The three broad categories of AKI:
Pre-renal
Intrinsic
Post-renal
The target O2 saturation for patients admitted for COPD exacerbation
88-92%
An example of pseudo-hemoptysis:
GIB, epistaxis, S. marcescens/K. Pneumoniae sputum production, etc
A great app where you can get all up-to-date information on STIs (including screening, diagnosis, and treatment) is the:
CDC STI Tx App
![]()
The first-line pressor for ALL forms of shock with hypotension is
Norepinephrine (Levophed)
You will NEVER be wrong for picking this in a hypotensive patient
A sometimes-useful tool in determining the etiology of AKI is the FeNa. If your patient is on diuretics, this tool can be used instead
FeUrea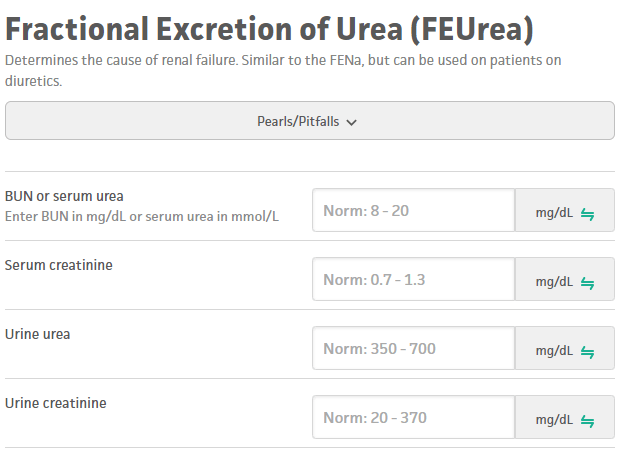
The classic dose/duration of prednisone for a COPD exacerbation
40mg
There is new data suggesting personalized doses based on body weight are more effective--stay tuned
The most common etiology of hemoptysis in the *outpatient* setting is
bronchitis
A 25F with no PMH presents with painful urination and mucopurulent vaginal discharge. She is otherwise in good health and has no other complaints. First-void urine is revealing for +chlamydia trachomatis, negative for gonorrhea. What should she be treated with (med, dose, and duration)?
Doxycycline 100mg BID x7d
Alternative options:
Azithro 1g once
Levofloxacin 500mg QDay x7d
The ventilator settings that affect oxygenation are
FiO2, PEEP
A 50M with ETOH-induced cirrhosis presents with worsening fatigue and jaundice. Labs demonstrate Cr 2.5 (baseline 0.8) which continues to worsen despite several days of albumin infusion and discontinuation of diuretics/beta blocker.
Renal is concerned for the presence of HRS. Which medication can be started at this time while initiating liver transplant workup?
Terlipressin + albumin (also accept midodrine/octreotide/albumin or levophed +/- vasopressin, if in ICU setting)
HRS--special type of AKI (arterial vasodilation triggered by by-products of liver failure, especially NO)
No one diagnostic test--rule out other etiologies/potential contributors, "albumin challenge" x48hrs, if no improvement
Dismal prognosis; need to fix underlying problem, high mortality within 3-6 months
A 45M with no PMH and a 5 pack-year history of smoking presents with cough and progressive SOB over the past 8 months. PFTs are notable for a post-bronchodilator FEV1/FVC of 60%. What lab test should be sent for evaluation of suspected COPD?
Alpha 1 antitrypsin; new to 2023 GOLD criteria, ALL patients with COPD should be screened for this
Patients with significant hemoptysis should be placed with the bleeding lung in the
Dependent position
A 32M with PMH HIV (CD4 180, most recent VLUD) presents with painful lesions as pictured below. He has lesions over >25% BSA. Swab returns positive for MPox. What medication should he be treated with (after consultation with ID)?

Tecovirimat (TPoxx)
Originally designed/stockpiled by US government for variola (smallpox) outbreak--currently approved under emergency use authorization (CDC) and under STOMP trial (NIH). Only medication with efficacy against MPox
You admit a 78M with PMH COPD on 2L who presents with severe flank pain and burning with urination. He is in septic shock; you start antibiotics and levophed, but MAPs remain consistently below 65 despite steady up-titration of levophed to 0.4 µg/kg/min. Which pressor should you add next?
Vasopressin
The Surviving Sepsis Campaign (SSC) 2021 proposes to start AVP in septic shock when the dose of norepinephrine (NE) base is in the range of 0.25–0.5 µg/kg/min
A 68M with PMH BPH, HTN, HLD presents with inability to urinate and tender suprapubic region x48hrs in the setting of running out of medications for the past several weeks. On exam he has a palpable suprapubic mass. Labs are notable for Cr 4.75 (baseline 0.8). He is started on tamsulosin/finasteride and a Foley is placed, draining 1.3L of urine.
What is the most likely complication now that this patient's post-obstructive AKI is resolved?
Post-obstructive natriuresis--excessive urine production with concomitant electrolyte abnormalities
A 72M with PMH COPD presents with wheezing, increased sputum production, and increased cough for the past 3 days. Exam is notable for diffuse wheezing, mild respiratory distress, use of accessory muscles, tachypnea (RR 30) and O2 sat 84%. The ED has already sent labs, and the patient is appropriately placed on BiPAP with marked improvement in symptoms and clinical appearance.
What lab finding would differentiate this patient's clinical presentation between a moderate and severe COPD exacerbation?
Presence of new/worsening respiratory acidosis on ABG
In a patient with large-volume hemoptysis progressing towards hemodynamic instability, this inhaled medication can be used in an attempt to staunch bleeding while other interventions are pursued:
TXA (tranexamic acid)
Not systemically absorbed, less risk of systemic thrombosis
A 23M with no PMH presents with complaint of intensely painful vesicles over his genitalia. He is currently sexually active with multiple partners and always uses condoms. What is the appropriate management of these lesions (med, dose, duration)?

HSV--condoms reduce, but do not prevent, transmission
Acyclovir 400mg TID x 7-10d
Famciclovir 250mg TID x 7-10d
Valacyclovir 1g BID x 7-10d
Can prolong therapy if not fully healed by 10d
According to the Surviving Sepsis 2021 guidelines, in patients with POSSIBLE septic shock, antibiotics should be administered within
1 hour (SAME as definite or probable septic shock)
A 65F with PMH ETOH-induced cirrhosis presents with decompensated cirrhosis in setting of ESBL E. Coli bacteremia 2/2 ascending UTI. Exam is notable for anasarca, jaundice, and other sequelae of chronic liver failure. On arrival Cr is 1.8 (baseline 0.6) which does not improve with antibiotics. Labs are notable for spec grav of 1.60 (high), FeNa indicates pre-renal etiology.
What is the next best step in management of this patient?
DIURESE
Paradigm of "extravascularly volume up, intravascularly volume down" is a misinterpretation. Glomeruli are "squished" by additional hydrostatic pressure which produces a pre-renal picture on labs; if patient is anasarcic without clear reason to avoid, consider diuresing first (rather than additional volume) in an anasarcic patient
A 68M with PMH COPD presents with acute worsening of dyspnea in the past 3 days. He endorses increased sputum production, increased purulence of sputum, and increased sputum volume. He is treated for a COPD exacerbation and started on antibiotic therapy, after which he improves rapidly.
What are the THREE indications for antibiotic therapy in COPD exacerbation?
1. Presence of all three cardinal symptoms – increase in dyspnea, sputum volume, and sputum purulence (Evidence B)
2. have two of the cardinal symptoms, if increased purulence of sputum is one of the two symptoms (Evidence C)
3. require mechanical ventilation (invasive or noninvasive) (Evidence B)
A 65F with PMH IIH, SLE off IS presents with acute-onset large-volume hemoptysis. She is hemodynamically stable but satting 82%, which improves to 96% with HFNC 40L/50% FiO2. On exam she is frequently coughing up moderate volumes of bright red blood with clots. CXR demonstrates diffuse bilateral parenchymal opacities (below). Diagnostic evaluation for suspected DAH involves:

Bronchoscopy with sequential BAL (lavage aliquots are progressively more hemorrhagic)
Also technically includes PFTs with DLCO above 100% of predicted; most patients with DAH are not stable enough for this
A 64M with PMH HTN, HLD presents for his annual physical. He has no complaints and feels well, although he does request STI screening as he has met a new partner and plans to become sexually active soon. He has not been sexually active in at least the past 5 years. Labs are notable for RPR 1:64 (no prior). What should he be treated with (med, dose, frequency, duration)?
IM PCN G, 2.4M U Qweek x 3 doses for late latent syphilis
Primary, secondary, or early latent syphilis (<1yr) = IM PCN G 2.4M U x1 dose
Late latent (>1yr), latent syphilis of unknown duration, or tertiary syphilis = above treatment
Neuro/ocular/otic syphilis = IV PCN 18-24M U QDay x10-14 days
The 2012 Berlin Criteria for ARDS include (name all 4):
1. Acute onset (within 1wk of insult)
2. Bilateral opacities
3. Respiratory failure not fully explained by volume overload or cardiac failure
4. PaO2/FiO2 <300 (sub-stratified by severity)