higher intrinsic activity = higher maximum efficacy
Bonus: Theory that suggests that the intensity of a drug response is related to the number of receptors occupied. Does not account for differences in drug potency.
Name three to four characteristics of the inflammatory response.
Redness, swelling, pain, heat, vasodilation, and increased capillary permeability.
What is the function of the RAAS system? What electrolyte does it regulate?
Bonus: What does RAAS stand for?
To regulate blood pressure and fluid balance. It regulates amount of Sodium released or retained.
Bonus: Renin-Angiotensin-Aldosterone-System
Why would someone be prescribed amoxicillin and calcium clavulanate (Augmentin) if the amoxicillin has been ineffective in the past?
The calcium clavulanate prevents penicillinase (a beta-lactamase) from inactivating the amoxicillin.
Name one factor that influences drug absorption, one that influences distribution, one that influences Metabolism, and one that influences excretion.
A: drug properties, route of administration, pH partitioning (ion trapping), blood flow, surface area, food.
D: blood flow, protein binding, ability to exit the vascular system, ability of the drug to enter the cell.
M: age, liver function, drug interactions, first-pass effect, Enterohepatic recirculation, pharmacogenomics, nutrition.
E: Kidney function, age, blood flow.
What effects will we see in our saliva, eyes, urinary system and heart rate with a muscarinic agonist medication?
increased production of saliva, bradycardia (slowed heart rate), increased urination, miosis (constriction of pupils).
What does Protamine Sulfate do?
Reverses the effects of Heparin. (antidote)
What are these curves showing is different between these two drugs?
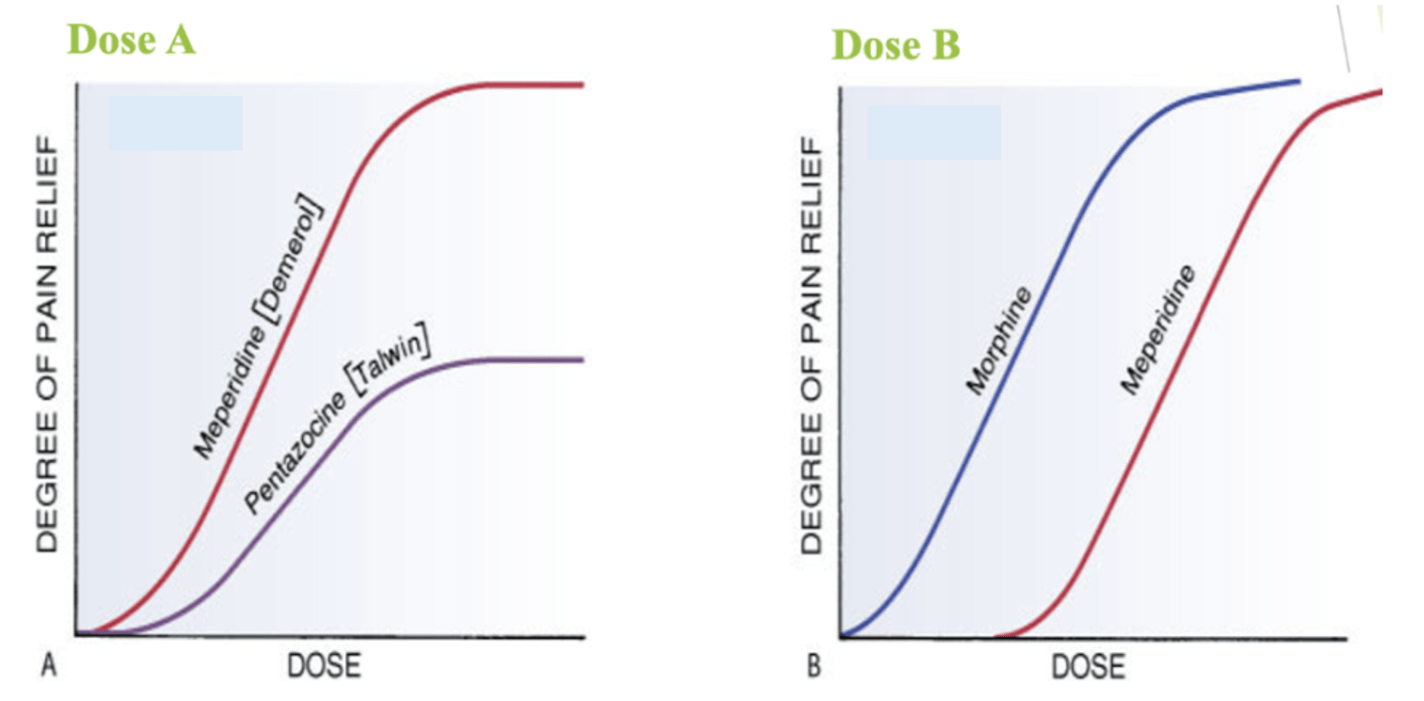
Dose A is showing a difference in efficacy and dose B is showing a difference in potency.
Which of the following is an example of active immunity?
A. Receiving a tetanus booster shot
B. Acquiring antibodies from breast milk
C. Receiving intravenous immunoglobulin (IVIG)
D. Inheriting maternal antibodies across the placenta
Receiving a tetanus booster shot
Describe the process of SIADH. (Syndrome of Inappropriate ADH).
Bonus: What electrolyte imbalance is being caused?
Process where your body is producing too much antidiuretic hormone (ADH), leading to excessive water retention and decreased thirst. (increase in water fluid)
Bonus: hyponatremia (low sodium-from dilution)
Which drug is reserved for MRSA and VRE infections and why do we reserve it for these uses?
Linezoid and so we do not aqcuire resistance to the drug with overuse.
What is the first-pass effect, and how does it influence drug bioavailability? What route goes through first pass effect?
The first-pass effect refers to the metabolism of a drug by the liver before it reaches systemic circulation, significantly reducing its bioavailability. Drugs administered PO/enterally are often subject to this effect, leading to a lower concentration in the bloodstream compared to intravenous administration.
What is the treatment for cholinergic crisis
Pralidoxime, Atropine?
What are thrombolytic drugs used for? What is their biggest constraint? What are the two thrombolytic drugs we learned about?
Bonus: What type of stroke do we use it for/ what type of stroke do we NOT use it for?
They dissolve blood clots and restore blood flow. They turn plasminogen to plasmin which degrades fibrin to dissipate clots. their biggest constraint is the time restriction (must be used within a few hours of symptoms onset) Two types are tPA and Streptokinase.
Bonus: Can be used for a ischemic stroke, but NOT a hemorrhagic stroke.
A nurse is preparing to administer a controlled substance. What 3 nursing actions are most essential with this type of drug? Who regulates controlled substances?
Double check of drug by another nurse before administering. Documented/ witnessed waste disposal. Record keeping is required of all inventory.
Are regulated by the Drug Enforcement Administration (DEA).
What are the steps of the cellular stage of inflammation?
What two things happen during the vascular stage of inflammation?
Cellular stage: migration and adhesion, transmigration, chemostasis, and phagocytosis.
Vascular Stage: Vasodilation and increased permeability
Describe the process of Diabetes Insipidus.
Bonus: What electrolyte imbalance does it cause?
Causes excessive water loss and increased urination and increased thirst. No ADH is secreted.
A dehydration cycle that causes polydipsia and polyuria because water failing to be reabsorbed in body.
Bonus: hypernatremia (high sodium levels)
Which antibiotic has irreversible ototoxicity, but reversible nephrotoxicity?
Which antibiotic causes discoloration in developing teeth?
Aminoglycosides
Tetracyclines
A nurse administers a drug with high protein affinity to a patient with hypoalbuminemia. What affect will this have on the drug concentration.
In hypoalbuminemia, fewer proteins are available to bind the drug, increasing free (active) drug levels. This raises the risk of toxicity, side effects, and overdose.
What is a classic symptom of myasthenia gravis? What category of drug is the primary treatment?
Bonus: Can you name a drug that treats Myasthenia Gravis?
ptosis (drooping eyelid) or muscle weakness.
acetylcholinesterase inhibitors.
Bonus: Neostigmine, edrophonium, ambenonium
What is the difference between how Heparin and Warfarin work as anticoagulants?
Bonus: How does Eliquis/Amixaban differ in how it works?
Heparin activates antithrombin III which prevents prothrombin converting to thrombin and from factor X working. Warfarin works by interfering with ability to use vitamin K, which is essential for clotting.
Bonus: Amixaban is a direct inhibitor of Factor X, preventing the conversion of prothrombin to thrombin. Unlike heparin, it works independently of antithrombin III.
Discuss the implications of a narrow therapeutic index on drug interactions and patient management (what 2 things do you need to check). What is an ED50 and LD50.
A narrow therapeutic index indicates that small changes in dosage or blood concentration can lead to toxicity. Checking liver and kidney function and taking blood serum levels.
ED50 : The average effective dose. The dose required to produce a defined effect in 50% of population.
LD50: ratio between effective dose and lethal dose.
What Ig class is involved in allergic responses and inflammation? Which Ig class is most abundant and can cross the placenta?
Bonus: which Ig class is in breastmilk?
allergies- IgE
most abundant - IgG
Bonus: Breastmilk- IgA
What is a symptom of hypokalemia? What is a symptom of hyperkalemia?
Bonus: why do you have to be careful when increasing K+ via IV?
hypokalemia: fatigue, cardiac rhythm changes, N/V/D.
hyperkalemia: EKG abnormal rhythms, neuromuscular excitability.
Bonus: need to infuse Potassium slowly to avoid putting patient into cardiac arrest.
Which four of these drugs are used for the treatment of TB? Are most of them hepatotoxic or nephrotoxic?
Isoniazid (INH), Erythromycin, Rifampin, Pyrazinamide, Bactrim, Ethambutol, Fluroquinolones, Gentamicin, Acyclovir.
Bonus: Which ones specifically are nephrotoxic and which are hepatotoxic?
Isoniazid (INH), Rifampin, Pyrazinamide, Ethambutol.
Bonus:
Heptatotoxic: Isoniazid (INH), Rifampin, Pyrazinamide
Nephrotoxic: Ethambutol
A postoperative patient receives an IV antibiotic with a half-life of 6 hours to prevent infection. The initial dose is 800 mg, administered at 0400 on April 10. When will 94% of the drug be eliminated?
Bonus: How much drug remains at 1600 on April 10?
94% of the drug is eliminated by 0400 on April 11.
Bonus: At 1600 on April 10, 200 mg remains in the body.
Which of the adrenergic receptor primarily mediates vasoconstriction in the peripheral blood vessels? Which would lead to bronchodilation?
Alpha-1
Beta-1
Beta-2
Alpha-2
Alpha-1
Beta-2
What are the two Hypercoagulability (hemostasis exaggerated/thrombosis) states?
1. Increased/Excessive Platelet Function (elevated lipids and cholesterol, smoking)
2. Accelerated Activity of coagulation (immobility, CHF, contraceptives)
What is the difference of Receptor Sensitivity Down-Regulation and Receptor Sensitivity Up-Regulation.
DOWN-Regulation is continual exposure to AGONIST, means receptor becomes desensitized. Develop tolerance to drug (loss of drug effect). UP-Regulation is continual exposure to ANTAGONIST so cells become hypersensitive.
What are two to three innate immunity cells? What are the two adaptive immunity cells?
Bonus: What does each cell do/ what process are they involved in?
Innate immunity: Neutrophil (first responders), macrophage (engulf and digest), mast cells (release histamine-trigger inflammation), dendritic, esinophils
Adaptive Immunity: B- lymphocytes- Produce antibodies (humoral immunity). T- lymphocytes- Cell-mediated immunity. (memory cells.)
hypomagnesemia manifestion? hypermagnesemia manifestion?
hypomagnesemia: 3 Ts: tremor, twitching, and tetany, altered LOC, arrhythmias.
hypermagnesemia: diminished deep tendon reflexes.
What is an adverse side effect of Clindamycin? What is the MOA of Clindamycin?
Its major adverse side effect is the promotion of C. diff superinfection.
Its MOA is bacteriostatic inhibitor of protein synthesis.
Describe the three methods of Renal drug excretion? Which excretion method does a majority of molecules undergo?
Bonus: What are 3 non renal ways of secretion?
Glomerular Filtration: Drugs filtered from blood into urine through capillary pore. (Protein bound drugs too big).
Passive tubular Reabsorption: Lipid-soluble drugs reabsorbed into the blood. (high to low conc.).
Active Secretion: Transport systems (P-glycoproteins) pump drugs from blood into urine.
Glomerular Filtration is the most common.
Bonus: Bile (enterohepatic recirculation) sweat, saliva, breast milk.
What is Bethanechol used to treat? What kind of drug is it? What is Atropine used for? What kind of drug is it?
Bonus: What kind of drug do you use to treat asthma?
To treat urinary retention and it is a muscarinic agonist. To treat bradycardia and it is a muscarinic antagonist.
Bonus: Beta 2 Agonist
What are the four stages of Hemostasis?
1. Vessel Spasm/ vascular injury
2. Formation of plug through Platelet adhesion
3. Coagulation Cascade (formation of fibrin clot)
4. clot retraction
What is the difference between a Non-Competitive Antagonist and a Competitive Antagonist?
A noncompetitive antagonist binding is irreversible and cannot be kicked off by an agonist. A competitive antagonist binding is reversible and can be kicked out by the next antagonist or agonist by increasing its concentration.
What physiologic changes cause erythema, heat, and swelling in inflammation?
Bonus: What are the first cells that are activated in the inflammation response?
Erythema and heat- increased blood flow from vasodilation.
Swelling- happens from increased vascular permeability so fluid flowing toward site of injury.
Bonus: Neutrophils
A nurse is caring for a client who has a pH of 7.50, PaCO2 of 30 mm Hg, and HCO3- of 22 mEq/L. Which acid-base imbalance is this client experiencing?
Respiratory alkalosis