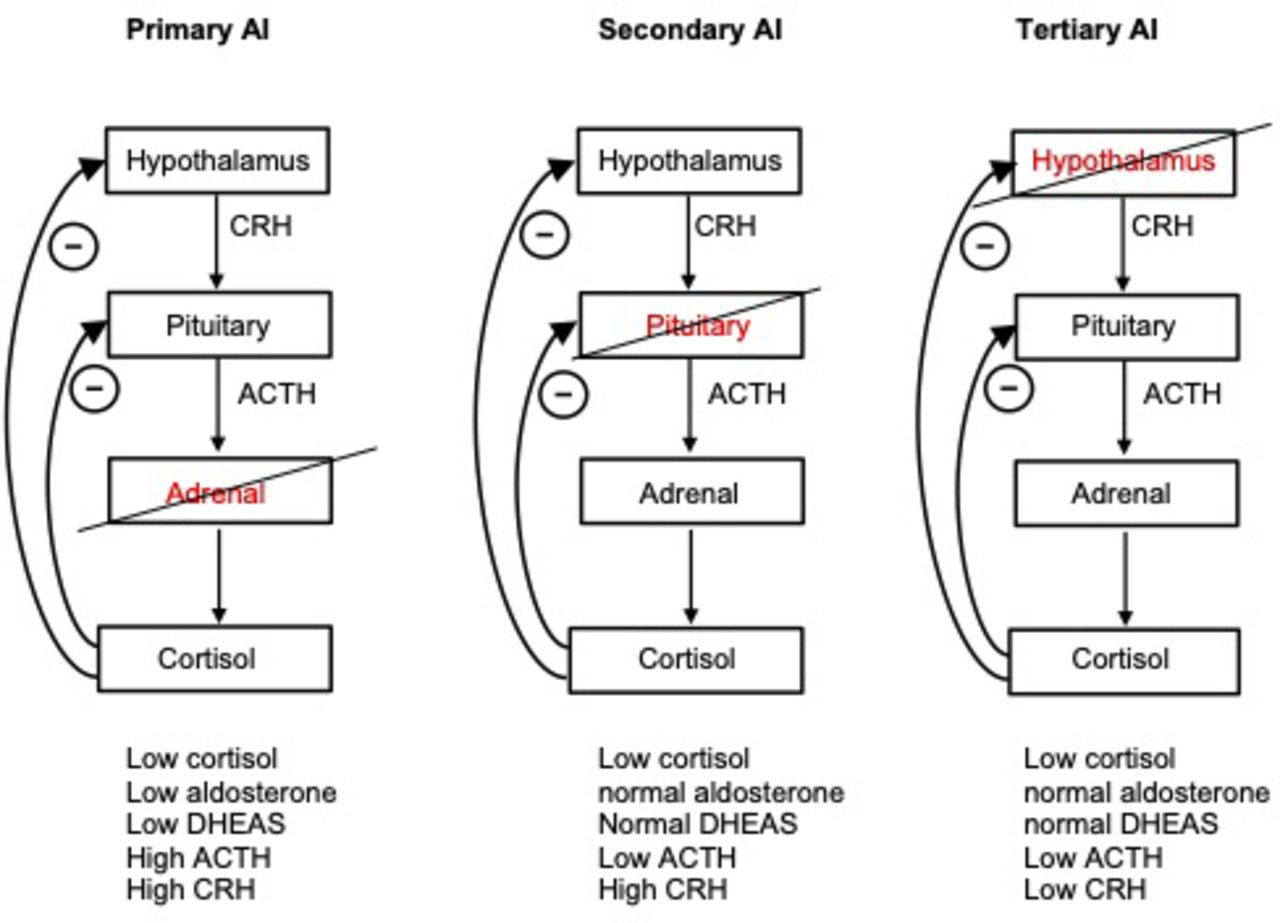
Please describe Primary vs Secondary vs Tertiary Adrenal insuff
How is IAP classified
IAP can be classified as Grade 1 (10–15 cm H2O), Grade II (15–25 cm H2O), Grade III (25–35 cm H2O), or Grade IV (>35 cm H2O). As the IAP increases through Grades II, III and IV, the degree of organ dysfunction progressively worsens.
Most patients with Grade III and all patients with Grade IV require abdominal decompression
What is the technical name for the Whipple procedure and who is the Surgeon the procedure is named after
pancreaticoduodenectomy, named after Allen Whipple
Perioperative stroke commonly occurs within ___ days after surgery and presents as an ____ neurologic deficit.
This could include a decrease or loss of motor function, facial droop, decreased sensation, alteration of speech, or mental status such as delirium, lethargy, or decreased responsiveness, which might be confused with sedation and pain. These acute neurologic deficits may be temporally associated with risk factors like changes in blood pressure, cardiogenic shock, atrial fibrillation, or supratherapeutic anticoagulation.
The timing of presentation may vary with anastomotic location. Gastrojejunal leaks after gastric bypass surgery usually present ____ and small bowel or colon leaks more typically present between ____ after surgery.
Helpful labs?
present early (<24 hours)
5-7 days
Laboratory tests like complete blood test, C-reactive protein, and procalcitonin may be elevated with anastomotic leak but are considered relatively nonspecific.
Patients taking more than ___ mg/day of prednisone or an equivalent dose for more than __ weeks or who have a clinical presentation of Cushing syndrome are considered ____risk for HPA suppression.
20, 3, High risk - should be given stress dose steroids during surgery
After abdominal surgery, there is a normal time course and pattern for return of intestinal motility. The small bowel usually develops contractile activity within ___ hours, the stomach requires ___ hours, and the colon recovers ___ days after surgery.
Small bowel - several hours
Stomach - 24-48hrs
Colon - 3-5 day
Define: Critical view of safey
It is essential that there is an understanding of the importance of obtaining the "critical view of safety" of the cystic triangle, which includes:
- Clearing the hepatocystic triangle of fat and fibrinous tissue
- Separating the lower third of the gallbladder from the liver to expose the cystic plate
- Visualizing two—and only two—tubular structures entering the gallbladder
Benzodiazepines are the first-line medications to stop seizures, especially IV lorazepam or diazepam. Intramuscular midazolam or IV phenobarbital can be used if lorazepam is not available or contraindicated
Risk factors for Fistulas.
What defines low vs high output?
FRIEND
that stands for foreign body, radiation, inflammatory bowel disease, epithelialization, neoplasia, and distal obstruction.
The fistula output over a 24-hour period is the most important determinant of its physiologic impact (on fluid and electrolyte status) on the patient and guides management. ECFs can be classified as
low (<200 mL/day), moderate (200–500 mL/day), or high (>500 mL/day) output.
Describe the ACTH Stimulation test
Obtain baseline serum cortisol.
●Administer cosyntropin 250 mcg (85 nmol, or 40 international units [the entire contents of the vial]) via intravenous (IV) or intramuscular (IM) injection [24].
●Obtain serum cortisol again at 30 and 60 minutes post-injection.
- Cortisol is < 14 = adrenal insuff likely
- Cortisol > 18 = Normal adrenal function
What is the definition of abdominal compartment Syndrome
What are major risk factors
It is defined as sustained increased IAP greater than or equal to 12 mm Hg along with new organ dysfunction or organ failure and improvement after abdominal decompression.
Primary ACS develops as a result of intraabdominal pathology (blunt or penetrating abdominal trauma, hemorrhage, abdominal aortic aneurysm rupture, intestinal obstruction, retroperitoneal hematoma).
Secondary ACS develops in the absence of abdominal injury and is described in patients with severe burn injury, multiple extremity fractures, and/or septic shock.
What is the most common CT imaging that would suggest injury to the hepatic artery
The most common CT scan finding suggestive of hepatic artery injury is nonenhancement of the right lobe during the arterial phase.
Define Delirium vs Dementia
Delirium - acute onset, underlying correctable pathological cause
Dementia - Chronic, slow onset, decrease in cognitive skill
Discuss treatment options for Low vs Moderate vs High output fistula

In hypotensive patients considered to be in adrenal crisis; what is the basal serum cortisol level that suggests diagnosis of adrenal insufficiency. What is the next test to confirm diagnosis.
a basal serum cortisol level <18 mcg/dL (<500 nmol/L) suggests the diagnosis of adrenal insufficiency. To confirm the diagnosis of adrenal insufficiency, ACTH stimulation testing should be performed at a later date.
Stress gastritis is more commonly seen in critically ill patients. What are high risk factors that would indicate stress ulcer prophylaxis
mechanical ventilation, coagulopathy (INR >1.5, platelet count <50,000, aPTT >2 times normal), hypoperfusion, significant burn, severe brain or spinal cord injury, multisystem trauma, and sepsis.
If taking a PPI prior to admission: Resume home PPI
What is the Bismuth-Strasberg classification system.

Delirium - Mnemonic for common risk factors
Toxic (shock, organ failure,
deliriogenic meds)
Hypoxemia
Infection
Non-pharmacologic causes
K+ or other electrolyte problem
Drugs
Eyes & Ears
Low O2 state (MI, stroke, PE)
Infection
Retention of urine or stool
Ictal
Underhydration/Undernutrition
Metabolic
(S)ubdural
Including myocardial infarction, stroke, seizure, electrolyte imbalance, hypoxia, hypothermia, hypoglycemia, and acidosis.
Absent treatable medical causes for POD are nonpharmacologic interventions, including cognitive reorientation, decreasing sleep disturbance, optimizing nutrition, fluid and oxygenation, providing hearing and vision aids, etc., that are preferable.
Common causes of postoperative bowel obstruction
Adhesions are responsible for the majority of early postoperative bowel obstructions (>90%), with internal herniation, intra-abdominal abscess, intramural hematoma, intussusception, and anastomotic edema or leak as less likely causes.
Vasopressin (ADH) is normally released in response to high serum osmolality but is also released in response to systemic stress (e.g., surgery) and inflammation.
What is the clinical Syndrome of SIADH
The clinical syndrome of SIADH consists of hyponatremia, inappropriately elevated urine osmolality, excessive urine sodium, and decreased serum osmolality in a euvolemic patient without edema;
SIADH - increase ADH - Renal tubules permeable to water - increase free water Reabsorption -> dilutional hyponatremia -> Concentrated urine sodium

pathophysiology of postoperative ileus
- what interleukin are thought to contribute to postoperative Ileus
IL-6 and IL-8
According to the Strasberg classification; what type of injury would require a Roux-en-Y hepaticojejunostomy repair
- Injuries E1-E5
- E1 injuries with > 2 cm of healthy CHD can be repaired with Roux-en-Y hepaticojejunostomy.
- E2 or E3 injuries with < 2 cm healthy CHD, exposure of the hepatic duct confluence by lowering the hilar plate to perform a biliary-enteric anastomosis is required for repair; transanastomotic stents may be used.
- E4 injuries that completely separate L and R hepatic ducts need separate biliary-enteric anastomosis to each duct; if inadequate extrahepatic ducts remain, intrahepatic duct can be isolated through the hepatic parenchyma and used for anastomoses; stents may be used.
- E5 injuries typically require the use of transanastomotic stents in addition to a biliary-enteric anastomosis.
What it artery(s) that results in Posterior epistaxis bleed and what is the current management ?
Woodruff's plexus, the rear, and fine terminal branches of the sphenopalatine and posterior ethmoidal arteries
The current management of posterior epistaxis includes combined anterior posterior packing, angiographic embolization, arterial ligation, and endoscopic electrocautery.
The presence of oral contrast in the large bowel at __ hours post-administration has been shown to predict the resolution of small bowel obstruction with ___ sensitivity and __ specificity
The presence of oral contrast in the large bowel at 24 hours post-administration has been shown to predict the resolution of small bowel obstruction with 97% sensitivity and 96% specificity