-Kinetics
OTC use of medications is nearly 60% of all drugs on the market. The FDA regulates these as these are the requirements (Indication for use and Safety profile).
Consumer must be able to easily:
-Diagnose condition
-Monitor effectiveness
-Benefits must outweigh risks
Drug should have:
-Limited interaction with other drugs
-Low potential for abuse
-High therapeutic index
We see polypharmacy ALOT in medicine, what is this term and who do you see it often with?
Polypharmacy-The concurrent use of multiple medications (typically 5 or more); typically seen with elderly patients.
Often times additional medications are to treat the side effects of initial medications prescribed.
What is a schedule V drug?
Schedule V - Lowest potential for abuse:
Robitussin AC with codeine, lyrica, Lomotil (treats diarrhea) -has morphine derivative that helps with nerve pain
What are all the steps involved with Pharmacokinetics?
Absorption: The rate at which a drug leaves its site of administration and enters the bloodstream for distribution to body tissues.
Distribution: The transport of a drug in the body by the bloodstream to its site of action
Metabolism:
The biologic transformation of a drug into: an inactive metabolite, a more soluble compound, a more potent metabolite
Elimination: The elimination of drugs or metabolites from the body
What are signs and symptoms of infection?
•Fever
•Chills
•Sweats
•Redness
•Pain
•Swelling
•Fatigue
•Weight loss
•Increased White Blood Cell (WBC) Count
•Pus
Sulfonamindes like Bactrim are effective for UTIs and ear infections, what potential side effects and teaching aspects do you provide to your patient?
SE: diarrhea, nausea, vomiting; crystalluria, toxic nephrosis; anemia, thromboycytopenia; Stevens-johnson syndrome, photosensitivity
Edu:
•Should be taken with at least 2000-3000 mL of fluid
per day, unless contraindicated.
•Due to photosensitivity, avoid sunlight and
tanning beds.
•These agents reduce the effectiveness of
oral contraceptives.
•Take with food to decrease GI upset
TB is a slow growing bacteria that may become dormant. You can diagnose a patient with TB through these exams.
1.TB skin test
2.If skin test is positive, then chest x-ray
3.If chest x-ray shows signs of TB, then culture of sputum or stomach secretions is obtained
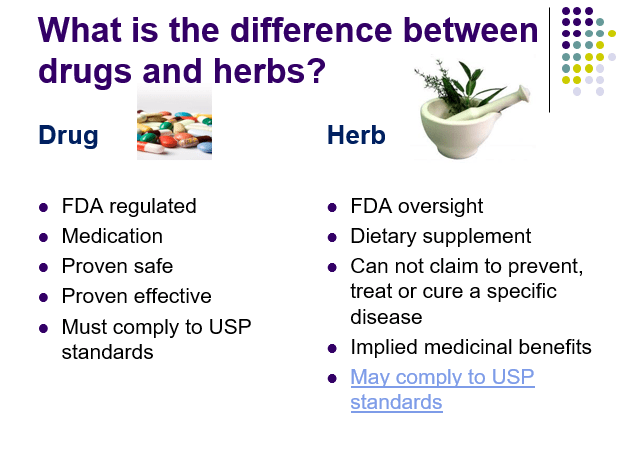
OTC use of both medications and drugs are common in patients. What is the difference between these two?
What is the difference between Pharmacokinetics and Pharmacodynamics?
Kinetics (korpse-what the body does to the drug)
Dynamics (drug-what the drug does the body)
What is a Scheduled IV drug?
Schedule IV - Low potential for abuse:
Xanax, Valium, Ativan, Ambien, Tramadol
What organs are involved with Metabolism?
Liver (main organ), skeletal muscle, kidneys, lungs, plasma, intestinal mucosa
What are the differences in these types of therapies? Empiric, Definitive, and Prophylactic
Empiric therapy: Broad spectrum vs narrow spectrum antibiotics
Definitive therapy: Most narrow spectrum, least toxic drug to meet culture/sensitivity results
Prophylactic therapy: Prevent
Penicillins are often combined with beta-lactamase to create a stronger antibiotic. What potential adverse and side effects do you look for as well as educate your patient with?
Adverse & Side Effects:
•Nausea, vomiting, diarrhea, abdominal pain, superinfections, colitis
•Allergic Reactions: common = urticaria, pruritus, & angioedema
•Idiosyncratic reactions occur, i.e. Stevens-Johnson Syndrome
Edu:
•Any patient taking a penicillin should be carefully monitored for an allergic reaction for at least 30 minutes after its administration.
•The effectiveness of oral penicillins is decreased when taken with caffeine, citrus fruit, cola beverages, fruit juices, or tomato juice.
•Alternate form of oral contraception
What treatment is utilized in TB?
Multidrug Therapy:
•4 antibiotics administered at the same time
•Often 24 months of drug therapy
•Adherence to drug regimen
•Around the clock
Primary Agents:
•Isoniazid (INH)
•Rifampin
•Ethambutol or streptomycin
•PZA (pyrazinadmide)
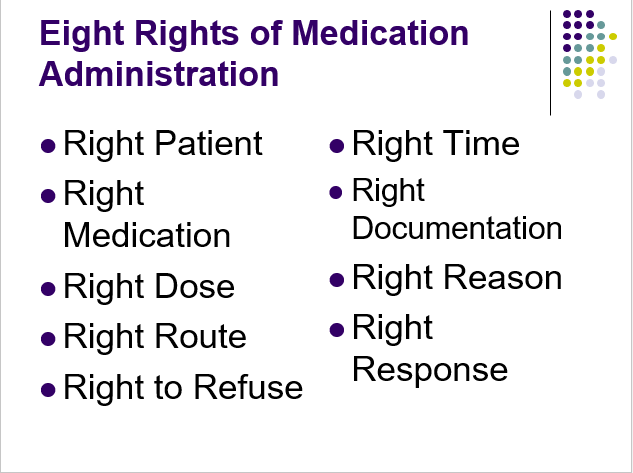
What is the nursing process in regards to medication administration? What is involved with each step?
Assessment, Diagnosis, Outcome Identification, Planning, Implementation, and Evaluation
What is an agonist and what does the antagonist do?
Agonist interacts with a receptor to produce a response
Antagonist has no specific pharmacological action of its own, but interacts with receptor to prevent the action of an agonist
What is a scheduled III drug?
Schedule III- Lower potential for abuse than Schedules I and II:
Tylenol with codeine, ketamine, anabolic steroids, testosterone
What organs are involved with Elimination and who do we consider dosing adjustments for?
Kidneys, respiratory tract, breast milk, saliva, and sweat
Renal dosing: adults and young children
How do you fight antibiotic resistance? (Don't be like Christy's mom.)
•Vaccinate
•Prevent conditions that lead to infections
•Get the unnecessary devices out
•Know when to say “no” to antibiotic use
•Treat infection ONLY
•Finish full course of prescribed antibiotic(s)
•Isolate the pathogen – Use isolation precautions
•Perform hand hygiene, perform hand hygiene, perform hand hygiene
There are 5 generations of Cephalosporins. What other antibiotic class are you considering?
Penicillins
What are adverse effects and teaching consideration for TB treatments INH and Rifampin?
Isoniazid
•Pyridoxine deficiency
•Peripheral neuropathy
•Liver toxicity
Rifampin
•Red-orange-brown discoloration of urine, tears, sweat, & sputum
•May decrease effectiveness of oral contraceptives
Edu: Coloring of secretions, Supplementation of VB6, oral contraceptive alternatives.
*Note* These are limited to the resources you have. Some say there are only 5 rights, some say 9.
What are indicated with NARROW therapeutic indexes?
Window/Index can be very narrow=doesn't work vs toxic
Peak concentration(highest level predicted)
Trough concentration (lowest, drawn before drug is administered)

What is a scheduled II drug?
Schedule II - High potential for abuse but currently has an accepted medical use in the U.S:
meperidine, morphine, cocaine, oxycodone, methadone, secobarbital, codeine, amphetamines, Vicodin,, fentanyl, Adderall, ritalin
What is a half life and steady state of a drug? What if the half life of a drug was 5 hours, when would I expect the steady state?
Drug Half Life: The time it takes for one half of the original amount of a drug in the body to be removed. A measure of the rate at which drugs are removed from the body.
Steady State: After approximately five half-lives, most drugs are considered to be effectively removed from the body. Physiologic state in which the amount of drug removed via elimination is equal to amount of drug absorbed with each dose.
5 hours=100%
10 hrs=50%
15 hrs=25%
20 hrs=12.5%
25 hrs=6.25%
What are the general teaching points as a nurse for antibiotic use?
•Assess for ALLERGIES!
•The most COMMON side effects of antibiotics are nausea, vomiting, and diarrhea.
•Assess for potential drug and/or food interactions.
•All oral antibiotics are absorbed better if taken with at least 6 to 8 ounces of water.
•Take antibiotics AROUND THE CLOCK for best results.
•Back up method of oral contraception
Macrolides like azithromycin is often used for STIs. What side effects do you consider along with teaching aspects?
SE:
•Chest pain, hypotension, palpitations, prolongs QT interval
•Abdominal pain, diarrhea, nausea, vomiting
•Hepatotoxicity, jaundice, anorexia
•Superinfections: vaginitis, stomatitis, thrush, c-diff
Edu: The absorption of oral macrolides is enhanced when taken on an empty stomach, but because
of the high incidence of GI upset, many agents
are taken after a meal or snack.
Antifungal drugs are used to treat fungal infections, these can often occur as a superinfection if the normal human flora has been adjusted by antibiotics. What classes of medications are utilized.
•Polyenes: Amphotericin B and nystatin
•Imidazoles: Ketoconazole, miconazole, clotrimazole
•Antimetabolic antifungal: Flucytosine
•Antiprotozoal agents: atovaquone
Identify this prescription:
cetirizine/Zyrtec 10 mg PO prn daily
Define the following: Subtherapeutic, Minimum Effective Concentration, Minimum Toxic Concentration, and Therapeutic (desired dose)
Minimum Effective Concentration (MEC): dose and interval to permit the plasma level to be above the minimal level required to elicit a pharmacological response" Just enough"
Minimum Toxic Concentration (MTC): The dosage and interval must permit the plasma level to be below the minimum toxic concentration.
Subtherapeutic: symptoms are still present and the current dose is not effective. Goal is to increase the dose or change the drug (per provider).
Therapeutic dose: The expected outcome of the drug that is optimized in the way we expect/want it to for the patient.
What is a scheduled I drug?
Schedule I - High potential for abuse & NO accepted medical use in the U.S.:
heroin, LSD, marijuana, peyote, hashish, ecstacy
What are factors that affect Distribution?
Protein-binding: "carriers" to their jobsite to work
Water vs fat soluble: water soluble= highly protein bound (slow) vs. fat soluble=poor protein bound (faster)
Blood-brain barrier: Water soluble drugs enter slowly
Organs: heart, liver, kidneys, brain vs. muscle, skin, fat
Bactericidal: Kill bacteria
Ex) Cephalosporins, polymxin and vancomycin
Bacteriostatic: Inhibit growth of bacteria that eventually leads to their death
Ex)Sulfonamides, erythromycin and lincomycin
Tetracyclines can target both gram positive and negative pathogens. This class of antibiotics has very specific contraindications and interactions. How do you educate your patient?
Interaction: Strong affinity for calcium
Contraindications: pregnancy and children under 8 years old. Hepatic and renal disease as well.
Edu: Contact the office if pregnancy is considered, use alt. form of contraceptive, avoid dairy products, and take on an empty stomach.
What is the education you would provide to your patient about the differences in Nystatin versus Amphotericin?
Nystatin-Topical infection like candidiasis
Amphotericin-Systemic infection given IV for progressive and fatal fungal infections.
-SE: fever/chills, nausea/vomiting, allergic reactions
Med error reporting is crucial to the safety of our patients and nurses. Define each one of these for me: Actual errors, Near misses, and Close call
Actual Errors: Giving a patient the WRONG medication/dose
Near Misses: event or situation that did not produce injury but only b/c of chance. NO patient injury due to luck.
Close Call: an event or situation or error that took place but was identified and captured prior to reaching the patient. Error was found prior to reaching the patient.
Define the following effects of medications: side effects, adverse effects, toxic effects, idiosyncratic, and additive effects
Side effects: effects of the drug that is not intended, can be predicted
An adverse outcome of drug therapy in which a patient is harmed in some way. Some adverse drug reactions are classified as side effects: Expected, well-known reactions that result in little or no change in patient management and Predictable frequency. The effect's intensity and occurrence are related to the size of the dose
Toxic effects- related to the dose of drug administered. All drugs are capable of producing toxic effects.
Idiosyncratic reaction are the result of abnormal reactivity to a drug caused by genetic differences between the client and nonreacting individuals
Additive Effects: potential of increased side effects
Scheduled drugs are enforced by which agency? And which schedule is not allowed refills on the script?
Drug Enforcement Agency (DEA):
The DEA regulates who can write prescriptions, manages refills for scheduled medications (Schedule II med refills are not allowed), Schedule II Meds must be hand written or electronically sent to pharmacy through DEA software (Cannot call in); ePDMP
What are all the factors that affect absorption?
Routes: Enteral, Parenteral, SQ, IM, IV Topical.
Foods: empty vs full (delay)
Dose/formulation: EC, controlled released
Absorptive surface
Blood flow to Small Intestine
GI motility
Fluoroquinolones like Cipro are often used for skin infections, what are the adverse effects to watch for as well as teaching aspects for your patient?
Adverse Effects: SEIZURES, Dizziness, headache, insomnia, DYSRHYTHMIAS: Prolongs QT interval, Pseudomembranous colitis, STEVEN’S JOHNSON SYNDROME, Abdominal pain, diarrhea, nausea, Peripheral neuropathy, Photosensitivity
Edu: Fluid intake, avoid dairy as it can decrease absorption, renal labs will be obtained and monitored, as well as use sunblock/protective clothing. We may monitor for hypoglycemia and warfarin if indicated.
Aminoglycosides like gentamicin are known to be very potent with serious toxicities, which toxicities are of a concern and what are the contraindications?
Nephrotoxicity (renal failure)
Ototoxicity (auditory impairment and vestibular impairment [eighth cranial nerve])
Contraindications: hypersensitivity, renal disease, and pregnancy/breastfeeding
Anti-Virals are utilized to treat viral illnesses but are often quite difficult to eradicate because viruses can duplicate/mutate. What are some viral infections we can treat?
Smallpox, poliomyelitis, chickenpox, mumps, rabies and influenza, hepatitis, herpes simplex, herpes zoster