A 78-year-old man is evaluated in the hospital for dyspnea and confusion. He was hospitalized 2 days ago after sustaining a midshaft fracture of the left femur. Twelve hours ago, he underwent operative repair under general anesthesia. One unit of packed red blood cells was transfused intraoperatively. Over the past 3 hours, he has become progressively more confused and hypoxemic. He is disoriented and cannot provide any further history. Medical history is otherwise notable for myelodysplastic syndrome and hypertension. Medications are lisinopril and subcutaneous heparin.
On physical examination, temperature is 37.8 °C (100.0 °F), blood pressure is 188/98 mm Hg, pulse rate is 110/min, and respiration rate is 22/min. Oxygen saturation is 93% with the patient breathing supplemental oxygen, 15 L/min by nonrebreather mask. He is agitated and confused. Lung examination reveals scattered crackles. The lower extremities are warm and well perfused. A petechial rash is noted on the right upper thorax. The surgical site is dry and intact.
Arterial blood gas studies (oxygen, 15 L/min by nonrebreather mask):
pH 7.39
Pco2 38 mm Hg (5.1 kPa)
Po2 62 mm Hg (8.2 kPa)
ECG shows sinus tachycardia but is otherwise normal. CT angiogram of the chest shows bilateral ground-glass opacifications and no pulmonary arterial filling defects.
Which of the following is the most likely diagnosis?
A.Anaphylactic transfusion reaction
B.Fat embolism syndrome
C.Hypertensive emergency
D.Malignant hyperthermia
A 28-year-old man is evaluated for a 4-month history of shortness of breath. It has progressed since onset, and he now notes dyspnea with walking up stairs. He has had no chest pain, cough, or orthopnea but has noticed occasional lower extremity edema at the end of the day. He does not smoke tobacco. His mother has pulmonary hypertension attributable to a variation in the gene for bone morphogenetic protein receptor type 2. He has no medical history and takes no medications.
On physical examination, vital signs are normal. No jugular venous distention or hepatojugular reflux is present. Cardiac examination reveals an accentuated pulmonic closure sound and a soft systolic murmur at the left lower sternal border. Lung sounds are normal. No lower extremity edema is noted.
Chest radiograph is normal.
Which of the following is the most appropriate diagnostic test to perform next?
Genetic testing
Right heart catheterization
Transthoracic echocardiography
Ventilation-perfusion scanning
An 84-year-old woman is evaluated in the emergency department for acute onset of shortness of breath and left-sided chest pain. She has severe COPD (Global Initiative for Chronic Obstructive Lung Disease [GOLD] stage 4/group E) for which she takes inhaled fluticasone furoate, umeclidinium, and vilanterol. She has a 50-pack-year history of smoking and continues to smoke.
On physical examination, temperature is 37.2 °C (99.0 °F), blood pressure is 117/65 mm Hg, pulse rate is 118/min, and respiration rate is 35/min. Oxygen saturation is 90% with the patient breathing oxygen, 6 L/min by nasal cannula. Auscultation of the lungs reveals diminished breath sounds on the right side and no breath sounds on the left side, with hyperresonance on percussion on the left side.
Chest radiograph shows a moderate left-sided pneumothorax; hyperinflation and diffuse scarring also are evident.
A small-bore thoracostomy tube is placed in the left chest and set initially on suction mode. No air leak is detected. Follow-up chest radiograph demonstrates full expansion of the lung.
Which of the following is the most appropriate next step in treatment?
Autologous blood patch
Chemical pleurodesis
Endobronchial valve placement
Thoracostomy tube removal
A 72-year-old man is evaluated for a 6-month history of progressive shortness of breath. He previously could climb two flights of stairs without dyspnea, but he now has to catch his breath after half a flight. He reports no chest pain but has an intermittent, nonproductive cough. He has a 30-pack-year history of tobacco use and quit smoking 6 years ago. Medical history is significant for hypertension, for which he takes amlodipine.
On physical examination, vital signs are normal. Oxygen saturation is 93% with the patient breathing ambient air. The remainder of the physical examination is normal.
Pulmonary function tests:
FEV1
58% of predicted
L
FVC
60% of predicted
L
FEV1/FVC ratio
0.97
Chest radiograph reveals right basilar scarring.
Which of the following is the most appropriate next step in management?
Measure lung volumes and Dlco
Perform 6-minute walk test
Perform transthoracic echocardiography
Start tiotropium
A 46-year-old woman is evaluated after the incidental discovery of a pulmonary nodule on CT scan. Two weeks ago, she was evaluated in the emergency department for abdominal pain. A CT scan of the abdomen obtained at that time revealed diverticulitis and a 5-mm solid pulmonary nodule with regular margins in the right lower lobe of the lung. She has no shortness of breath, chest pain, hemoptysis, weight loss, or other symptoms. She has not previously undergone chest imaging. The patient has hypertension treated with lisinopril. Her mother died of breast cancer; she has no other family history of cancer. She does not smoke tobacco.
Physical examination findings, including vital signs, are normal.
Which of the following is the most appropriate next step in image-based diagnostic testing?
A 44-year-old woman is evaluated for a 3-month history of exertional dyspnea. She initially presented 3 months ago with chest pain and dyspnea and was diagnosed with pulmonary embolism. Her dyspnea initially improved, but she has not regained her baseline. She now can walk up one flight of stairs before needing to stop. She has no other medical history, and her only medication is rivaroxaban.
On physical examination, blood pressure is 104/74 mm Hg and pulse rate is 92/min; other vital signs are normal. No jugular venous distention is present. Cardiac examination reveals an accentuated pulmonic valve closure sound. Lung examination is normal. No peripheral edema is present.
Chest radiograph is normal.
Which of the following is the most appropriate next step in management?
CT pulmonary angiography
Inferior vena cava filter placement
Right heart catheterization
Transthoracic echocardiography
A 73-year-old man is evaluated for a pulmonary nodule. Chest CT performed 1 week ago revealed an 8-mm ground-glass opacity without a solid component in the right upper lobe of the lung. The opacity is unchanged in size and appearance when compared to findings on chest CT performed 1 year ago. He has COPD (Global Initiative for Chronic Obstructive Lung Disease [GOLD] stage 1/group A) and a 40-pack-year history of smoking; he stopped smoking 13 years ago. The patient's only medication is an as-needed albuterol inhaler.
On physical examination, vital signs and other findings are normal.
Which of the following is the most appropriate next step in testing?
PET/CT
Repeat chest CT in 1 year
Repeat chest CT in 2 years
No further testing
A 40-year-old woman presents to refill her albuterol inhaler. Over the last 4 to 5 months, she has noticed that she needs her albuterol inhaler 3 times weekly for symptoms not associated with exercise. She has no symptoms upon awakening. There are no apparent environmental triggers, reflux symptoms, sinus symptoms, or recent respiratory infections.
Vital signs are normal. The patient has expiratory wheezing.
Laboratory studies, including a complete blood count and IgE level, are normal.
Pulmonary function tests:
FEV1
82% of predicted
FEV1 improves significantly following inhaled albuterol. Her inhaler technique is excellent.
Which of the following is the most appropriate treatment?
Budesonide-formoterol twice daily and as needed
Ipratropium four times daily
Montelukast once daily
Salmeterol twice daily
A 24-year-old patient is evaluated in the emergency department for dyspnea and wheezing. They have a history of moderate persistent asthma and woke up in the middle of the night with shortness of breath that has not resolved with rescue inhaler therapy. The patient misplaced their asthma action plan and has a new nonproductive cough but no chest pain, fevers, or other new symptoms. Other medical history includes allergic rhinitis and nasal polyps. Medications are medium-dose budesonide-formoterol and montelukast.
On physical examination, temperature is 36.7 °C (98.1 °F), pulse rate is 105/min, and respiration rate is 22/min. Oxygen saturation is 94% with the patient breathing ambient air. The patient is speaking in four- to five-word sentences with no accessory muscle use. Lung auscultation reveals diffuse expiratory wheezes with fair air movement.
Chest radiograph is normal.
Which of the following is the most appropriate therapy?
A.Azithromycin
B.High-dose budesonide-formoterol
C.Prednisone
D.Tiotropium
A 66-year-old man is evaluated for worsening dyspnea and hypoxemia 24 hours after undergoing open cholecystectomy. He has a productive cough and abdominal pain at the incision site, which is aggravated by the cough. He has a 24-pack-year history of smoking. Medications are subcutaneous heparin and morphine sulfate as needed for pain.
On physical examination, respiration rate is 24/min; other vital signs are normal. Oxygen saturation is 90% with the patient breathing supplemental oxygen, 4 L/min by nasal cannula. BMI is 37. Mildly increased work of breathing and shallow breath sounds are noted. Pulmonary examination reveals decreased breath sounds in both lung bases with bibasilar crackles. Abdominal examination reveals moderate tenderness in the right upper quadrant over the incision without rebound tenderness, and the surgical wound is without erythema or discharge. The remainder of the examination is normal.
Chest radiograph shows small lung volumes with bibasilar atelectasis.
A patient-controlled analgesia pump is started.
Which of the following is the most appropriate management?
Bronchoscopy
Naloxone
Piperacillin-tazobactam
Respiratory physiotherapy
A 72-year-old patient is evaluated for worsening dyspnea on exertion. They have a longtime history of cigarette smoking.
Chest radiograph is shown.

Which of the following is the most likely abnormality seen on this frontal chest radiograph?
Hilar adenopathy
Interstitial lung disease
Mediastinal mass
Prominence of the pulmonary arteries
A 73-year-old man is hospitalized for dyspnea, orthopnea, and daytime sleepiness. He has amyotrophic lateral sclerosis.
Respiration rate is 28/min. Oxygen saturation is 87% with the patient breathing ambient air. His speech is clear. He is able to manage his secretions and has an intact gag reflex. He has abdominal paradoxical breathing and shallow tachypnea. He has scattered fasciculations. He is awake but dozes off easily.
Arterial blood gases (ambient air):
pH
7.3
L
Pco2
76 mm Hg (10.1 kPa)
H
Po2
50 mm Hg (6.7 kPa)
L
The alveolar-arterial oxygen gradient is normal.
Chest radiograph reveals shallow inspiration.
Which of the following is the most appropriate treatment?
Invasive mechanical ventilation
Noninvasive ventilation with bilevel positive airway pressure
Noninvasive ventilation with continuous positive airway pressure
Oxygen administration through nasal cannula
A 57-year-old man is evaluated for loud snoring. His husband notes a long history of snoring that is worse in the supine position. The patient occasionally gasps when supine, but his husband has not noted apnea. The patient describes a regular sleep schedule between 10:30 pm and 6:30 am; he awakens feeling rested and does not have daytime sleepiness or headaches. He does not drink alcohol. Medical history is significant for dyslipidemia and recently diagnosed type 2 diabetes mellitus. Medications are rosuvastatin and metformin.
On physical examination, vital signs are normal. Oxygen saturation is 97% with the patient breathing ambient air. BMI is 36. He has a low-lying soft palate and normal tonsils. Pulmonary, cardiac, and neurologic examinations are normal.
The patient is referred to a bariatric clinic.
Which of the following is the most appropriate diagnostic test to perform next?
Home sleep apnea testing
In-laboratory polysomnography
Overnight pulse oximetry
No further diagnostic testing
An 84-year-old woman is hospitalized for cough and confusion. Two days ago, she had onset of confusion and global weakness. Over the next day, her oral intake decreased and she developed a productive cough and low-grade fever. Medical history is significant for hypertension and heart failure with preserved ejection fraction. Her medications are lisinopril, empagliflozin, spironolactone, and furosemide.
On physical examination, temperature is 37.8 °C (100.0 °F), blood pressure is 100/60 mm Hg, pulse rate is 118/min, and respiration rate is 28/min. Oxygen saturation is 89% with the patient breathing high-flow humidified oxygen by nasal cannula. Neck veins are flat. Pulmonary examination reveals few crackles in the left lung base. The remainder of the examination is normal.
Laboratory studies:
Hemoglobin
12.6 g/dL (126 g/L)
Leukocyte count
19,400/µL (19.4 × 109/L), with 84% neutrophils, 12% lymphocytes, and 4% monocytes
H
Blood urea nitrogen
40 mg/dL (14.3 mmol/L)
H
Creatinine
1.9 mg/dL (168 µmol/L)
H
B-type natriuretic peptide level
226 pg/mL (226 ng/L)
H
COVID-19, influenza A/B tests
Negative
Chest radiograph is normal.
Which of the following is the best next step in management?
Ceftriaxone and azithromycin
Intravenous furosemide
Serum procalcitonin measurement
Ventilation-perfusion scanning
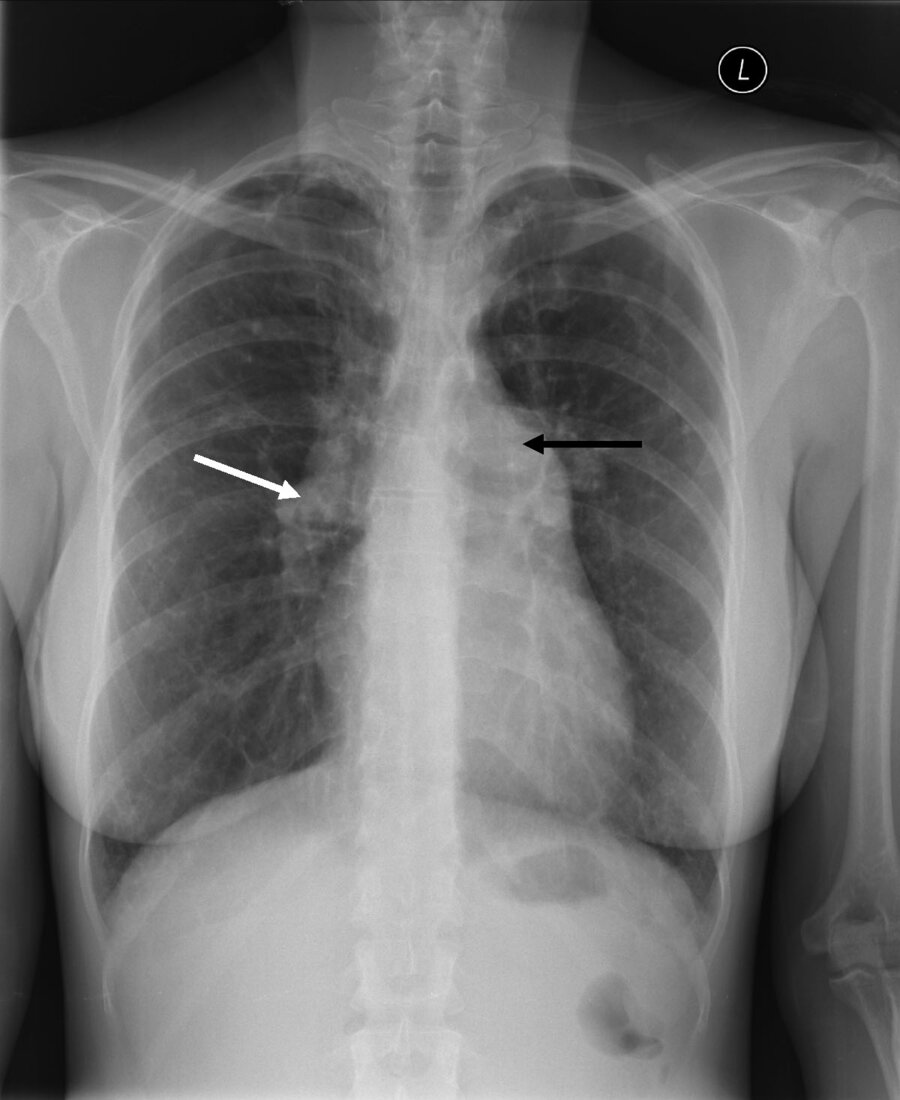
A 48-year-old man is hospitalized following 4 weeks of cough and fever unresponsive to antibiotic therapy.
Chest CT scan is shown.
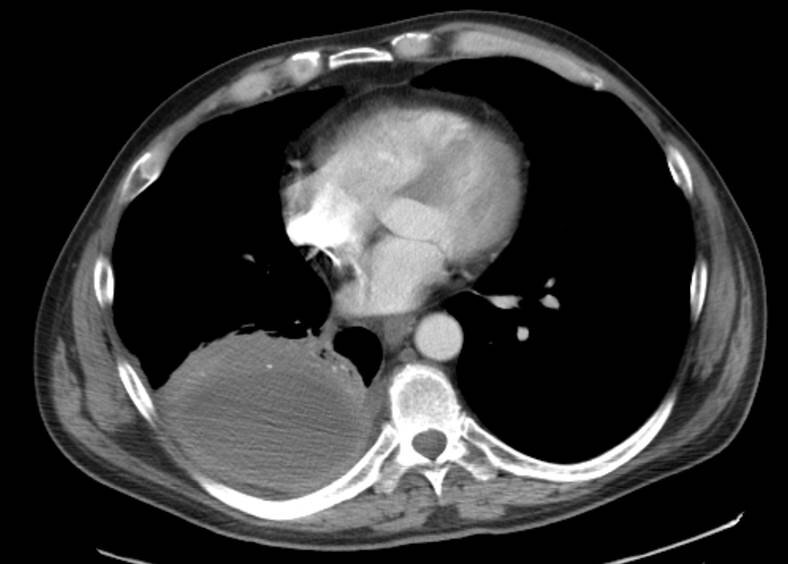
Which of the following is the most likely diagnosis?
Empyema
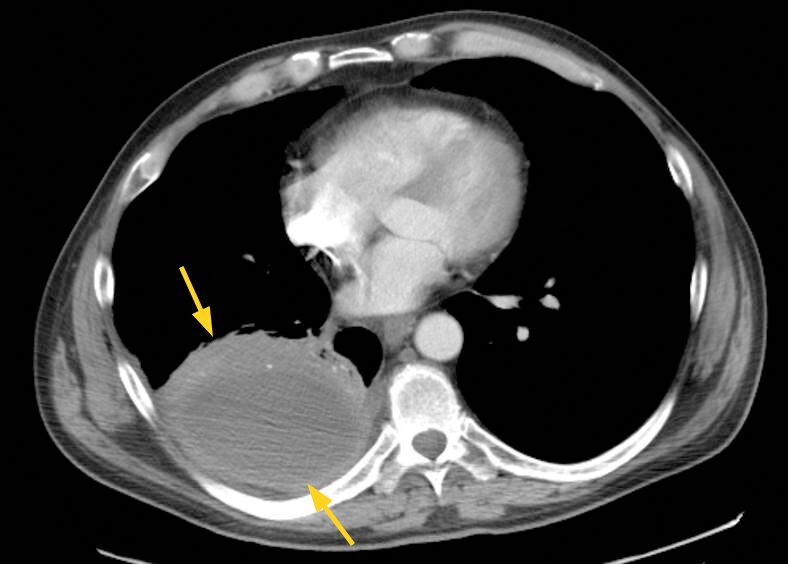
Lung abscess
Lung cancer
Mesothelioma
A 69-year-old man is evaluated for chronic dyspnea without cough. Pulmonary function demonstrates an obstructive defect that persists following bronchodilator administration.
Chest radiographs are shown.
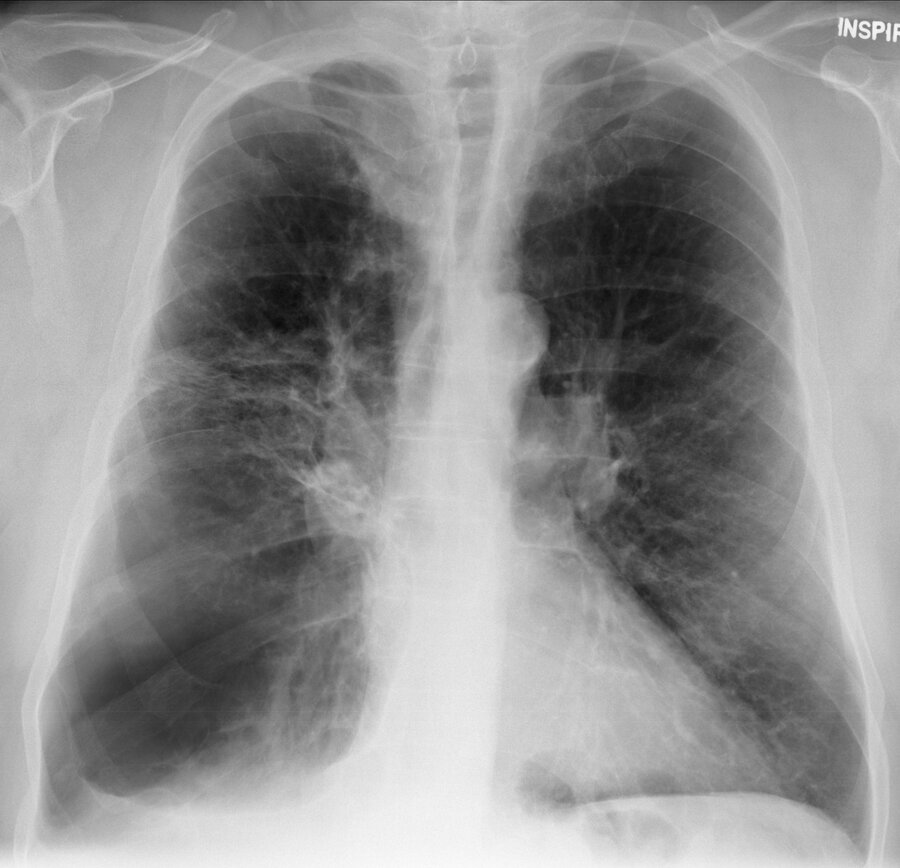

Which of the following conditions is the most likely radiographic diagnosis?
Bronchiectasis
Bullous lung disease
Left lower lobe pneumonia
.Hodgkin lymphoma