Typically the most affected region in unilateral ACA stroke
What is the contralateral leg (motor and sensory)
can also affect bowel/bladder (paracentral gyrus) and executive fxn if b/l or hypoplastic vessels/weird anatomy
A patient with impaired fluency, intact comprehension, and impaired repetition has this type of aphasia.
What is nonfluent aphasia (Broca's aphasia)?
The H-reflex on NCS is most commonly used to assess for this condition
What is S1 radiculopathy?
The rotator cuff is comprised of these muscles.
What are the Supraspinatus, Infraspinatus, Teres Minor, and Subscapularis?
This level on the Ranchos Los Amigos scale refers to patients exhibiting confused and appropriate behavior.
What is level VI?

SBP goals for ischemic and hemorrhagic strokes respectively
What is SBP <220, SBP<140?
Return to normotension over days to weeks
These scores on the Galveston Orientation and Amnesia Test (GOAT) and Orientation-Log (O-Log) represent emergence from Post-Traumatic Amnesia? (100pts each)
What is at least 75 for two consecutive days on the GOAT and at least 25 for two consecutive days on the O-Log?
Injury to this nerve causes lateral scapular winging
What is the spinal accessory nerve (CN XI)?
Trapezius weakness
True Leg length discrepancy is assessed by measuring between these two bony landmarks.
What is the ASIS and medial malleolus?
Note, apparent leg length is measured from umbilicus and medial malleolus
At this stage of Brunnstrom's stroke recovery process, spasticity begins to decrease
What is stage 4?

The three most commonly affected areas of the brain with lacunar strokes. (100 pts per answer)
What is putamen, thalamus, internal capsule?
These are the ICP and CPP goals in TBI management
What is ICP<20, CPP>60?
CPP = MAP - ICP
Entrapment of the suprascapular nerve here causes isolated infraspinatus weakness.
What is the spinoglenoid notch?
This is a fracture resulting from excessive pronation-external rotation of a planted foot:
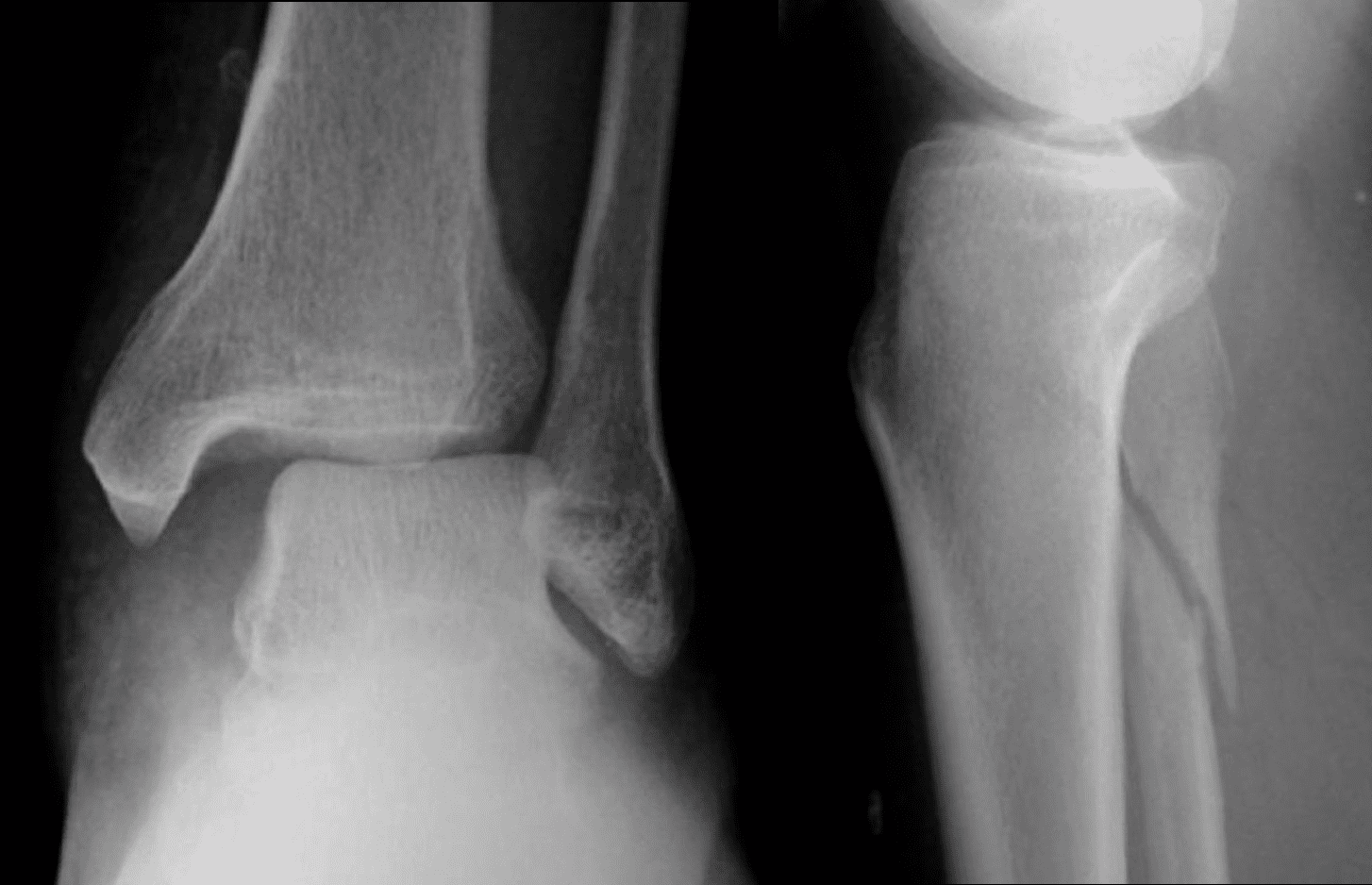
What is a Maissonneuve fracture?
Combination of proximal fibular fracture and distal talofibular syndesmotic injury (widening) can include medial mal fx
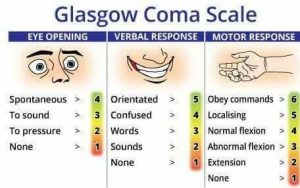
A trauma patient who opens his eyes when spoken to, uses nonsensical words, and pulls his fingers away from you when the nailbeds are pressed has this GCS score.
What is 10? (Motor 4, verbal 3, eye 3)
This stroke syndrome can present with hoarse voice, dypshagia, ipsilateral ataxia/nystagmus, ipsilateral horner syndrome
What is Wallenberg Syndrome (lateral medullary CVA)?
"Dr. Wallenberg at the VA says don't PICA horse that can't eat"
Can also see intractable hiccups (involvement of expiratory area in the medulla, dorsal motor nucleus of vagus n, and nucleus ambiguus can result in disregulated respiration/involuntary inspiration)
Alexia without agraphia can occur with a lesion here, (include the side)
What is the dominant PCA territory?
Infarct of splenium of corpus callosum so language centers are intact but unable to receive information from contralateral visual cortex and visual word form area may be disrupted
This is considered the only muscle innervated by single cervical nerve root
(name the muscle, root, and peripheral nerve; 100pts each, 400 if all)
What is the rhomboid major?
C5, Dorsal Scapular Nerve
The Rockwood classification of an AC joint injury with complete rupture of both the AC and CC ligaments, and superior displacement of the clavicle, and increased CC distance of 25-100% relative to the contralateral side.
What is type III?

LIn TBI patients, severe disability is unlikely when the duration of post-traumatic amnesia (PTA) is less than this amount of time.
What is 2 months?
PTA
Severe disability unlikely when <2 months
Good recovery unlikely when >3 months
Coma
Severe disability unlikely when <2 weeks
Good recovery unlikely when >4 weeks
This is the specific type of vision loss expectd with a unilateral PCA infarct. (300pt);
This is the name of the syndrome resulting from a bilateral PCA infarct (200pts)
What is homonymous hemianopsia with macular sparing?
What is Anton syndrome? (Cortical blindness with denial)
These are the midline structures in Rule of 4's
(100pts each, 500 if all)
What are the motor (Corticospinal) tract, Medial Lemniscus, Motor Nuclei 3,4,6,12, and MLF?
Side structures: What are the STT, Spinocerebellar tract, Sensory nucleus of 5, Sympathetics
This would be the most appropriate interpretation of an EMG with spontaneous potentials and large amplitude/large duration motor units in pronator teres, FCR, and cervical paraspinals; but normal needle EMG findings in deltoid, biceps brachii, triceps, and FDI.
What is an acute (active denervation) on chronic C6 radiculopathy?
Timeline of findings?
A complete fracture of the femoral neck with partial displacment would be this stage on the Garden classification.
What is stage III?
I: Incomplete, nondisplaced
II: Complete, nondisplaced
III: Complete, Partially displaced, capsule intact
IV: Complete, Completely Displaced, capsule ruptured

This rehabilitation approach, also known as the neurodevelopmental technique, aims to inhibit primitive reflexes, avoid use of synergistic movement, and facilitate automatic reactions with subsequent normal development.
What is the Bobath technique?
Rationale- patient's may never advance past synergy patterns if not forced to do controlled/fine motor
Which approach uses Synergy as part of therapy?