A pathogen is...
a) a living thing.
b) an agent that causes infectious and non-infectious diseases.
c) an agent that causes an infectious disease.
d) an agent that results from genetics.
c
What is the innate immune system?
The immune system that provides a generalised, non-specific response to pathogens.
Name the three types of phagocytes.
- Neutrophils, macrophages, dendritic cells
Why is the third line of defence said to be 'adaptive'?
Because it responds differently to each individual pathogen / antigen.
Name the fluid that flows through the lymphatic system.
Lymph
Name the four types of cellular pathogens.
Fungi
Bacteria
Worms (parasites)
Protozoa
A plant has thorns on its branches to prevent animals from eating it. What type of defence is this?
Physical
What cell releases histamine? What is the role of histamine in an immune response?
- Mast cells
- Causes vasodilation of blood vessels, allowing from increased blood supply and vessel permeability.
There are two immune responses that occur in the third line of defence. Name the response and the group of cells that are associated.
Cell mediated - T cells
Humoral - B cells
Where are B and T cells formed? Where do they mature?
Both are formed in the bone marrow. B cells mature here too, whereas T cells mature in the thymus.
Explain why someone may develop an allergy to a peanut.
The person's immune system will overreact to the presence of the allergen (peanut), triggering an immune response.
Define 'physical barrier'
The use of a solid or fluid that prevents the pathogen from invading.
NK Cells are large granulated cells that target both abnormal and virally-infected cells. Name the two receptors found on the surface of an NK cell. Then, outline how a cell would avoid death by an NK cell.
Killer inhibitory receptor & Killer activation receptor
If the killer inhibitory receptor detects a sufficient number of MHC Class I markers, then it overrides the killer activation signal, preventing cell death. Cell death is only initiated in infected or abnormal cells with missing MHC Class I markers
What is the role of Th cells? What part(s) of the third line of defence is/are they involved with?
Th cells assist both the cell-mediated and humoral responses.
What happens in the lymph nodes?
B and T cells gather and attach to foreign antigens.
Explain why a virus is not classified as a cellular pathogen.
Because it is unable to reproduce on its own, so must inject its genetic material into a host, hijaking its machinery, allowing it to replicate.
What is an example of a microbiota barrier in humans?
Bacteria in the stomach or on skin
Outline the process of phagocytosis.
1) Pathogen is engulfed by phagocyte via phagocytosis, and stored in a vesicle.
2) The vesicle containing the pathogen fuses with a lysosome.
3) Enzymes (ie. lysozyme) starts to break down the pathogen.
4) Fragments of the pathogen are presented on MHC Class II markers.
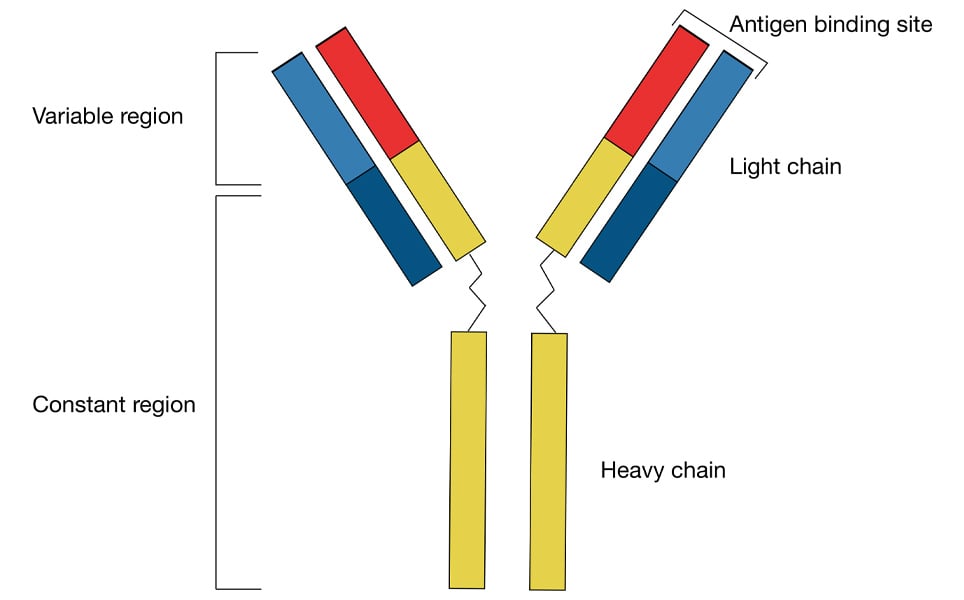
Draw an antibody and label four key parts.
State two key roles of the lymphatic system
Site of maturation of lymphocytes.
Act as a transport system for APCs and pathogens.
Site of clonal selection and expansion.
Stores memory cells.
Name the two most important self antigens, and the types of cells they are found on.
MHC Class I markers - expressed on all nucleated cells (not RBCs)
MHC Class II markers - found on APCs
Explain why tears are classified as a chemical barrier in humans.
Tears contain lysosymes, which is an enzyme that attempts to interfere with pathogen activity through altering its structure (cell walls)
Outline the inflammatory response.
1) INITIATION - The pathogen enters the body, stimulating macrophage activation in affected tissues. Damaged cells release cytokines, causing mast cells to release histamine.
2) VASODILATION - Histamine binds to blood vessel receptors, causing vasodilation. Gaps in the blood vessel walls form, increasing permeability to immune cells. The injury site becomes swollen, red, and warm.
3) MIGRATION - Phagocytes (macrophages and neutrophils) are guided to damaged cells by cytokines. Pathogens become phagocytosed and digested by enzymes such as lysozymes. Complement proteins act on pathogens, making it easier for phagocytes to destroy them.
Outline the process involved in manufacturing antibodies (4 marks)
An APC presents an antigen on its MHC II Markers (1).
A Th cell releases cytokines, activating a complementary naive B cell (clonal selection) (1).
B cell undergoes clonal expansion, making lots of copies of the selected naive B cell (1).
B cells differentiate, forming memory B cells and plasma cells, which secrete antibodies that target the pathogen (1).
What is the difference between an efferent lymphatic vessel and an afferent lymphatic vessel?
Afferent lymphatic vessels - transport lymph towards the lymph node.
Efferent lymphatic vessels - transport lymph away from the lymph node.