Prior to 2004, what was the old classification of grades of VIN?
What is 1, 2, 3
What are 3 concerning colposcopic features of vulvar HSIL?
What are abnormal/atypical vessels, ulcerations, focal nodules
Which patients with vulvar HSIL should be treated?
What is all of them. Vulvar HSIL is a premalignant condition.
Case series in New Zealand 405 patients with VIN. 63 (16%) received no treatment and 10 progressed to invasive cancer
What is power density?
How does it change in relation to spot size?
What is: Power density (W/D2) is the concentration of laser energy at its focal point.
Power density increases as spot size decreases. Larger the spot size= less PD (coagulation effect). Smaller spot size = greater PD (cutting effect).
*PPT slides 50-55
This great mimicker is associated with vulvar squamous cell carcinoma in 5% of cases.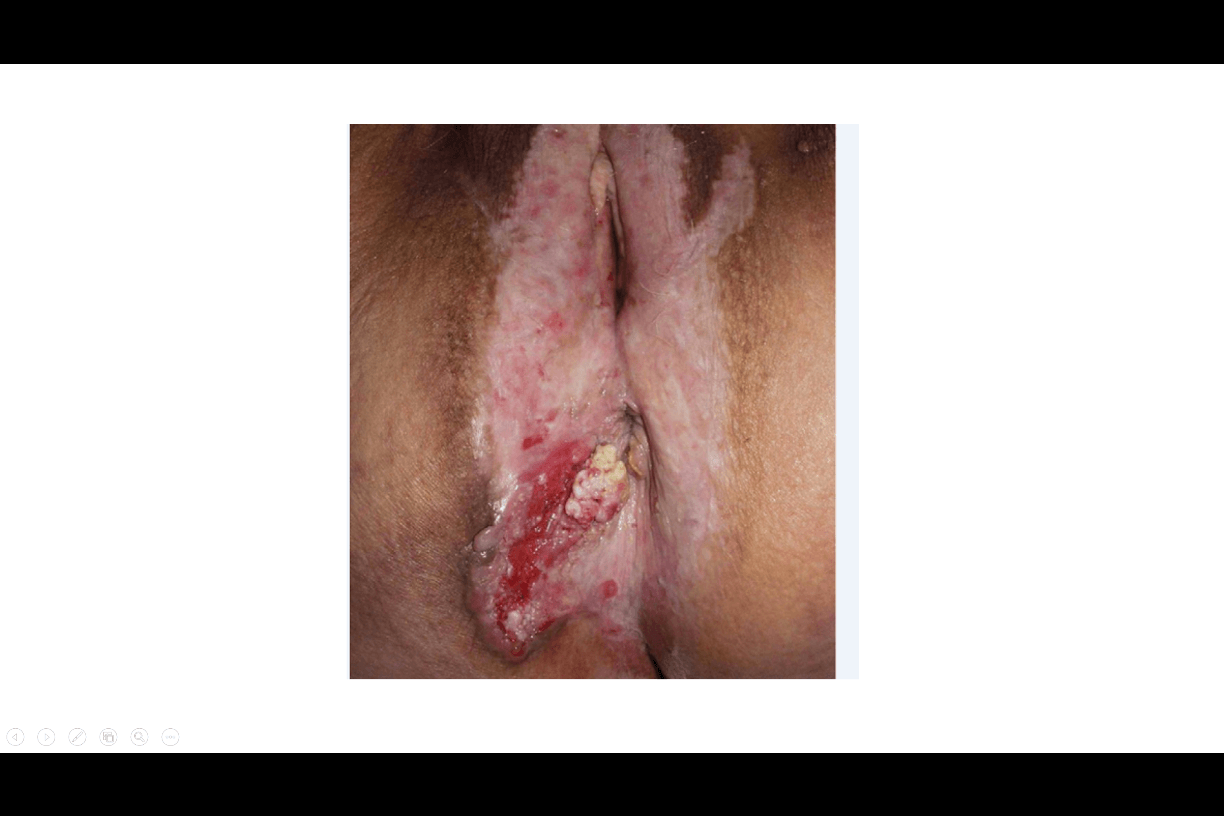
What is lichen sclerosis
2 part question:
1. Name the 3 layers of the vulvar skin.
2. How many surgical planes exist for the vulvar skin?
What is:
1. epidermis, dermis, subcutaneous
2. 4.
How much did the incidence of VIN increase from 1973 to 2000?
What is 4 fold
As of 2015, what is the new classification of VIN?
What is LSIL, HSIL, and Differentiated type VIN
When should biopsy be performed for suspected condyloma? (2)
What is :
1. postmenopausal women with genital warts
2. all ages when topical therapy fails
When is WLE treatment of choice for vulvar HSIL?
What is: if cancer is suspected d/t potential for occult invasion even if biopsy shows vulvar HSIL.
Occult invasion reported in 3% of women undergoing surgery (2/3 are superficial).
What laser settings will you ask your OR tech to set on the CO2 laser for non-hair bearing vulvar HSIL?
What is: Power Density 750-1250 W/cm2
Spot size 2-3mm
Power setting 15-30 W
Pulse or continuous mode
What is this great mimicker of vulvar HSIL?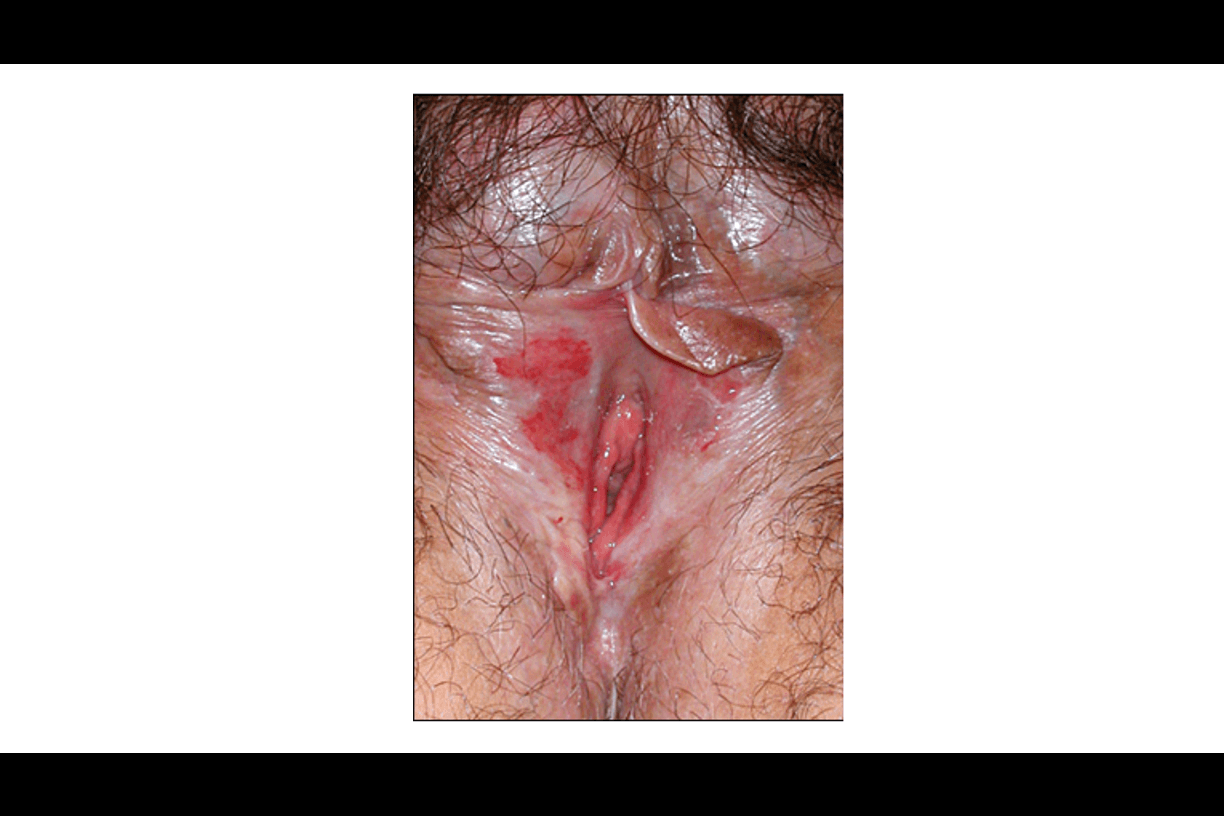
What is lichen planus
What vulvar skin layers constitute the first surgical plane?
What is epidermis down to basement membrane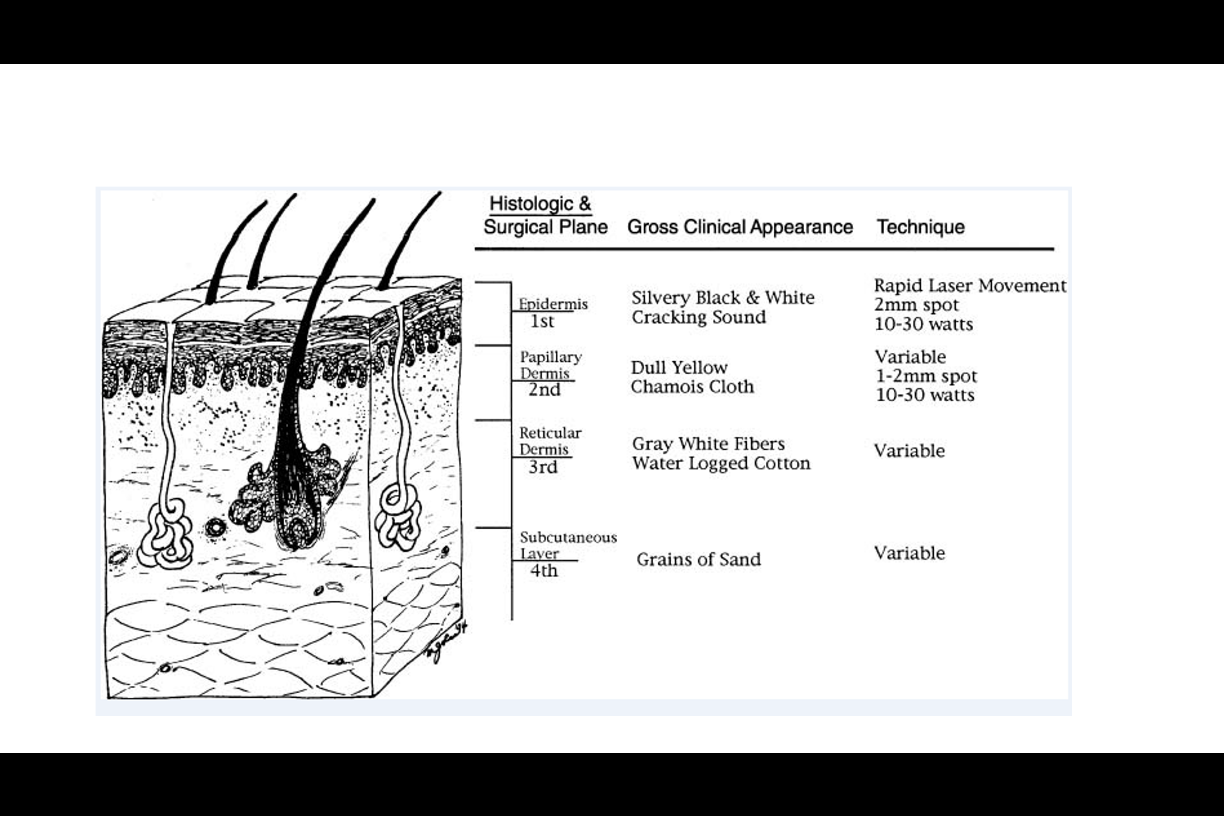
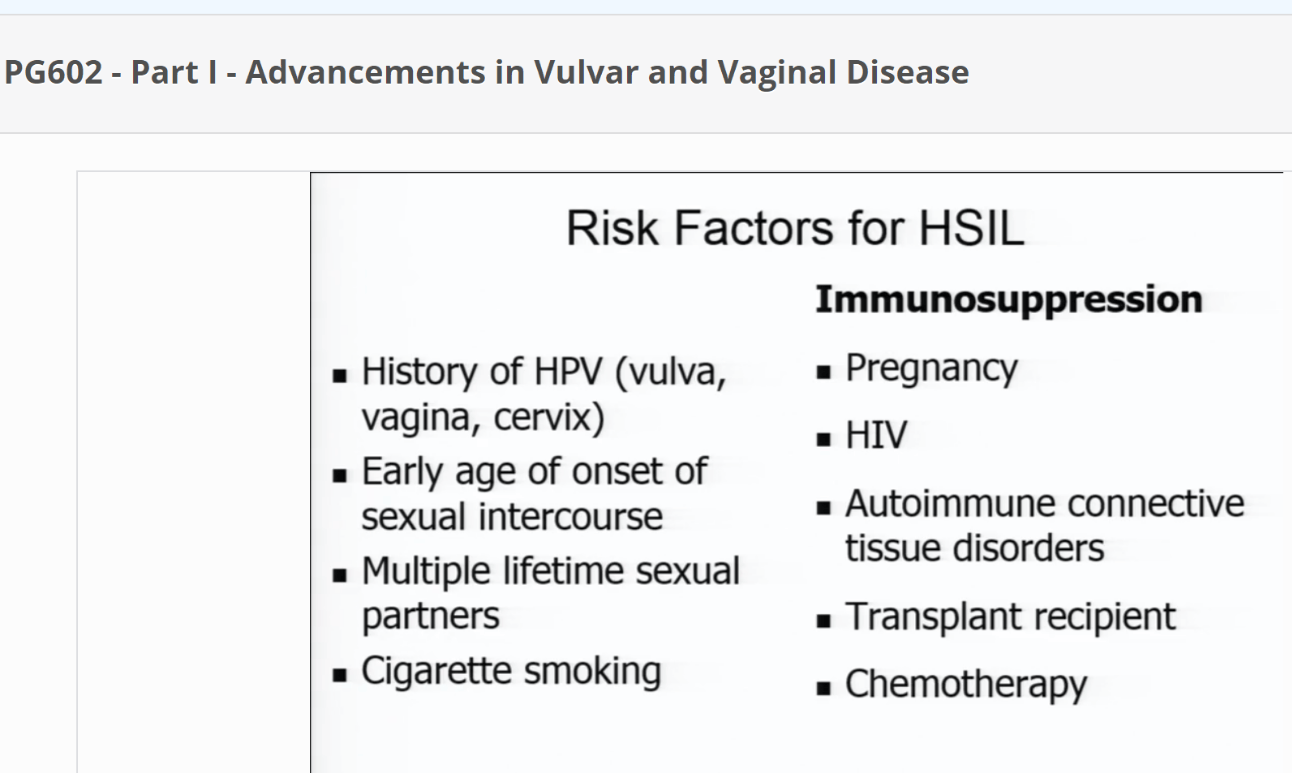
What are 3 risk factors for vulvar HSIL?
What lesions fit in the vulvar LSIL category?
What are flat lesions/condyloma, or those with HPV effect (essentially VIN 1)
What are 3 common signs/symptoms of vulvar SIL on clinical presentation?
What is 1. asymptomatic (50%) and noticed on pelvic exam
2. vulvar pruritis/discomfort (64%)
3. vulvar lesion (40%)
What are the suggested excision margins for WLE or laser ablation?
What is gross margins of 0.5-1cm around tissue with visible disease.
This may be altered to avoid injury to the clitoris, urethra, anus or other critical structures.
Women with clear margins in excised tissue have lower, although still significant, risk of recurrence compared to women with positive margins.
What is the primary tissue effect produced by CO2 laser?
What is thermal.
PPT slide 56-57
What is this great mimicker of vulvar HSIL?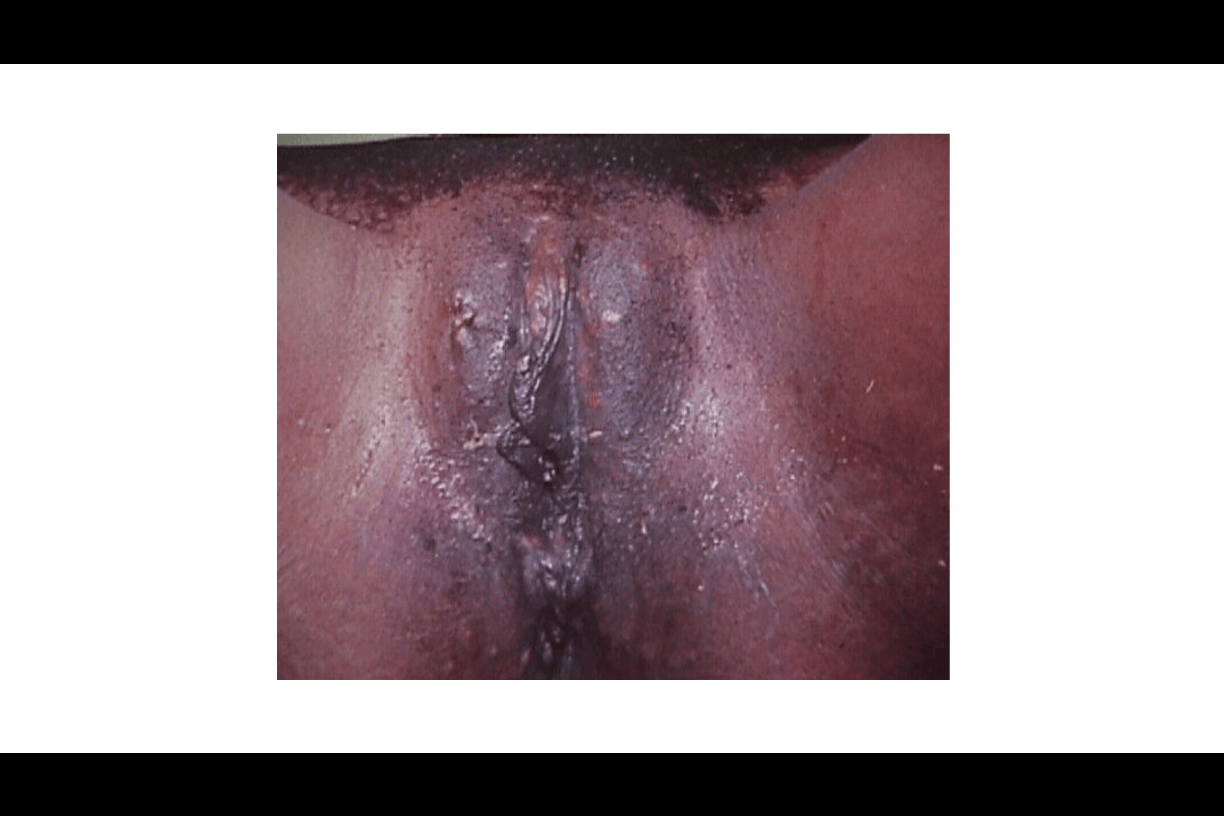
What is Condyloma lata of secondary syphilis
What layers constitute the second surgical plane of vulvar skin?
What is: it extends into papillary dermis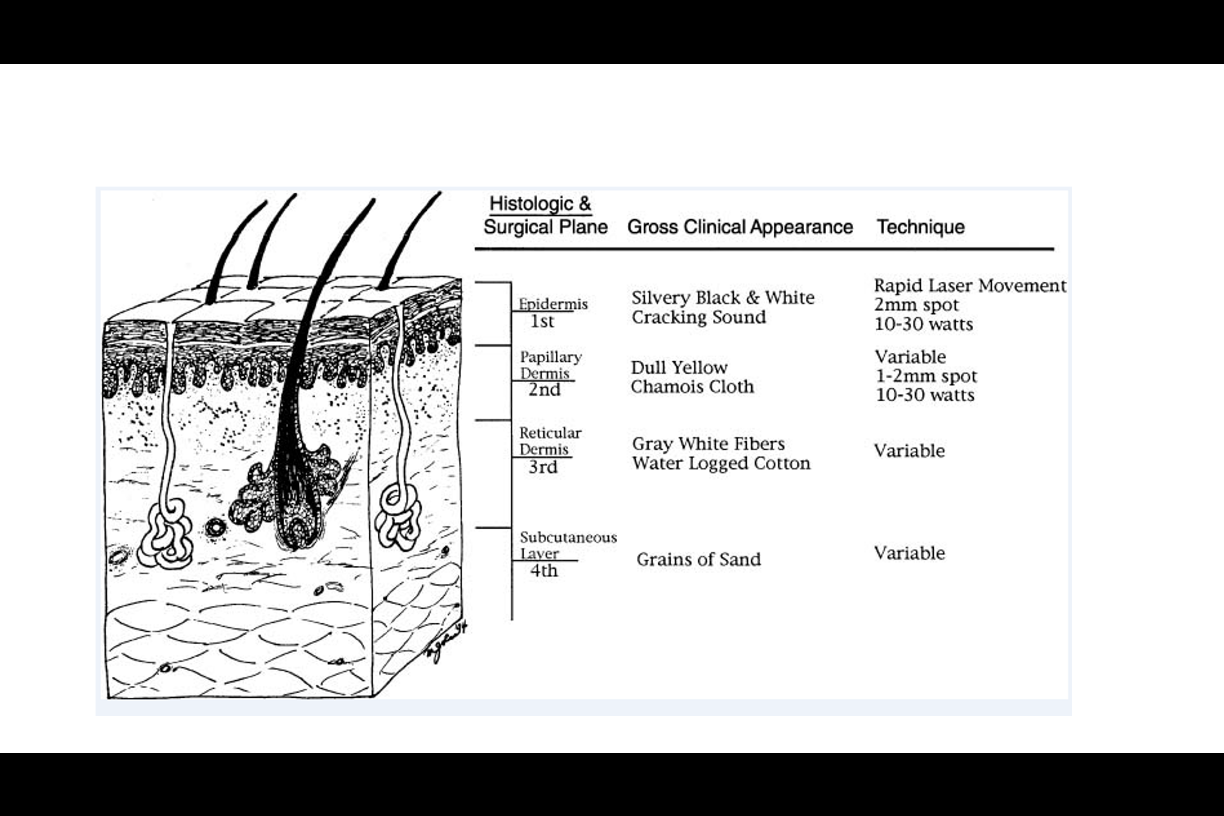
2 questions:
1. What 2 vaccines are available to protect against HPV?
2. How many strains of HPV do each protect against?
What is:
1. quadrivalent and nanovalent vaccines
2. 4 strains (6,11,16,18) and 9 strains (6,11,16,18,31,33,45,52,58)
*16,18 are the m/c strains of HPV that cause vulvar cancer in US.
*target age 11-12 years with catch up through age 26.
What lesions fit into the vulvar HSIL classification?
What are VIN usual type lesions: warty, basaloid, mixoid (VIN 2, 3)
What is the pathognomonic clinical appearance of vulvar SIL?
What is NONE.
They can be white/grey/brown/pink; raised or flat
*Go to PPT slide 20-25
What depth is acceptable for treatment of vulvar HSIL?
What is: if margins are clear, removal of the epidermis is acceptable. Removal of the underlying dermis (papillary layer) helps ensure absence of early invasive disease.
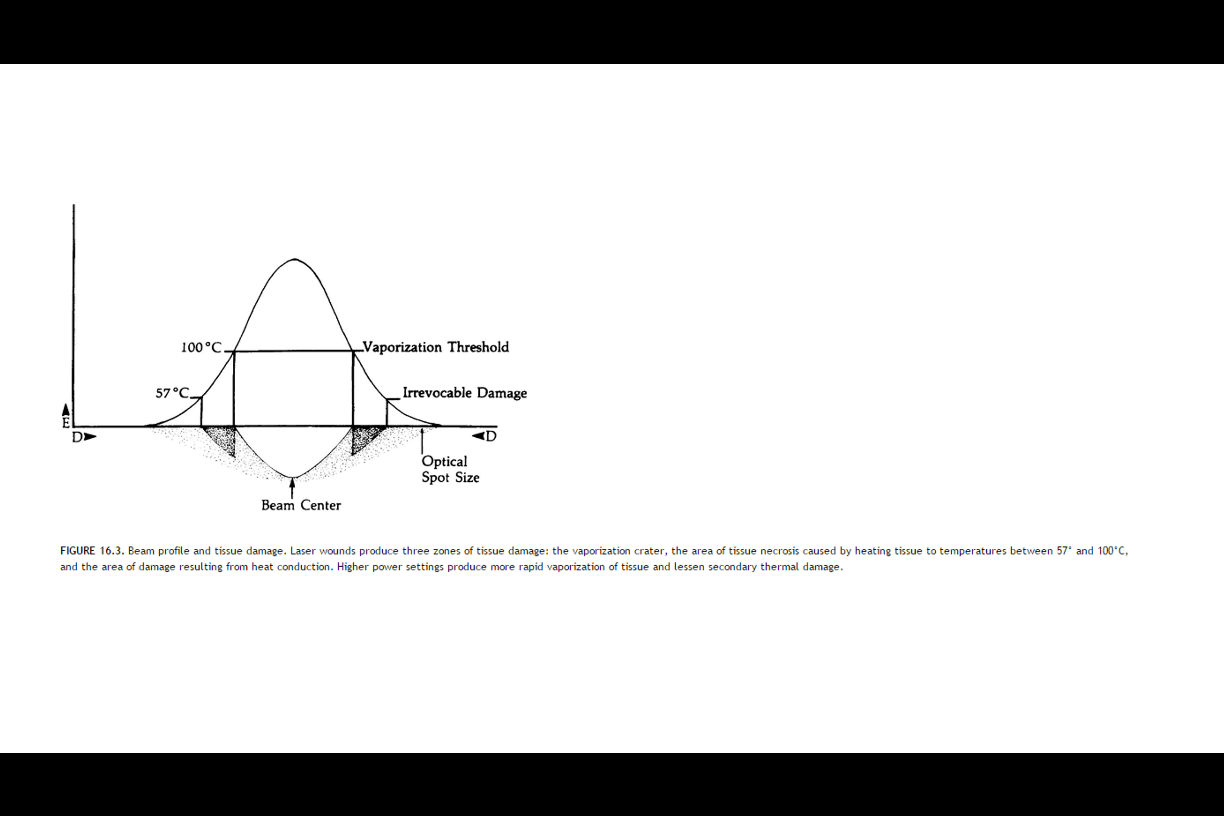
What are the 3 zones of laser tissue damage?
What are: 1. vaporization (>1000 C)*
2. tissue death short of vaporization (57-1000 C)
3. cell death d/t conduction of heat away from laser site (570 C)
What is this great mimicker of vulvar HSIL?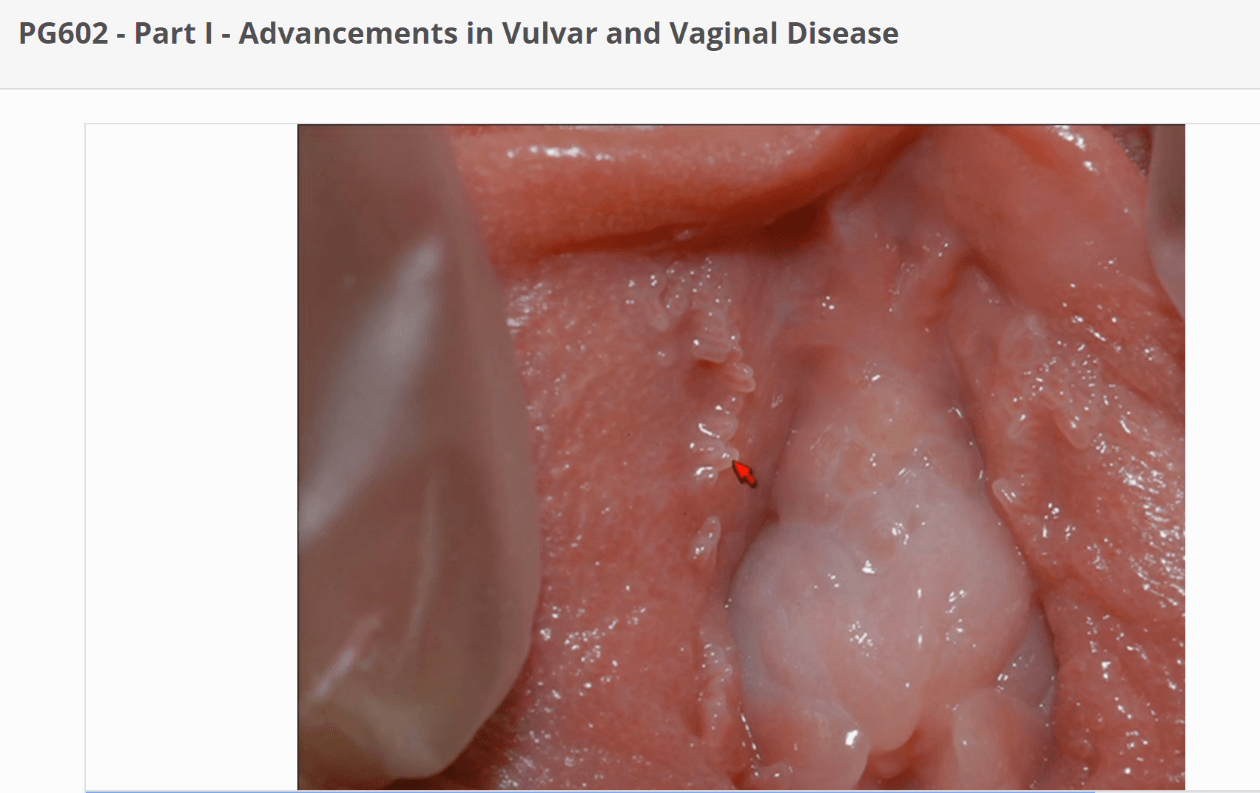
What is vestibular micropapillae.
Normal variant. Single based projections with finger-like projections.
What constitutes the layers of the 3rd surgical plane of the vulvar skin?
What is: extends into reticular dermis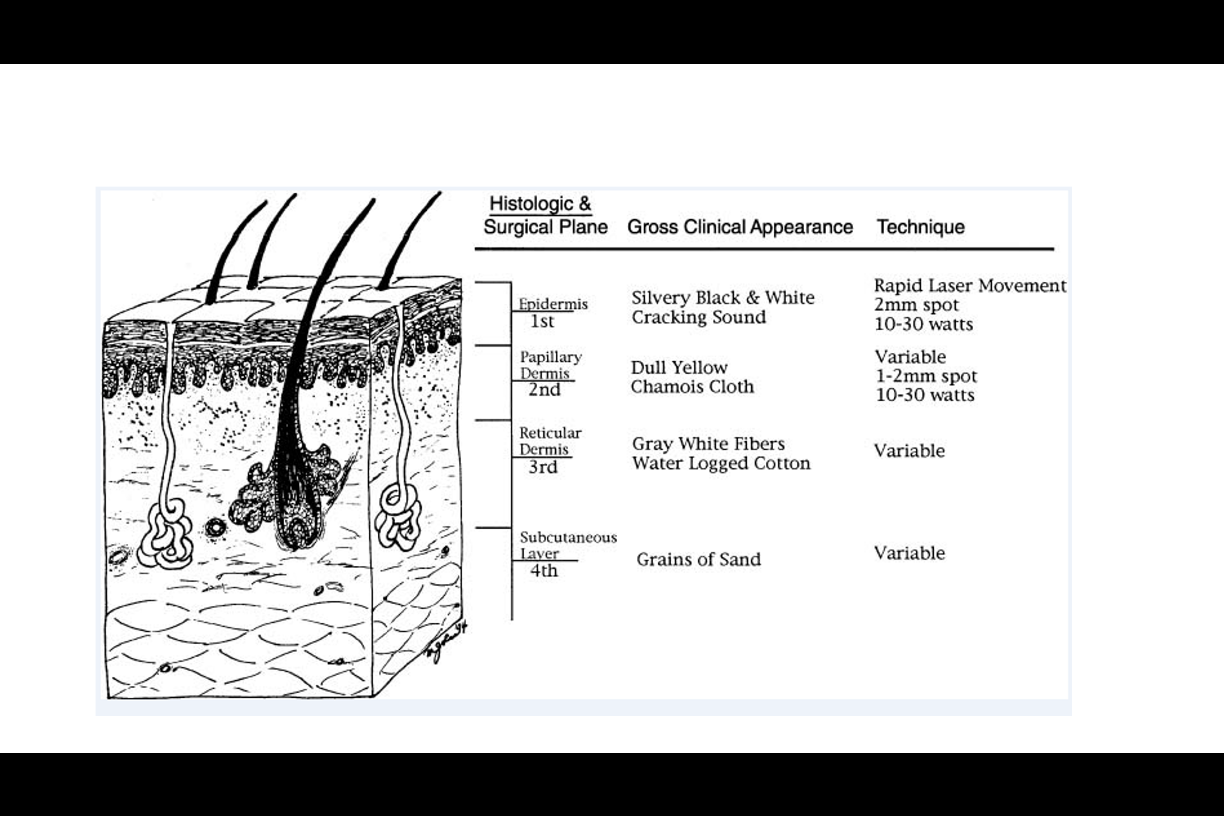
Per ACOG, how are women with complete response to therapy followed up?
What is: 6 months, 12 months after initial treatment and annually thereafter for physical exam.
*Some authorities recommend every 6 months indefinitely.
Which type of preinvasive vulvar disease is usually NOT associated with HPV?
What is Differentiated VIN.
List 3 of 5 indications for a vulvar biopsy.
What are: 1. visible lesion for which no definitive diagnosis can be made on clinical ground
2. possible malignancy
3. visible lesions with presumed clinical diagnosis that is not responding to usual therapy
4. lesions with atypical vascular patterns
5. stable lesions that rapidly change in color, border, or size.
BETTER SAFE THAN SORRY!!!
How does depth differ for hair bearing and non-hair bearing areas when treating vulvar HSIL surgically?
What is: Hair bearing areas need to extend to depth of at lease 3mm to include the hair folllicle which can harbor vulvar HSIL (extend to subcutaneous fat)
Non-hair bearing areas need to extend through the dermis (up to 2mm).
How do the CO2 laser settings differ for treatment of condyloma acuminata (vulvar LSIL) and vulvar HSIL?
What is: they don't. It is the depth of tissue destruction that differs.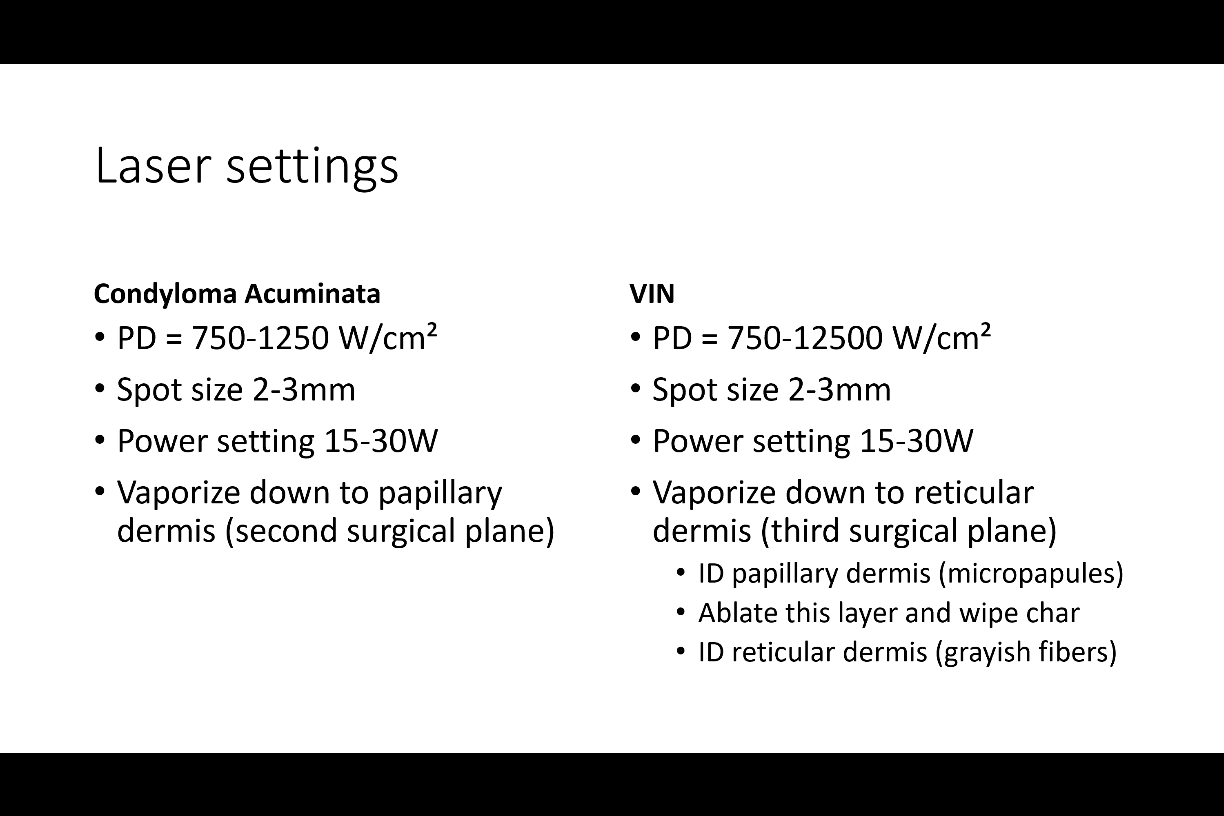
What is this great mimicker?
Paget's Disease of vulva
When lasering vulvar HSIL in non-hair bearing area, how do you assure you are lasering to the appropriate depth recommended?
What is: laser down to papillary dermis which is dull yellow color. Wipe char away and should see gray white fibers of reticular dermis (which is correct depth).
*Need intact skin appendages as they are the source of squamous epithelium for reepitheliazation.
2 questions:
1. How does Imiquimod work to treat vulvar HSIL? 2. How is it prescribed?
What is:
1. topical immune response modulator that stimulates local cytokine production and cell-mediated immunity
2. 5% formulation 3 times/week for 12-20 weeks. Colposcopy at 4-6 week intervals during treatment