This is how often the scrub person should change gloves during a procedure?
Every 60-150 minutes and after contact with bone cement.

This is the name of what should be done before each case to ensure that ALL evidence from the previous patient and procedure has been removed.
The Room Survey.
During a Malignant Hyperthermia (MH) Crisis, after the first dose is given, this is the amount of Dantrolene that you would give the patient if their symptoms were not resolving.
After initial dose, maintenance dantrolene should be continued (1mg/kg/dose every 4-6 hours). If the initial symptoms re-occur, another full dose is given.
This is the type of anesthesia used when making a skin incision or when administering nerve blocks.
Local anesthetics.
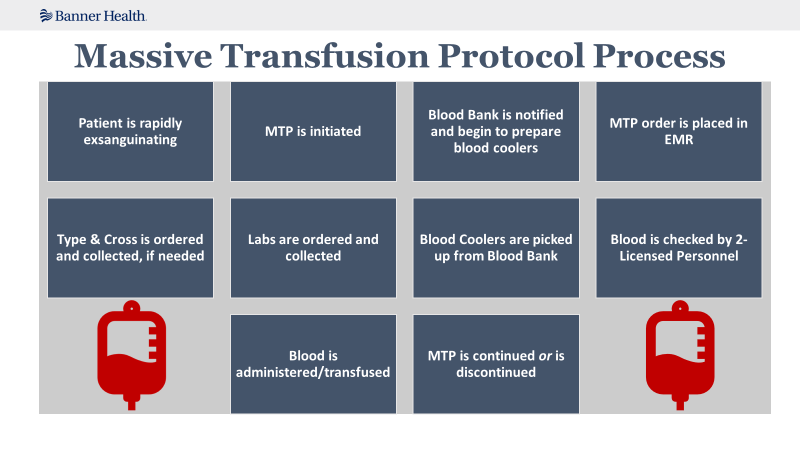
This protocol can be activated if the patient meets criteria for excessive bleeding.
Massive Transfusion Protocol (MTP).
This is the area of the gown that is considered sterile.
The chest to the level of the sterile field and the sleeves from 2 inches above the elbow to the proximal edge of the cuff.

This is how often horizontal surfaces in the OR should be damp dusted.
Before the first surgical procedure of the day

This is the type of sterile towel that would be considered a drape.

Impervious towel
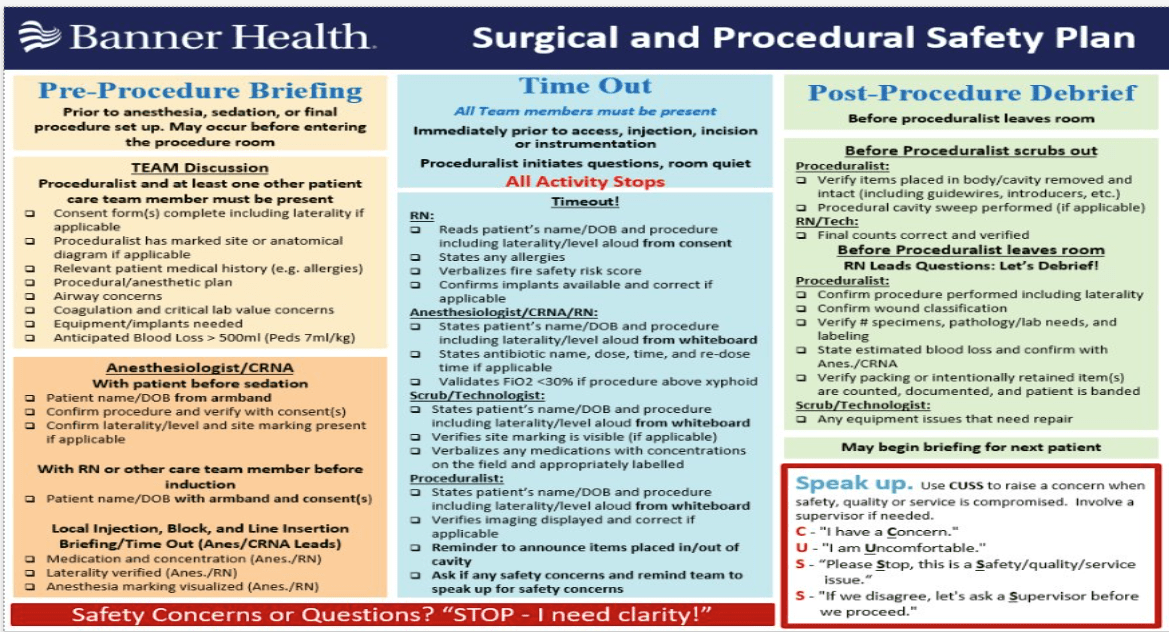
Consent etiquette is required when filling out consents. These are some items that you must be sure to check.
No abbreviations, must include laterality and levels, must match the order in the EMR, must be signed by the patient/patient representative and surgeon PRIOR to leaving PREOP.
This is the correct sequence when performing closing counts, starting with the patient/surgical wound.
From the patient/surgical wound, to the mayo stand, to the back table, to the kick bucket, to the sponge bags, to off the field.
These are known to be triggering agents.
Inhaled anesthetic agents or Succinylcholine.

These are some skin complications that can arise from local anesthetic infiltration.
Petechaie, Bruising, Hematoma, Soft Tissue Injury, and LAST.
These individuals are able to initiate the order of MTP.
Advanced Providers, MDs, DOs, Surgical Residents.
This is the element of the fire triangle that a laser belongs in.
Ignition
This is how you should protect the sterile field IF you have set up, but the case is unexpectedly delayed.
*The sterile field can be covered with sterile cuffed drapes
*A portion of the back table that will not be used immediately can be covered
*Remember to prepare the sterile field as close to the time of use as possible
This is how we can confirm the success of the biological indicator testing (BI).
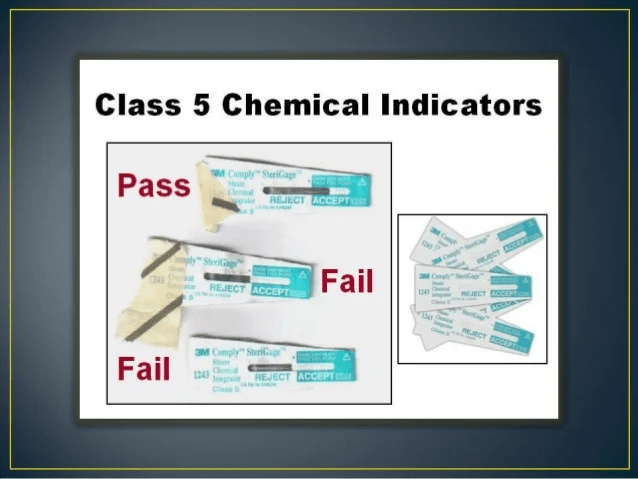
A BI vial that is unprocessed should produce a positive result after incubation.
This is how recent a history and physical must be updated for an inpatient surgical patient.
Within the last 24 hours.
This is what must be written on the white count board for any sponges being placed inside a cavity.
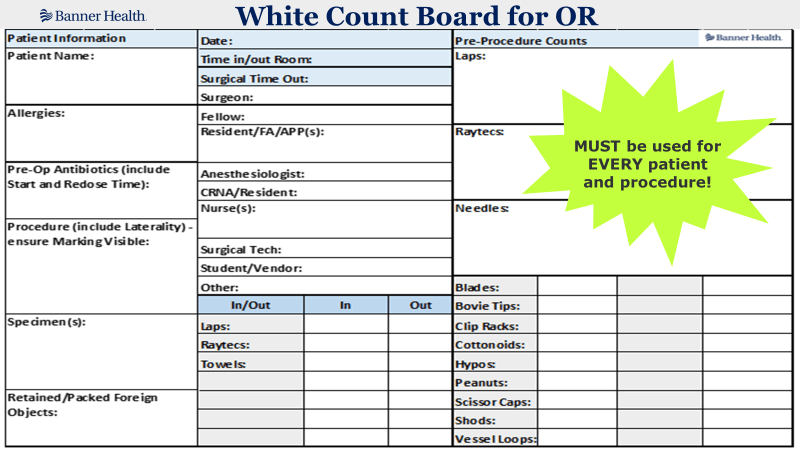
The number of items placed in the cavity and the number of items removed from the cavity. "Announce and Count"
This is an anesthetic agent that can be used in a patient with a history of MH.
Propofol.
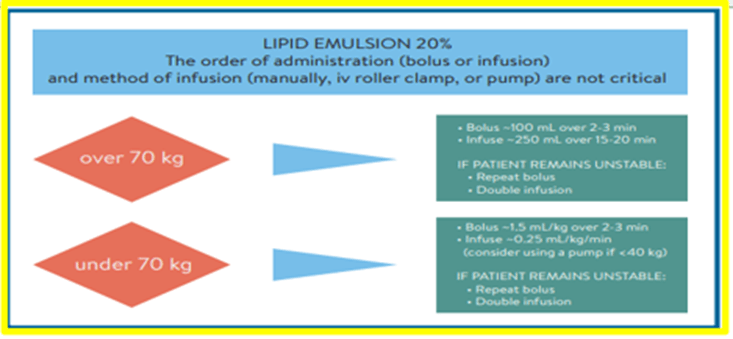
This is the reversal agent for Local Anesthetic Systemic Toxicity (LAST).
Intralipid 20%.
This is the criteria that needs to be met in order to initiate MTP.

Administration of 8-10 units of RBCs to an adult in less than 24 hours.
Acute Administration of 4-5 units of RBCs in one hour.
Pediatric patients who are requiring blood products for resuscitation.
The best practice you should do when you first enter the operating room space for the start of your shift.
Best practice is to perform a First Scrub of the Day.

This is the definition of an Accountable Care Organization.
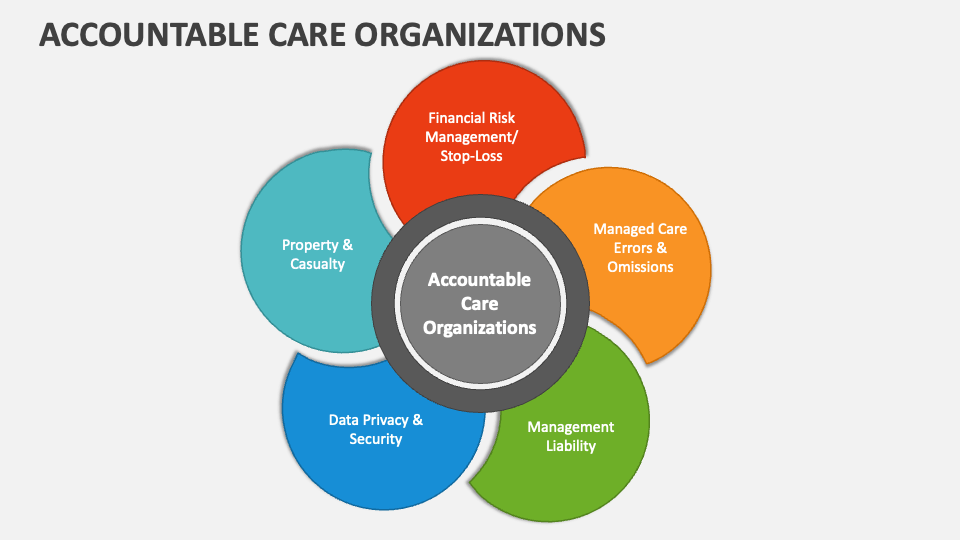
VOLUNTARY coordinated effort across health care specialties.
This is the type of risk factor for surgical patients who use Alcohol.
Exaggerated physiological stress response

This is what should be done before the patient's surgical site is marked.
Checking the physician's orders, checking the consent, asking the patient to verify the procedure, and checking imaging or radiologist's reports to confirm the procedure.
This is the name of the count that must be performed PRIOR to the patient entering the OR.

Initial or Baseline Count.
This is an EARLY sign of MH.
Increased ETCO2.
Sinus Tachycardia.
Masseter (jaw) rigidity.
Muscle rigidity.
This is a sign and symptom you may see in a patient exhibiting symptoms of LAST.
Tinnitus, Blurred Vision, Dizziness or Lightheadedness, Tongue Paresthesia.
This is the MTP process.
This is when we know it is safe for anesthesia to remove the ET or LMA?
When the patient is able to maintain their airway on their own.
This is how you would let your gown unfold if you were gowning yourself off the back table.

Step back from the back table and allow the gown to unfold.
This is what should be documented after surgery regarding skin antisepsis.

Hypersensitivity
This is how the surgeon should mark the site on the patient's skin.
Their initials. The way the surgeon marks the patient should be a consistent mark used throughout the hospital (IR, ICU, ED or anywhere procedures are done).

This is the type of sponge/towel that MUST be used for intentional packing.
RFID sponge or towel.
This is the first thing you should do if your patient is showing signs and symptoms of an MH Crisis.
Call for help!!

This is where your Intralipid 20% can be found.
In the Lipid Rescue Kit, PYXIS, and in Pharmacy.
This must be completed after the administration of blood products to the patient.

Transfusion Record and EMR Documentation.
This is what could negatively affect the sterility of an instrument.

Exposure to moisture.
This is the FIRST step in reprocessing surgical instruments after they have been used during a procedure.
Cleaning bioburden off instruments.
This is a skills-based error when done incorrectly by an RN.
Omits a section of the surgical safety checklist during the time out because of an interruption.
This is how the surgeon should mark a patient who has a cast on and is scheduled for an ORIF of the left wrist.

Surgeon's initials on the anatomical diagram.
This is the first thing you should do if you have an incorrect count.
Recount! Notify the surgeon it is incorrect.
These are the carts that must be in the room if your patient is showing signs and symptoms of an MH Crisis.
MH Cart and the Code Blue Cart!
Make sure you know where both are!
This is the available dose of Intralipid 20%.
250mL or 500mL. Please be sure you where and how much of this is kept at your facility.
This is who must be notified with either the continuation or the discontinuation of MTP.
Blood Bank.
This is a complication we are concerned about when a patient is in the Trendelenburg position for an extended period.

Increased intraocular pressure.
This is when biological monitoring should never be used.

In IUSS (Immediate Use Steam Sterilizers)
This is what stage pressure injury that should be documented if the patient has painful skin that is abraded, blisters, or has shallow crater.
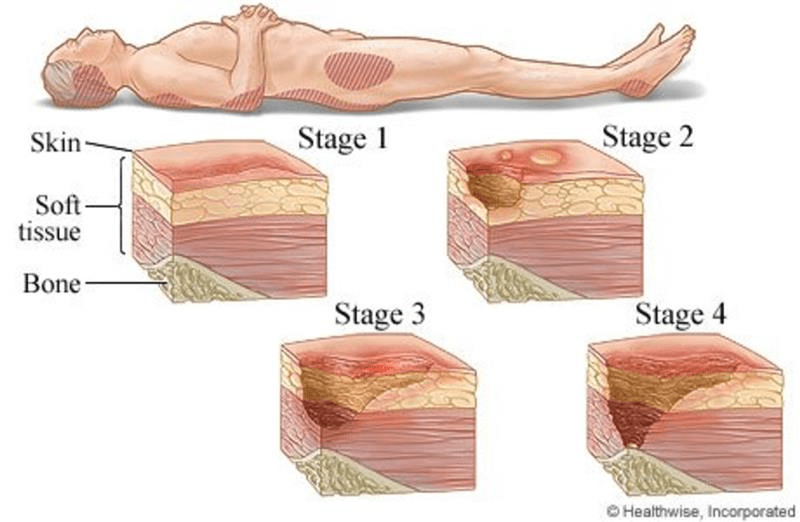
Stage 2
This is a characteristic of patient and family centered care. Name as many as you can!
Alliance between health care practitioners, the patient, and the patients support system
Focus on communication with everyone who is involved in the patient's care (patient and family)
Patient and family participation in care
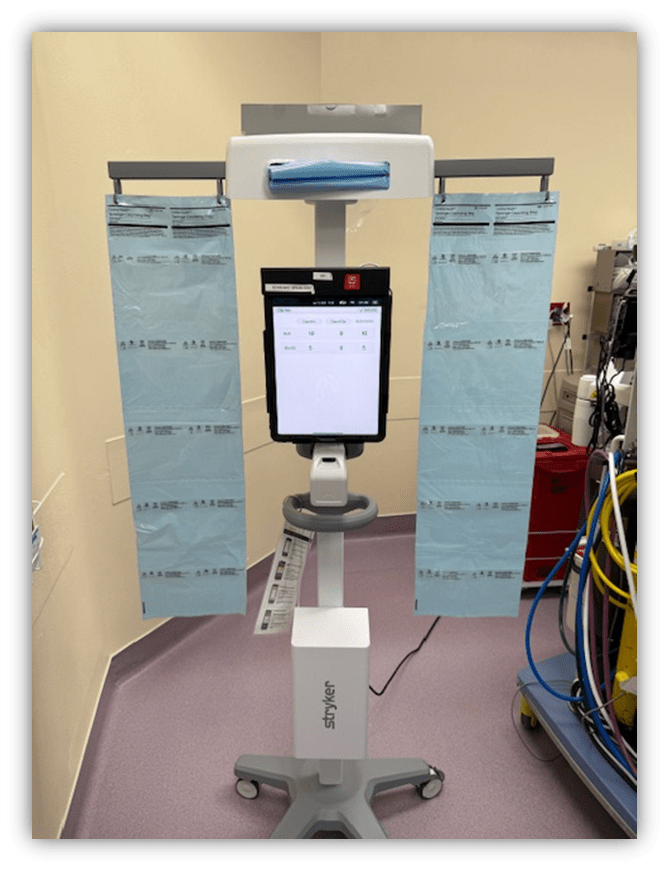
There is a miscount. This is what must be done if the room and patient have been searched using the SurgiCount reader and the count is still off.
Intraoperative imaging MUST be taken.
This is the name of the professional organization you should also call during an MH Crisis.
MHAUS
MHAUS Hotline
1.800.644.9737
1.800.mh.hyper
This is another name for Intralipid 20%.
Liquid Emulsion OR Fat Emulsion.
This is how often vitals are taken while the patient is receiving MTP.
Continuously, every 15 minutes during transfusion, if not more frequently.

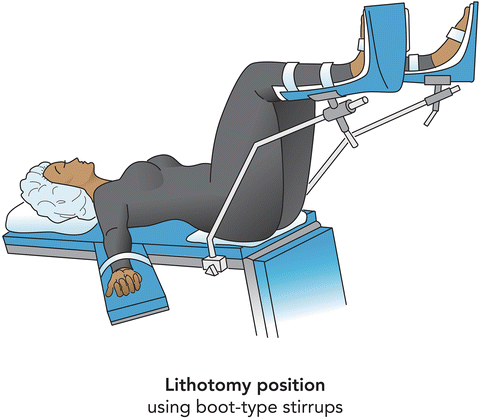
This is the most likely physiological effect that can occur when a patient is in the lithotomy position.
Hip dislocation.
This is the wound class that you would document if you were in a laparoscopic appendectomy and the surgeon encounters purulent inflammation of the appendix.
Wound Class IV

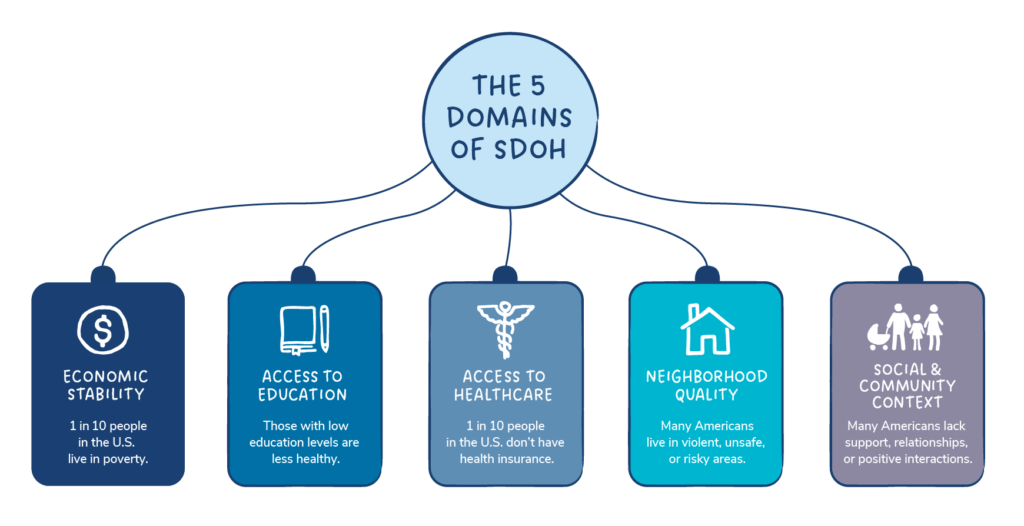
This is the Domain (SDOH) that associated with employment, food, housing and poverty.
Economic stability
This is what the OR RN should do if they are taking their patient to surgery, but the patient's site has not been marked AND there is also no Anatomical Diagram.
STOP and have it completed.

This is what we do when someone interrupts the visual and audible counts between the circulator and the scrub.
Restart! Pause for the Gauze!
This is how many mg's are in a vial of dantrolene. This is how many mg's are in a vial of ryanodex.
20 in dantrolene and 250 in ryanodex
This is where your patient should be transferred to after an occurrence of LAST.
ICU or higher level of care.

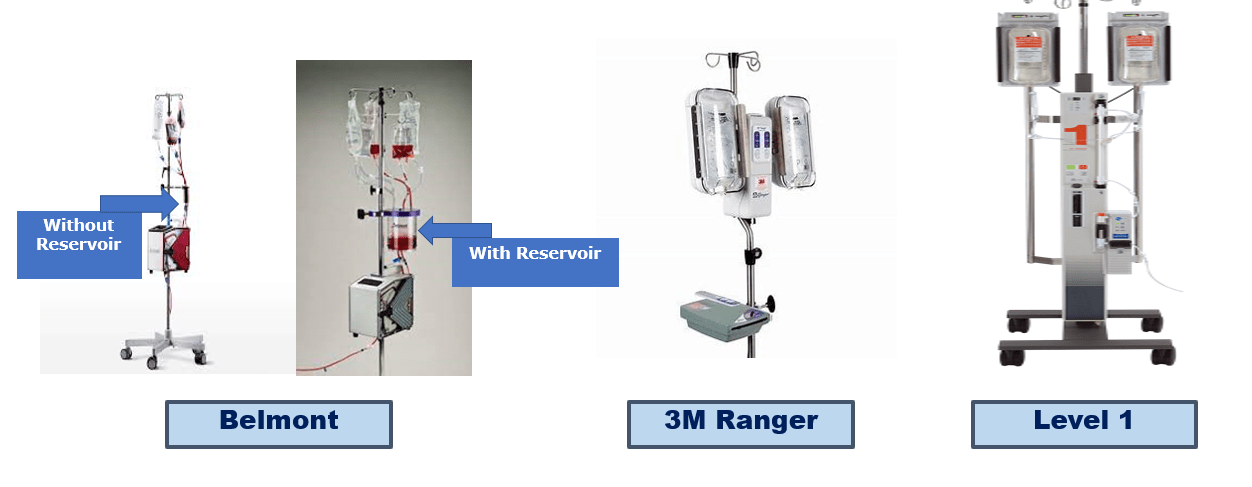
These are the names of the equipment that is used for rapid blood infusion.
Belmont, 3M Ranger, Level 1.
This is how to determine how long a wrapped item on the shelf in the core is sterile.

Sterility of wrapped items is Event Related for wrapped items and 5 years for heat-seal pouches and 3 years for self seal pouches.
Dropping it on the floor, moisture detected on the packaging, rips or tears in the packaging.
This is the phase of healing where hemostasis, phagocytosis and edema occur.
Inflammation.
This is a way to describe what health disparity means.

Higher burden of some populations.