What type of hypersensitivity reactions are anaphylactoid reactions?
Trick question! They mimic hypersensitivity type 1 reactions - IgE mediated, anaphylaxis - however do not involve IgE.
4 signs of dehydrated infant
1 sunken fontanelle
2 sunken eyes
3 increased skin turgor
4 dry mucous membranes
Condition leading to highest mortality in Australia >65yrs?
CAD
What is the most common bacterial pathogen in CAP?
Strep. Pneumoniae
3 effects of adrenaline related to anaphylaxis
1 vasoconstriction
2 bronchodilation
3 positive inotrope
5 signs of severe malaria
1 altered consciousness (cerebral malaria)
2 extreme weakness (prostration)
3 seizures/convulsions
4 metabolic acidosis
5 respiratory distress
Patient with diabetes is 10x more likely to develop CVD. What does this represent?
relative risk
First line medication (with dosage) for severe CAP?
What about for patients with immediate hypersensitivity to penicillin?
IV ceftriaxone 1g daily AND IV azithromycin 500mg daily
Allergy: moxifloxacin 400mg IV daily
Which one of the following is most likely to result in a HR 40b/min?
1 SVT
2 VF
3 Atrial flutter
4 Heart block
5 Nodal reentry
Heart block
Spirometry: shows airflow obstruction but is not improved by bronchodilators, indicating what disease? Pathophysiology of disease
COPD: irreversible air flow obstruction
(FEV1/FVC < 0.7)
Chronic inflammation:
- damage to bronchial tree causes airway fibrosis and narrowing, increased mucus production and death of ciliated cells traps mucus = chronic bronchitis
- damage to lung parenchyma: permanently enlarged alveoli, decreased airway elasticity and decreased structural support for airway patency = emphysema
When repeated every 2-5 years, the FOBT used in the national bowel cancer screening program in Australia has sensitivity and specificity above 90% and a PPV of 3-10% for colorectal cancer.
Which factor best explains the relatively low PPV of the FOBT when used as a screening test for colorectal cancer in Australia?
prevalence of colorectal cancer in Australia
4 differential diagnoses for pleuritic chest pain
1 pneumonia
2 infective exacerbation COPD
3 pericarditis
4 PE
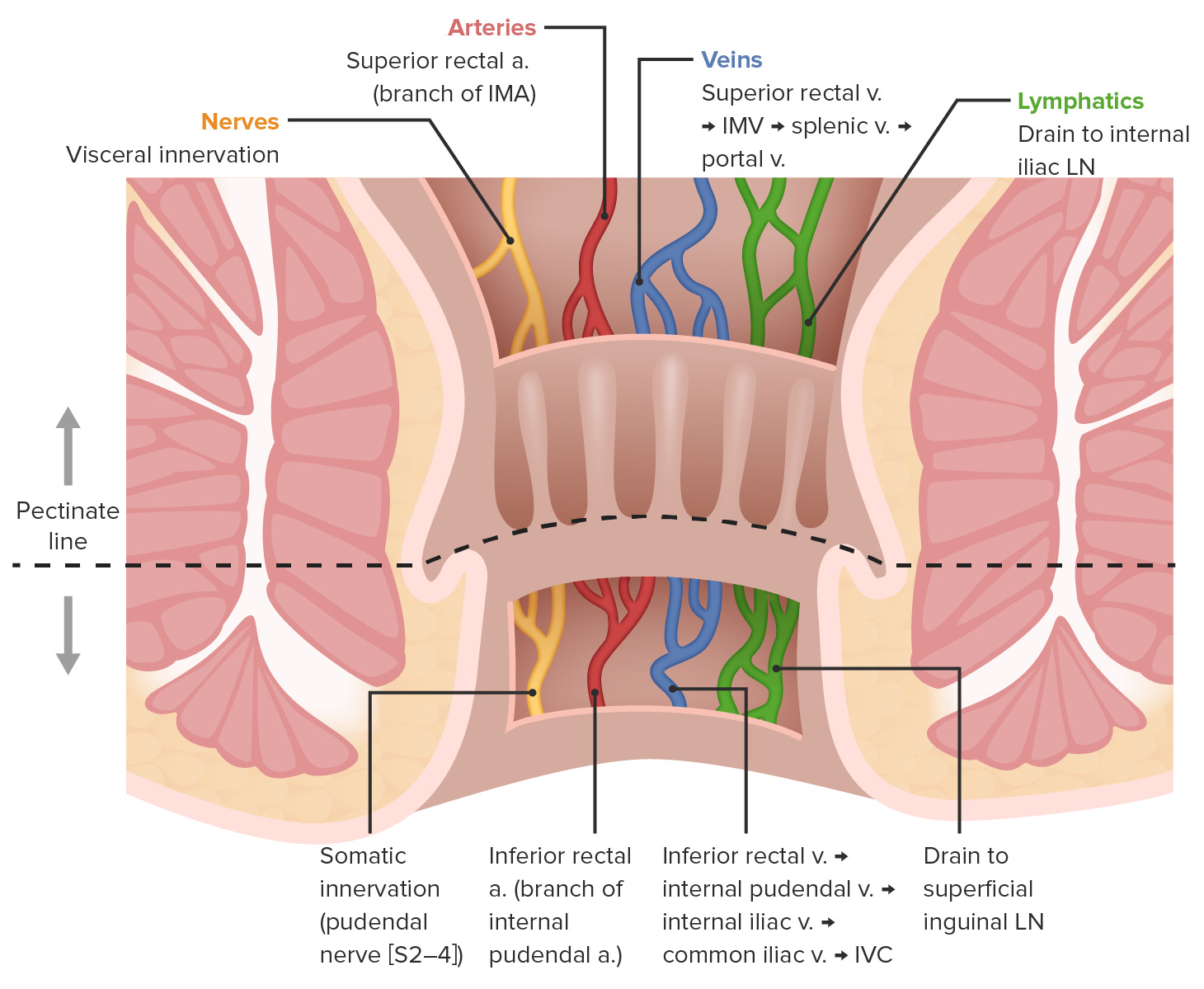
- lymph node drainage
- nerve supply
- blood supply and drainage
What is hepatisation? Two types of hepatization
Descriptive term for the conversion of lung tissue to solid tissue in diseases such as pneumonia
1 red hepatization: characterised by presence of RBC, neutrophils, fibrin in the alveoli giving the lungs a red, firm appearance
2 grey hepatization: RBC break down, leaving a fibrino-suppurative exudate, gives the lungs a grayish colour
With regard to consent for medical procedures, what comprises battery? (1)
failure to obtain valid consent constitutes battery - an intentional or reckless (0.5) application of physical force without the patient's consent (0.5)
Bacterial infection is associated with decreased platelets, however...
- septicemia activates coagulation cascade (rare complication is disseminated intravascular coagulation) and 'uses up' the platelets
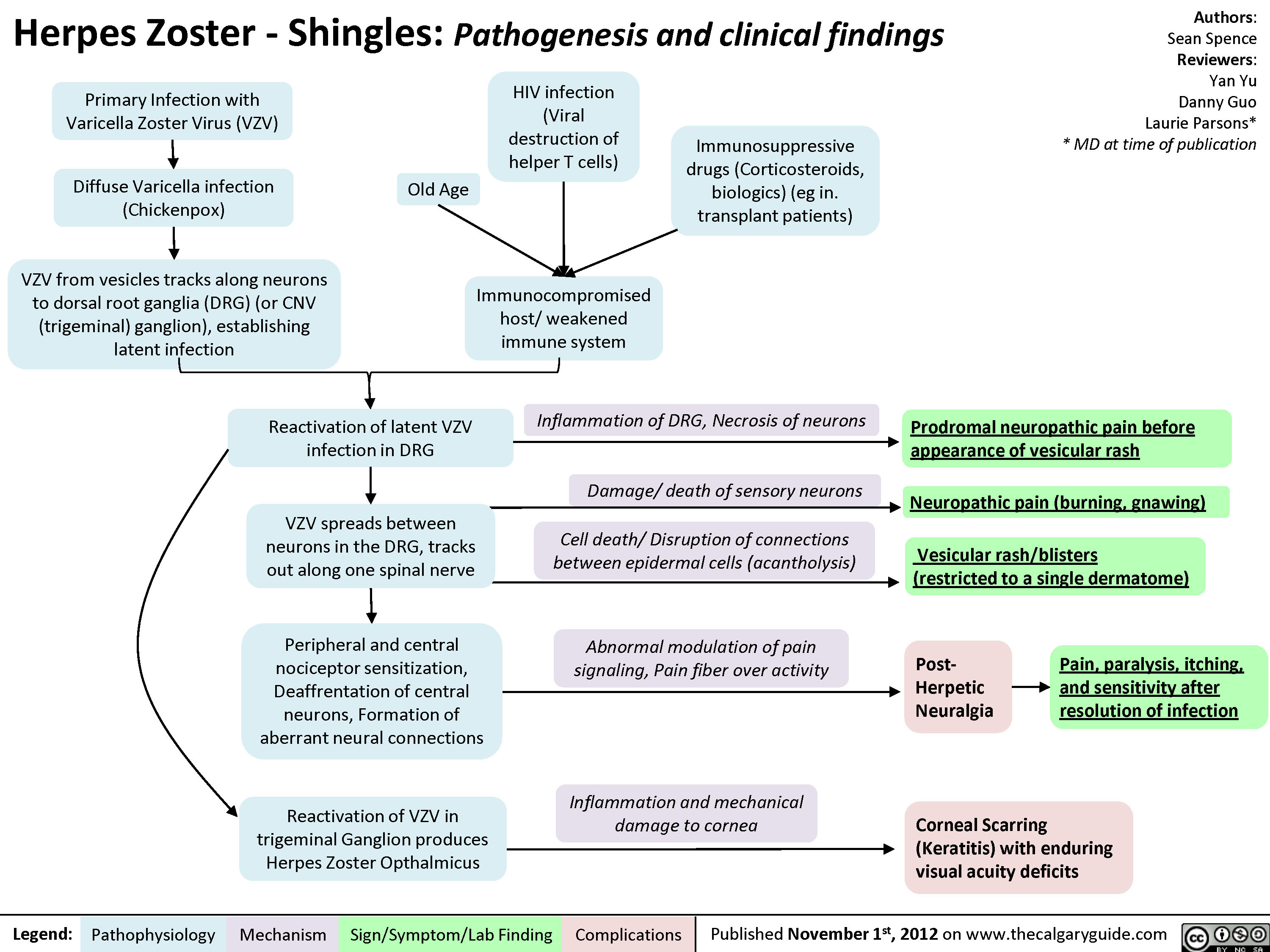
Pathophysiology of shingles
Hydrocephalus acquired before birth may be related to what?
Blockage of aqueduct of sylvius (aka cerebral aqueduct which connects 3rd and 4th ventricles in the brain)

A 7 year old child has been diagnosed with CAP. He is not allergic to any antibiotics, and the infecting organism is sensitive all antibiotics. What antibiotic should be given to this child?
Mild CAP (provide dose), CAP that requires hospitilisation and CAP critically ill/immunocompromised children
Mild CAP:
- High dose – amoxicillin at 25 mg/kg (max 1 g) per dose orally, three times a day for 5 days.
- If atypical pathogen suspected (e.g., Mycoplasma pneumoniae), school aged, or patient has a school aged sibling, commence either:
- doxycycline (if child aged > 8 years) 2 mg/kg (max 100 mg) per dose orally, 12‑hourly for 5 days, or
- clarithromycin 7.5 mg/kg (max 500 mg) per dose orally, 12‑hourly for 5 days, or
- azithromycin 10 mg/kg (max 500 mg) per dose orally, once a day for 5 days.
CAP that requires hospitilisation: ampicillin or penicillin
In critically ill or immunocompromised children in whom pneumococcal pneumonia is suspected or possible, vancomycin and a broad-spectrum cephalosporin should be used until or unless organism susceptibilities are available