What small vessel vasculitis presents with asthma, nasal polyp, sinusitis, neuropathy with granuloma on biopsy, +pANCA/MPO?
A. Microscopic polyA
B. Eosinophilic granulomatosis with polyA
C. granulomatosis with polyA
D. polyA nodosa
eosinophilic granulomatosis with polyA (churg-strauss)
72 yo M presents with 1 year of difficulty rising from chair and notes he has been dropping objects. PMhx includes HTN on losartan, HLD on statin.
labs: CK 900
Q: what is his dx?
A. Dermatomyositis
B. Inclusion Body Myositis
C. Polymyositis
D. Necrotizing Myositits
Inclusion Body Myositis (slow onset, Prox & Distal muscle groups)
Muscle biopsy: inclusion bodies (same as polyM/DermoM)
+anti-cN1A (rarely obtained)
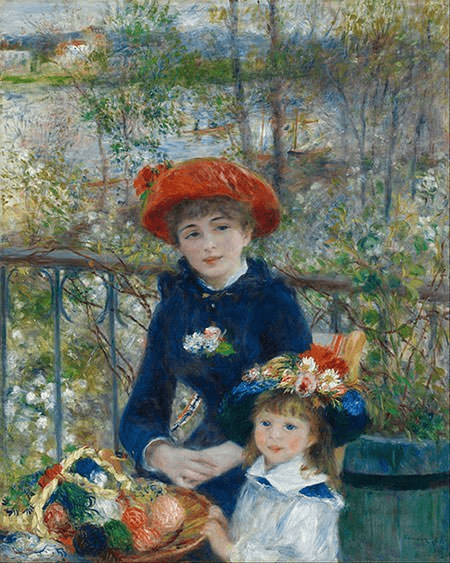
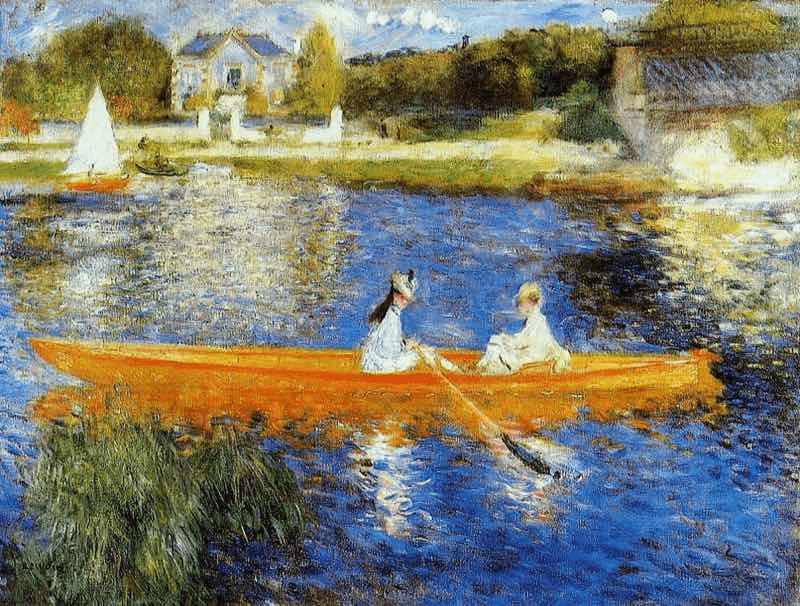
What low sensitivity lab test is positive in Hep B/C, TB/fungal infection, mix CT disease, Waldenstrom's gammoglobathy as well as this arthritis? This famous impressionist suffered from this arthritis.
Rheumatoid factor
43 Yo M presents with this rash

What is his greatest risk factor for progression to system disease? Age, gender, +ANA, + RF
+ANA
This is discoid SLE
+ ssA Ro or +ssB B- La
55 Yo F with PMHx Scleroderma who recently received steroids for a COPD exacerbation, she notes her reflux is a little worse. Vitals: HR 70, BP 150/80. Labs: CBC: schistocytess, cr 0.8-->1.4, LFT WNL
How will you treat her today?
a. calcium channel blocker
b. ace inhibitor
c. methlprednisolone
d. rituximab
ace inhibitor
This patient is in scleraderma renal crisis
RF: steroids (prednisone equiv>20mg/dl)
45 Yo M presents with recurrent conjunctivitis, otitis media, he comes into because he is coughing up blood and notes red bumps on his lower extremities.
VS: 99F, HR 100, 150/90 mmHg, RR 24, SaO2 94%

CBC WNL, BMP: Cr 1.8
UA: significant for protein
Negative MPO, C-ANCA 1-1000, PR3 1-120
CXRAY: cavitary lesion in LUL
Q: What is your dx?
A. Microscopic polyA
B. Eosinophilic granulomatosis with polyA
C. granulomatosis with polyA
D. polyA nodosa
C. granulomatosis with polyA
palp. purpura, sinusitis, lungs and renal involvement
renal: crescentic nephritis
38 Yo M carpenter who can no longer lift his tools, notes weakness started about 5 or 6 months ago. He has a rash on his hands shown below.

CK 15,000.
Q: What organ is at greatest risk for future complication given this patient's dx?
A. kidney
B. liver
C. lung
D. CNS
This patient has Dermato/Polymyositis, he is at risk for anti-synthase syndrome which manifests as iLD in the lungs
22 Yo M presents with three weeks of low back pain, most notable at night and early in the morning, better with activity.
labs: HCT 35, ESR 45

Q: what should you do next for this patient?
A. start NSAIDs
B. Order HLA-B27
C. order CT
D. order MRI
This patient has sacroilitis (Ank Spond)
start NSAIDs
inflammatory low back pain DDx
Spondoarthropathies (PAIR)
Infection (Potts, OM)
tumor (Prostate, breast, MM>>renal, liver, thyroid)
complications: require hip replacements (Ank Spond), enthesopathy (heel/rib pain), uveitis (painful red eye), cauda equina, amyloidosis, aortic insufficiency
27 Yo female presents to your office noting pain in joints, prior occurrence of pericarditis. Prior work-up includes +ANA, +Anti-Smith, low complement, +cardiolipin IgM, IgG. She does not have protein or blood in her urine. She briefly been on prednisone in the past.

Q: what medication should you start her on?
a. prednisone
b. mycophenolate
c. hydroxychloroquine
D. etanercept
hydroxychloroquine
this patient has SLE, I am also worried about APLS
hydroxychloroquine decreases SLE flares and risk of clots in APLS patients
All SLE patients should be on hydroxychloroquine unless they have a contraindication or can't tolerate
82 Yo F presents with temporal headache for the past two months, low grade fever and weight loss. She notes facial pain when chewing, change in vision in left eye last night
ESR 90
Q: what is your next step?
A. MRA temporal artery
B. temporal artery biopsy
C. patient needs IV methypred
D. obtain blood and urine cultures
The patient has giant cell arteritis with vision loss
(rheumatologic ER)
3/5 to dx temporal arteritis: headache, 50 y/o+, elevated ESR, + MRA, + biopsy
which small vessel vasculitis does not have granulomas on biopsy, can present with pulmonary hemorrhage and crescentic glomerular nephritis with +pANCA / MPO with normal c3/c4
a. Granulomatosis with polyangiitis
b. Microscopic polyangiitis
c. Eosinophilic granulomatosis with polyangiitis
d. polyarthritis nodosa
e. IgA vasculits
microscopic polyarthritis
72 yo M presents noting one month of difficulty rising from a chair. PMHx: HTN on losartan, HLD on statin.
Exam: 4/5 quad motor strength bilateral
CK: 11,000 AST 400 ALT 400
Q: what antibody do you expect to be positive?
A. histone
B. Jo1
C. HMG CoA reductase
D. SRP
This patient has necrotizing myositis (+HMG-CoA reductase) - note sudden onset
RF: statins
tx: steroids
55 Yo M notes pain in his hands and swelling in his fingers, it is hard to flex his fingers now. has a history of long standing low back pain


Q: What is his diagnosis?
A. Rheumatoid
B. SLE
C. Psoriatic arthritis
D. hemochromatosis
Psoriatic Arthritis
Pencil & Cup, dactylitis
joints: wrist, MCP, PIP, DIP
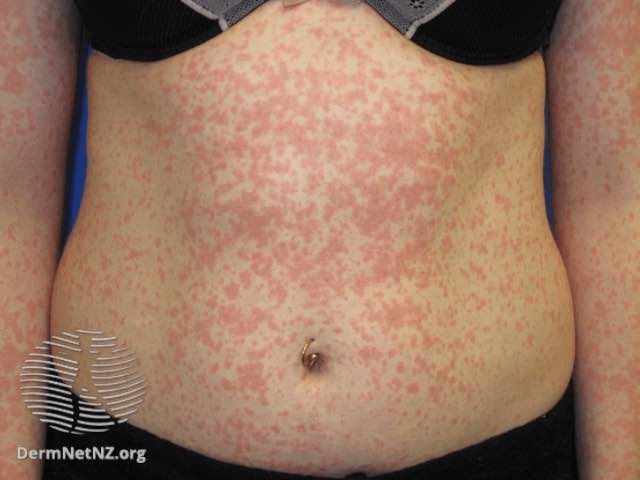
30 Yo F presents with low grade fevers, two months of arthralgias, rash shown below, last month had a sore throat with nasal congestion

CBC: WBC 3,000, Hb 11, platelets 130,000
BMP, LFTs WNL
Urine: 1+ protein and blood
Q: What test will you order next?
A. anti-mitochondrial Ab
B. ANA
C. HIV
D. RF / CCP
E. skin biopsy
livedo reticularis DDx: SLE, APLS, PAN, hep C, atherosclerotic embolic syndrome
30 Yo F elementary teacher noting three weeks of low grade fever (101) intermittent rash (see below), lumps on neck, sore hand, wrist and knees.
VS: temp 101, HR 100
cervical LAD
swollen knees and wrists
labs: WBC 25,000, Hb 11, AST 60, ALT 60, CRP 200
Q: next test?
A. ANA B. ferritin C. hep B D. Parvo IgM, IgG
This is still's disease (ferritin ~20,000-30,000)
prolonged low grade fever, polyarthralgia, LAD + labs
65 Yo M PMhx Hepatitis B, presents with 1 month of myalgia, numbness and weakness in right foot, dx 2 months ago with new onset hypertension. He has small necrotic ulcers on his legs.
VS: 99F, 165/90 mmHg,
CBC: Hb 10, WBC 13,000, platelet 430,000
ANCA: negative
UA: unremarkable
renal U/S: micro aneurysms of renal artery
deep skin biopsy: panmural necrosis of medium sized artery
Q: dx?
a. IgA vasculitis
b. microscopic polyarteritis
c. polyarteritis nodosa
d. Kawasaki
polyarteritis nodosa
(skin/renal/neuro + autoI or hep B)
Kawasaki - children, fever/rash, mucositis (I am worried their coronary arterities/pericarditis/aneursyms) - tx ASA/IVIG
50 Yo M prior professional football player presents with bilateral pain in his hands. Notes minimal pain in the morning, worse when using his hands a lot. A doctor placed him on MTX in the past without benefit.
Exam: tender MCP joints

Q: next step?
A. Order CCP
B. start NSAIDs
C. start low dose prednisone
D. Order ferritin
This patient has hemochromatosis, order ferritin
26 yo Female present with DOE, mylagias for six months, arm aches when doing physical activity with them. No rashes, headache, jaw pain. No neurologic or gastrointestinal symptoms.
Pex: HR 80, BP right arm: 120/70, left arm 95/60, RR 18. No rash. reduced radial pulse in left arm. lung clears. 2/6 decrescendo diastolic murmur at LSB.
CBC: Hb 10, WBC 9,000 platelets 200,000
BMP & UA: WNL
ANA: negative
TTE: notable for Aortic regurg, dilated aortic root, LV dilation with normal EF
Q: dx?
a. giant cell arteritis
b. IgA vasculitis
c. Kawaski disease
d. Polyartheritis nodosa
e. takayasu arteritis
Takayasu - granulomatous vasculitis, (large vessel, F age<30, claudication of UEx, aorta = AI