During Rest, Inhaling, and Expiration, which Atmospheric pressure is higher, IntraPlural or Intrapulmanory
The Intrapulmonary is always higher.
What is Positive transpulmonary pressure? (intrapulmonary minus intrapleural pressure)
This keeps the lungs partially inflated at all times, This prevents the lungs from collapsing.
the exchange of O2 for CO2 occurs when?
Once Air makes it way into the alveolus
What are the Functions of Mucous in alveolar space?
-prevents desiccation of lung tissue(H2O in mucous provide moisture to alveolar tissue and prevents desiccation)
- surface tension of water in alveolar spaces causes the alveolus to resist expansion
- resisting of expansion produces recoil in alevolus during exhaustion and aids w/ flow of air out of lungs
this substance prevents alveolar collapse due to surface tension and unequal alveolar volume. It's also made up of Type II alveolar cells; 90% phospholipid w 10% proteins. it also interferes w the H-bond between H2O causing reduced T and minimize effects of T in alveolar space.
what is pulmonary surfactant?
During rest what is the Intrapulmonary, and Intra pleural pressures?
760mmHg, 756mmHg
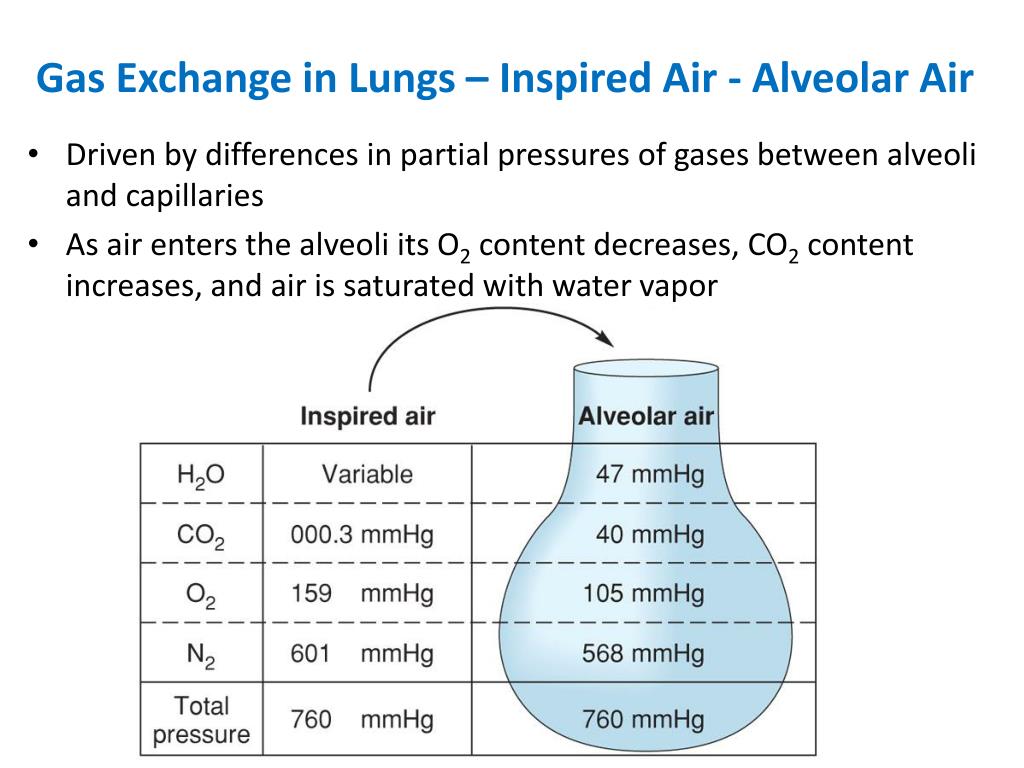
Memorize this Chart!!!!!!!!!!!
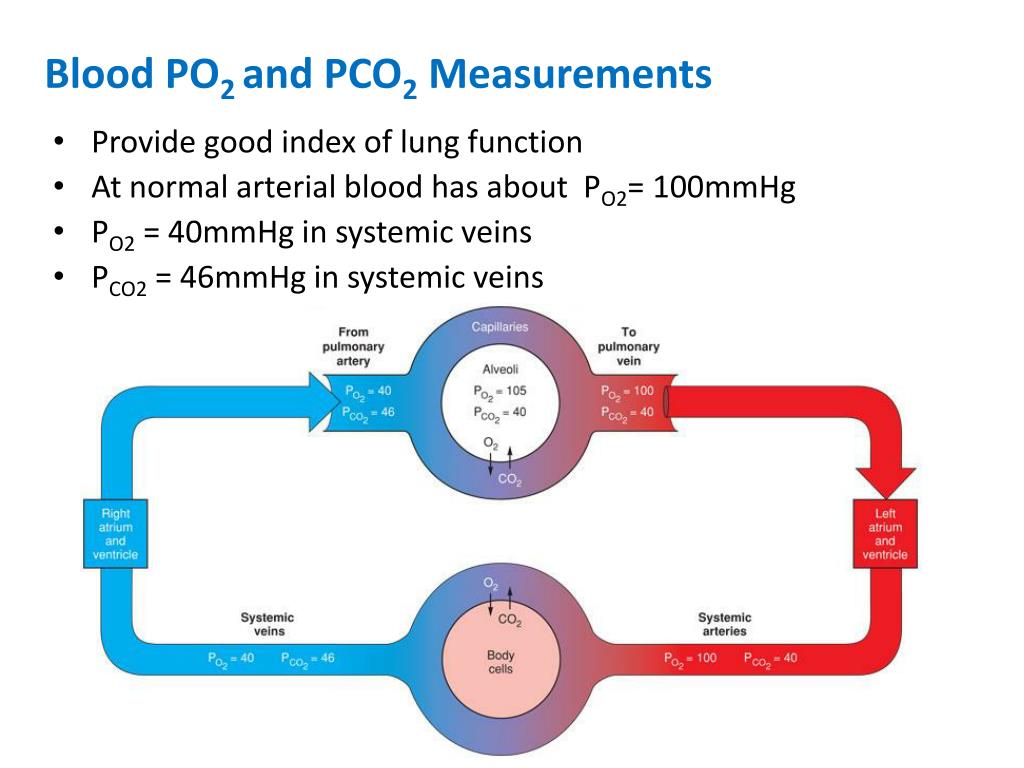
Memorize this chart!!!!!!!
_________ is directly proportional to alveolar pressure.
what is surface tension?
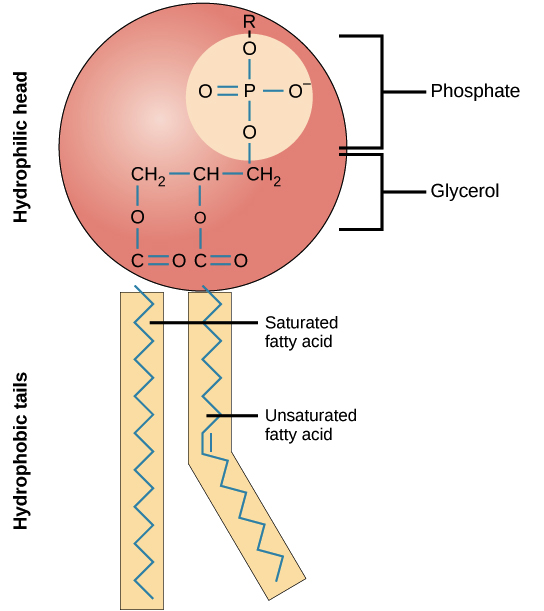
Recall that phospholipids are amphipathic Hydrophilic head interacts with H2O molecule and inhibits H-bond formation. This lowers surface tension. surface tension is disproportionately reduced in smaller alveoli
what is the structure of the Respiratory system
Nasal Passage->Nasal Cavity->Pharynx->Trachea->Bronchi->Bronchioles-> Terminal Bronchioles->Respiratory Bronchioles->Alveolus
Inspired Air at Alveolus/Alveoli. What is it?
Warmed air(from passing through the body). "cleaned air" (Fine particles are filtered with nose hairs, beating of cilia by ciliated cells lining the trachea). Humidified (the mucous lining the respiratory tracts add water vapor to the traveling air)
Type I & Type II alveolus cells line the___
what is the alveolus lined w/?
alveoli are not all equal in size. Pressure in each alveolus is calculated as _ = (_ x _)/r; T= surface tension r= radius
what is alveolus pressure equation P=(2 x T)/r.

rhythmicity center in medulla oblongata generated auto breathing (12-20 breaths/min); contains inspiratory neurons and expiratory neurons. Ventilation volume rate is 6-10 Lt/min. apneustic area of pons stimulates inspirtory neurons and promotes inspiration. Pneumotaxic area antagonizes apneustic area and inhibits inspiration(decrease)
What do contraction of the diaphragm and intercostals do during Inspiration?
Increase in the thoracic cavity volume by the diaphragm shifting downward and ribcage moving out and up. This causes the decrease for the Intrapulmonary Pressure
Why do we need some CO2 in our blood?
This fluid forms a thin wall lining layer in the alveolus. Most of the H2O in the mucous results from Cl- transport out of the alveolar cells
what is Mucous in the Alveolus?
Blood CO2 increases and this lead to pH decrease. This decrease is detected by chemoreceptors neurons. The stimulated neurons lead to stimulation of inspiration neurons, thus breath rate increases
what is The Effects of Blood PCO2/ pH on ventilation
What do Relaxation of the diaphragm and intercostals do during Expiration?
It decreases the thoracic cavity volume by diaphragm moving upwards and ribcage moving down and in. This causes the increase of intrapulmonary pressure.
Reverse Chloride Shift. What occurs with the CO2?
CO2; dissolved in plasma DIFFUSES into alveolus.; attached to Hd(Haldane Effect) detaches, and DIFFUSES into alveolus; diffuses out RBCs, diffuses in the alveolus and is exhaled.at lungs band 3 works in reverse, this promotes breakdown of carbonic acid into H2O and CO2.
These channels are found on the membrane of the alveolar cells (I & II), along with liver, pancreas, digestive, and reproductive tract cells. This is also a CI- channel that allows CI- to diffuse out of alveolar cells and into mucous. This also promotes movement of H2O out of cells and into mucous by osmosis.
What is the Cystic Fibrosis Transmembrane Conductance Regulator?
one collapse water in mucous keeps _____ wall stuck together making it impossible to open back up. leads to reduced lung volume for respiration, where not enough O2 is obtained causing hypoxia
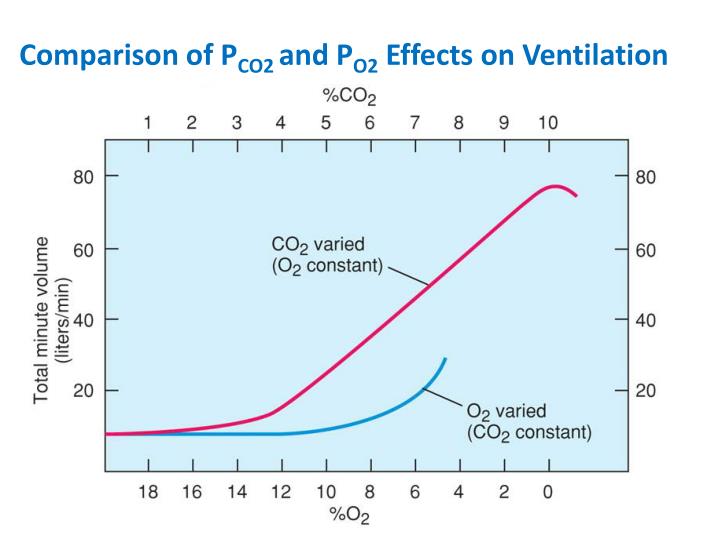
this graph compares the effect of PCO2 and PO2 on ventilation rate. changes in PCo2 have greater effect on ventilation rate than changes to PO2