What "pressure" causes fluid to move out of capillaries contributing to edema in heart failure?
What is increased hydrostatic pressure?
A patient has sudden swelling and pain in one leg after a long flight. What’s the most likely cause?
What is DVT?
A 50-year-old woman has new swelling in both legs. She recently started taking amlodipine for high blood pressure. Her lungs are clear and JVP is normal.
What is the most likely cause of her edema?
What is medication side effect from the amlodipine, amcalcium channel blocker?
Dihydropyridine calcium channel blockers (like amlodipine) commonly cause dose-dependent bilateral leg edema due to arteriolar dilation, which increases capillary hydrostatic pressure; not volume overload.
That’s why patients often have normal heart and lung exams.
What score test is used to assess probability for DVT before ordering imaging?
What is the Wells score?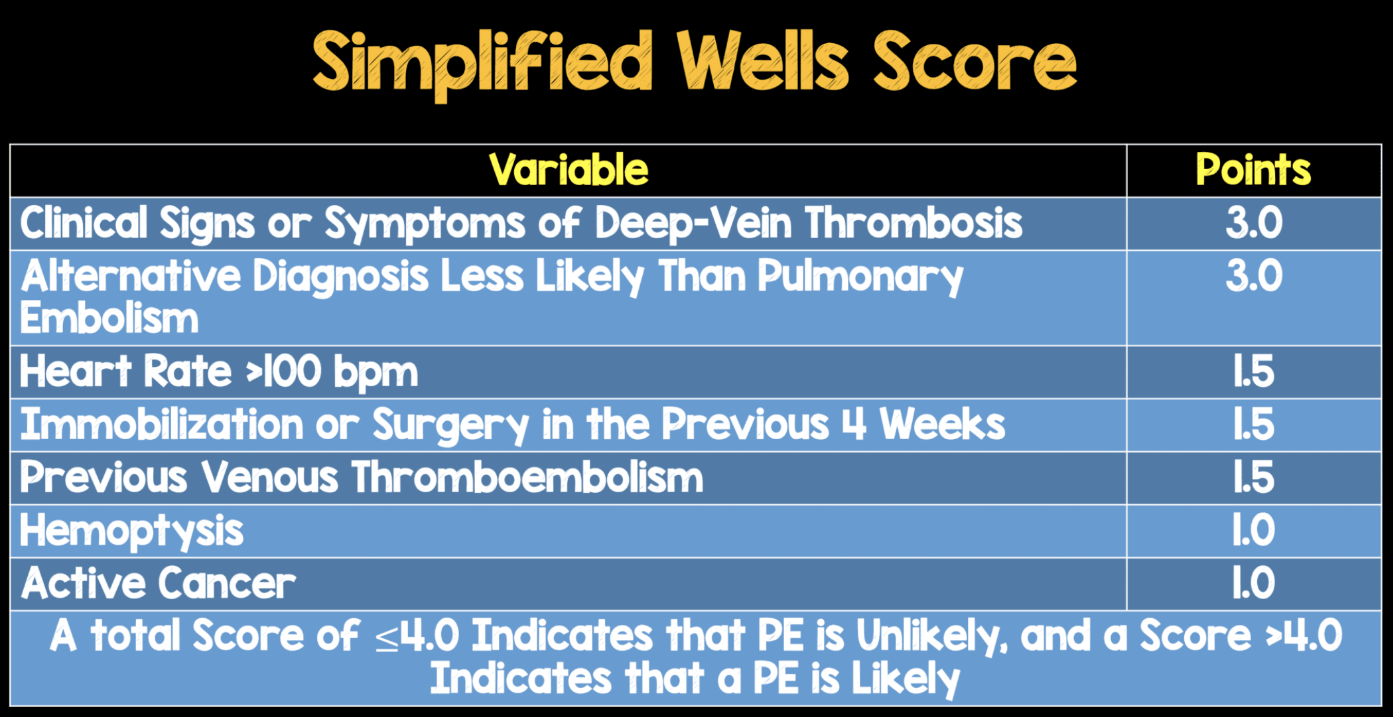
A 70-year-old woman is brought to the ER with severe confusion, hypothermia, and slow heart rate. On exam, she has dry skin, a puffy face, and non-pitting edema of the hands and feet. Her daughter says she stopped taking her thyroid medication weeks ago.
What life threatening condition should you suspect?
What is myxedema coma?
Which mechanism is responsible for edema in liver failure because of low albumin production?
What is decreased oncotic pressure?
What imaging test is used when you think a patient might have lymphedema?
What is lymphoscintigraphy? MRI can also be helpful.
A 40-year-old man presents with leg swelling, frothy urine, and periorbital puffiness. Labs reveal hypoalbuminemia and heavy proteinuria.
What is the most likely diagnosis?
What is nephrotic syndrome?
Nephrotic syndrome causes edema due to low oncotic pressure from protein loss. Periorbital swelling is a subtle but classic clue especially in the morning.
This test can indicate the presence of a blood clot if elevated.
What is a D-dimer?
Which serious soft tissue infection typically caused by Streptococcus pyogenes should be suspected in rapid swelling of the lower leg with blackening of the skin, blisters filled with pus, crepitus, and fever?
What is necrotizing fasciitis?
Which mechanism results in edema seen in sepsis or anaphylaxis?
What is edema due to increased capillary permeability?
Name two causes of long term swelling in one leg (not including DVT).
What are chronic venous insufficiency, lymphedema, or a pelvic mass pressing on veins?
A 32-year-old woman at 34 weeks gestation presents with bilateral leg swelling that's been gradually worsening. Vitals: BP 118/76, HR 82. She denies headaches, vision changes, abdominal pain, or shortness of breath. Urinalysis is negative for protein. Lungs are clear. There is 2+ pitting edema in both legs.
What is the most appropriate next step in management?
What is reassurance and routine prenatal care?
In late pregnancy, bilateral pitting edema is common and usually benign because the uterine pressure on the inferior vena cava reduces venous return from the legs. The key is to rule out preeclampsia (look for HTN and proteinuria). No additional testing is needed if vitals and urine are normal, and there are no alarming symptoms.
What imaging would you order if you highly suspect DVT?
What is a venous ultrasound?
A 62-year-old woman presents with sudden, severe pain and swelling in her left leg. The leg appears dusky blue, is tense to palpation, and she has a history of prior DVT. Her vital signs show tachycardia and borderline hypotension.
What is the likely diagnosis causing this limb-threatening presentation?
What is phlegmasia cerulea dolens?

Phlegmasia cerulea dolens is a massive DVT causing near-complete venous outflow obstruction → severe congestion, ischemia, and risk of limb loss. It's a vascular emergency that requires urgent vascular surgery or interventional radiology consult.
How would you describe this finding?
What is pitting edema?
Pitting edema occurs from low protein fluid. The fluid is watery and low in protein so when you press on the skin, it displaces easily making a pit. It's seen with CHF, nephrotic syndrome and cirrhosis.
Non-pitting edema is seen in lymphedema, myxedema, or long-standing chronic edema. The fluid is rich in proteins (thicker and more gelatinous) so its harder to compress leaving no pit when you press on the skin.
A 65-year-old patient presents with sudden swelling and discomfort in the back of the knee that has now moved into the calf. There is no redness, fever, or history of trauma. Ultrasound shows fluid extending down the leg but no signs of DVT.
What is the most likely diagnosis?
What is a ruptured Baker’s cyst?
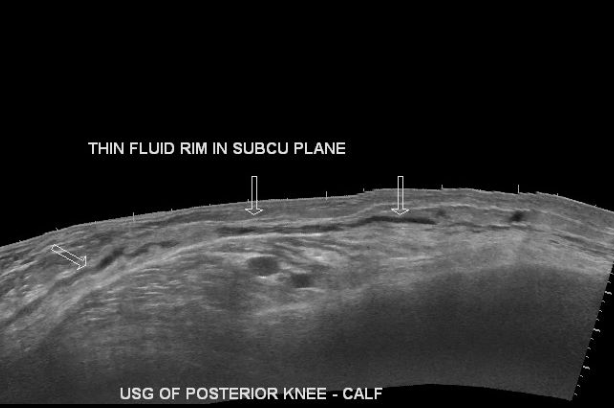
A ruptured Baker’s cyst can mimic DVT but usually presents with calf pain and swelling without systemic signs. Ultrasound can show fluid tracking along the calf muscles, and there's no vein compression.
A 58-year-old man with alcohol-related cirrhosis presents with progressive bilateral leg swelling and abdominal distension. He has no chest pain or shortness of breath. Vitals are stable. Exam shows tense ascites and 2+ pitting edema in both legs. Labs: Na 129, albumin 2.3, creatinine 1.1, AST 88, ALT 40.
What is the most appropriate initial treatment for his edema?
Spironolactone (aldosterone antagonist) + furosemide (loop diuretic)
In cirrhosis, portal hypertension and low albumin lead to activation of the RAAS system → increased aldosterone. This causes sodium and water retention. Spironolactone is an aldosterone antagonist → directly counteracts the main driver of fluid retention in cirrhosis. First-line diuretic for ascites in cirrhosis.
Furosemide is loop diuretic → promotes potent natriuresis and diuresis and helps manage volume overload more quickly.
What are the two key findings on compression ultrasound for diagnosing DVT?
What is noncompressible vein and lack of flow augmentation?
A patient presents with bilateral leg edema, elevated JVP, orthopnea, S3 heart sound and bibasilar crackles on auscultation.
What is the next best test to confirm the suspected diagnosis?
What is an echocardiogram and/or BNP?
Echocardiogram is the diagnostic test. BNP is supportive.
A patient with pancreatic cancer presents with progressive bilateral leg swelling. Imaging reveals extensive retroperitoneal lymphadenopathy compressing major vessels. Labs show normal albumin and kidney function.
Which pathophysiologic mechanism is primarily responsible for this patient’s edema?
What is lymphatic obstruction?
Lymphatic obstruction causes non-pitting edema and can result from malignancy, surgery, radiation, or infection. It leads to the accumulation of protein-rich fluid in the interstitial space and typically doesn’t respond to elevation or diuretics.
You suspect a DVT in a patient with sudden leg swelling and tenderness. Their first leg ultrasound is negative, but they’re still very symptomatic.
What’s the next best step?
What is repeat the ultrasound in 5–7 days?
Early DVTs may not be visible on initial ultrasound. If clinical suspicion remains high, a repeat scan is important to catch a clot that may have formed or extended after the first test.
A 54-year-old woman presents with gradual, painless bilateral leg swelling. She denies shortness of breath or weight gain. Her legs are symmetrically enlarged, soft, and tender to touch, but her feet are spared. No improvement with elevation.
What is the most likely diagnosis?
What is lipedema?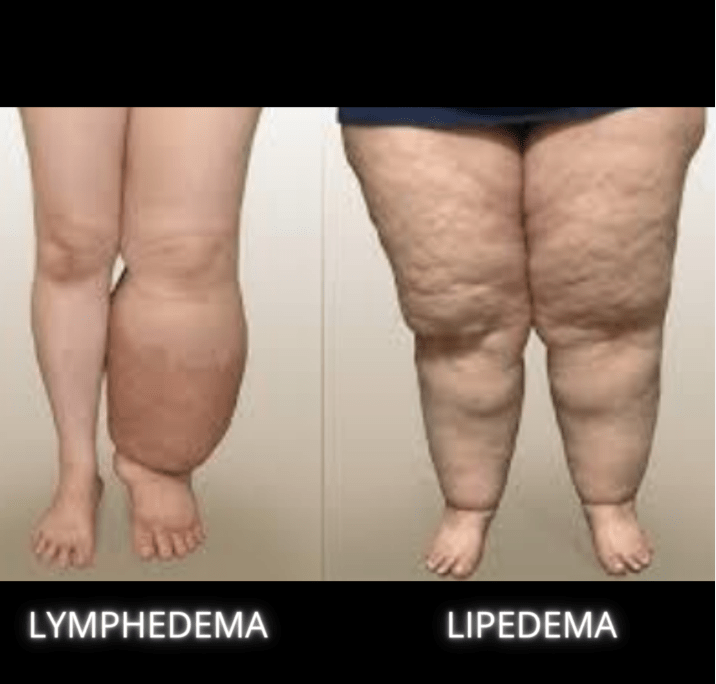
Lipedema is often misdiagnosed as obesity or lymphedema. It affects women, involves fat accumulation in the legs, and spares the feet. It causes tenderness, is symmetrical, and doesn’t respond well to diuretics or elevation.
A 69-year-old man presents with unilateral leg swelling. Duplex ultrasound is negative for DVT, but symptoms persist. On further questioning, he mentions mild left lower abdominal pain and difficulty urinating.
Which imaging study should be ordered next, and what are you looking for?
What is CT abdomen and pelvis to evaluate for a pelvic mass compressing venous return?
When DVT is ruled out but unilateral edema persists, think about external compression (pelvic or retroperitoneal mass, iliac vein thrombosis). A CT or MRI can reveal masses or deep pelvic pathology not seen on leg ultrasound.
A 35-year-old construction worker is brought to the ED after being trapped under debris for over an hour. He has severe swelling of his right lower leg, which is tense, tender, and increasingly painful. Pain worsens with passive dorsiflexion. His foot feels cool, and dorsalis pedis pulse is faint. What is the most urgent test/imaging?
What is measure compartment pressures?
Suspect compartment syndrome following a acute crush injury. Normal is below 10. If exceeds more than >30 indicative of acute compartment syndrome.