30 yo M snowboarder brought in with aa femur fx and abdominal pain. Denies LOC. GCS 15, BP 98/60 mmHg and HR 112 bp. CT abdomen/pelvis reveals grade 2 liver laceration and grade 3 right renal laceration without urine extravasation. The following factor causes the greatest potential increase in morbidity in this patient.
a) Grade of liver laceration
b) Initial GCS
c) Age
d) Heart rate on admission
e) Initiating VTE prophylaxis at 72 hrs
Initiating VTE prophylaxis at 72 hrs
Patients progress from hypocoagulable to hypercoagulable around 12 hrs after trauma.
What are the 3 peaks in trauma deaths?
0-30 minutes: hemorrhagic shock
30min-4 hrs: TBI mcc of death in trauma pts reaching the hospital alive, these pts can be saved with rapid assessment (golden hour), preventing secondary injury to the brain by avoiding hypotension and hypoxia
days to weeks: deaths due to multisystem organ failure and sepsis
Hard Signs in penetrating neck injury
Bleeding, Emphysema or bubbling at wound, Neurologic deficit, Hemorrhagic Shock, Hematemesis, Airway Compromised, Pulsatile or Expanding Hematoma
The early sepsis triad
hyperventilation, confusion and hypotension
Describe GSC components and which is the most important prognostic indicatory?
Motor: 6- follows commands, 5-localizes pain, 4-withdraws from pain, 3-flexion with pain (decorticate), 2-extension with pain (decerebrate), 1-no response
Verbal: 5-oriented, 4-confused, 3-inapproopriate words, 2- incomprehensible sounds, 1-no response
Eye opening: 4-spontneous opening, 3-opens to command, 2-opens to pain, 1-no response
45 yo man presents with second and third degree burns to the anterior surface of both arms and entire right leg. He also has superficial burns to both hands. What is his estimated total body surface area burned?
27%
Upper extremity account for 9% (anterior =4.5%), each lower extremity accounts for 18%, anterior and posterior trunk each accounts for 18%, the head and neck account for 9%, hands are 1% each and the perineum account for 1%. First degree burns are not included.
Explain Denver criteria and list at least 3 risk factors.
Used to screen for vertebral and carotid artery dissection and/or injury after blunt head and neck trauma
Signs and Symptoms
- Arterial hemorrhage
- Cervical bruit
- Expanding neck hematoma
- Focal neurologic deficit
- Neuro exam inconsistent with head CT
- Stroke on head CT
Risk Factors
- Midface Fractures (Le Fort II or III)
- Basilar Skull Fracture with carotid canal involvement
- Diffuse axonal injury with GCS<6
- Cervical spine fracture
- Hanging with anoxic brain injury
- Seat belt abrasion or other soft tissue injury of the anterior neck resulting in significant swelling or altered mental status
- Isolated seatbelt sign without other neurologic symptoms has not been identified as a risk factor

- Isolated seatbelt sign without other neurologic symptoms has not been identified as a risk factor
33 yo M, caught in a residential fire, suffers burns covering 50% of his total body surface area. Immediate intubation was performed at the scene & IV fluid resuscitation was started. Upon arrival at the emergency department, the patient's vistal signs were as HR 110, BP 140/73, with respirations maintained by a bag valve mask achieving an O2 sat of 98%. An initial assessment shows severe bilateral chest wall burns. Despite the continuation of mechanical ventilation, the intensivist ovserves that the patient is increasingly harder to ventilate. The patient's peak airway pressures are 36 cmH20 with an arterial oxygen saturation of 90%. An urgent ABG reveals a Pa02 of 55mmHg & a PaCO2 of 60 mmHg. There are no signs of pneumothorax or parenchymal disease on the chest x-ray. The patient's urine output is satisfactory & bladder pressures are recorded at 12 mmHg. What would be the optimal course of action to enhance this patient's respiratory condition?
Perform bilateral chest escharotomies along the mid-axillary lines & a transverse incision may be needed if the eschar extends onto the abdomen.
Concern for what type of fracture after flexion-distraction injury from rapid deceleration during blunt trauma?
Chance Fracture (horizontal disruption of all columns)
Location: Thoracolumbar
Management: Orthotic brace for low grade injury, surgery if neurologic deficits or ligamentous injury; also HIGH RISK of hollow viscous injury
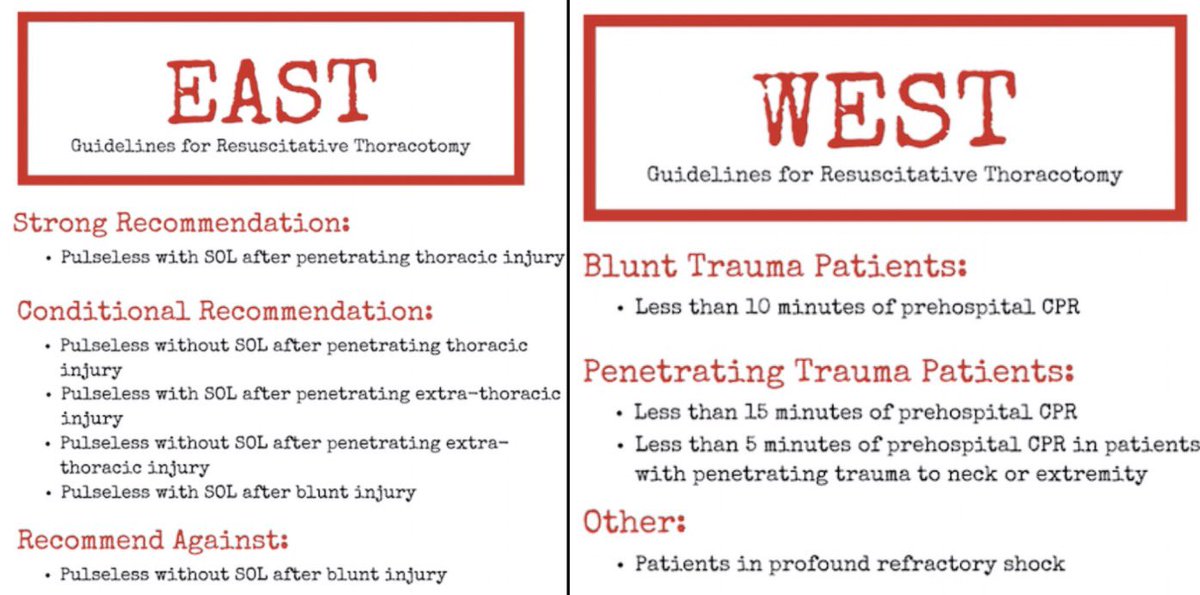
Best indications for ED Thoracotomy
Stab wound to the chest with agonal breathing on transport, loss of pulse in ED
Signs of life were considered present with any of the following: pupillary response, spontaneous ventilation, presence of carotid pulse, measurable or palpable blood pressure, extremity movement, or cardiac electrical activity.
45 yo M presents to the ED with multiple GSW wounds to the Right upper extremities. Vitals: HR-105, BP- 95/60 Weak distal pulses with delayed capillary refill. What grading system is used to evaluate?
Mangled Extremity Severity Score (MESS)
7 or higher correlates well with primary amputation
- Skeletal/soft tissue injury
- Low energy (stab, pistol gunshot, fracture) – 1 point
- Medium energy (multiple/open fractures) – 2 points
- High energy (high-speed motor vehicle collision, rifle) – 3 points
- Very high energy (+gross contamination) – 4 points
- Limb ischemia
- Reduced pulse but normal perfusion – 1 point
- Pulseless, abnormal perfusion – 2 points
- Paralyzed, insensate – 3 points
- Shock
- Systolic blood pressure greater than 90 mm Hg – 0 points
- Transient hypotension – 1 point
- Persistent hypotension – 2 points
- Age
- Younger than 30 years of age – 0 points
- Age 30 to 50 years – 1 point
- Older than 50 years – 2 points
67 yo M is POD 6 from an open sigmoid colectomy for perforated diverticulitis with feculent peritonitis. He is intubated preoperatively for septic shock and has remained on mechanical ventilation. His hemodynamics have normalized on minimal vasopressors, and he is receiving full enteral nutrition. Ventilator settings include: FiO2 40%, PEEP 5cm H20, tidal volume 450 mL, RR 14. ABG shows pH 7.39, PaCO2 42, PaO2 92. In spontaneous mode, he has a RR of 30, RSBI of 110 and NIF of -28 cm H20. He is alert and follows commands. Which of the following is the most appropriate next step in management?
Begin a SBT with low level pressure support
Weaning Criteria: hemodynamic stability, adequate oxygenation, minimal vent settings, adequate respiratory muscle strength and appropriate mental status. RSBI is slightly higher then traditional cutoff of 105 but should not be used in isolation.
7-year-old falls from monkey bars. X-ray shows a displaced extension-type supracondylar fracture. The hand is pulseless but well-perfused (pink). Best next step?
Urgent reduction/pinning; many regain pulse afterward
Persists after closed reduction requires immediate vascular exploration.
Associated Neurovascular Injury: Brachial artery
Complications: Forearm compartment syndrome, Volkmann ischemic contracture
What is class 2 hemorrhagic shock?
Class 2: 15-30% blood loss with increased HR, normal BP, narrowed pulse pressures
A patient with TBI has MAP 80 mmHg and ICP 25 mmHg. What is the CPP?
CPP = 80 – 25 = 55
Supportive treatment for elevated ICP includes keeping CPP >60 (give volume and pressors to improve MAP)
What scoring system has a direct association with mortality and survival probability after traumatic injury?
Injury Severity Score (ISS)
It takes only the highest Abbreviated Injury Scale (AIS) score in each region
ISS = sum of squares for the highest AIS grades in the three most severely injured ISS body regions
scores range from 1 to 75
single score of 6 on any AIS region results in automatic score of 75
