An 11-year-old boy is brought to the emergency department by his parents because of episodic abdominal pain and stools with blood and mucus. During each episode, the patient pulls both knees to his chest. Physical examination reveals a finding shown in the image. Endoscopy reveals multiple hamartomatous polyps in the small intestine.
Which of the following is the most likely diagnosis? (no answer choices)

Peutz-Jeghers syndrome
- Peutz-Jeghers syndrome presents with multiple hamartomatous polyps that can lead to obstruction and with hyperpigmentation of the mouth, lips, hands, and/or genitalia.
The other choices are incorrect:
- Familial adenomatous polyposis and its subtypes, Gardner syndrome and Turcot syndrome, are associated with thousands of colonic polyps, though not typically hamartomatous polyps. The diseases are not associated with hyperpigmented lip macules.
- Hamartomatous polyps can occur in patients with juvenile polyposis syndrome, but hyperpigmented lip macules are not present.
A 34-year-old man presents to his primary care physician for his yearly physical examination. He recently began experiencing a burning sensation below his sternum and a sour taste in his mouth. Treatment is initiated with as-needed famotidine for symptom relief.
Which of the following best describes the mechanism of action of the drug prescribed for this patient?
A. Bind to and inhibit the H+/K+-ATPase of parietal cells
B. Binds to M3-receptors
C. Binds to and activates prostaglandin receptors
D. Binds to and inhibits histamine receptors
E. Somatostatin analog that binds to receptors
D. Binds to and inhibits histamine receptors
- \Histamine H2-receptor antagonists, such as ranitidine, famotidine, and cimetidine, bind to and inhibit Gs-coupled histamine H2-receptors, thereby decreasing hydrogen ion secretion by parietal cells and relieving the symptoms of heartburn and reflux.
The other choices are incorrect:
- Proton pump inhibitors bind to and inhibit the H+/K+-ATPase of parietal cells. These are usually first-line medications for the treatment of gastroesophageal reflux disease.
- Anticholinergics, such as atropine, bind to M3-receptors to block their interaction with acetylcholine, which normally stimulates acid secretion from the stomach.
- Prostaglandins bind to prostaglandin receptors on parietal cells, resulting in decreased acid secretion, increased mucin and bicarbonate secretion, and stimulation of epithelial cell proliferation.
- Octreotide binds to and inhibits activation of somatostatin receptors, resulting in the inhibition of secretion of motilin, secretin, gastrin, vasoactive intestinal peptide, insulin, and glucagon in the gastrointestinal system.
A 40-year-old male presents to the office because of burning retrosternal chest pain after meals. The pain improves with antacids. He denies nausea, vomiting, palpitations, and syncope. The physical examination shows an obese male with normal vital signs and a normal physical examination. The ECG is normal. Upper endoscopy reveals proximal dislocation of the gastroesophageal junction 3 cm above the diaphragmatic indentation of the esophagus and erosive changes in the lower esophagus.
This patient is at most increased risk of developing which of the following conditions?
A. Achalasia
B. Esophageal adenocarcinoma
C. Gastric adenocarcinoma
D. Metaplastic atrophic gastritis
E. Mucosa-associated lymphoid tissue lymphoma
F. Squamous cell carcinoma of the esophagus
B. Esophageal adenocarcinoma
- A sliding hiatal hernia can manifest with symptoms of GERD, which causes burning postprandial retrosternal pain.
- GERD is associated with an increased risk of Barrett esophagus that can progress to esophageal adenocarcinoma.
The other choices are incorrect because they are not consequences of GERD:
- Mucosa-associated lymphoid tissue lymphoma is a type of non-Hodgkin lymphoma, often occurring in the stomach. There is a strong association between this type of lymphoma and infection with Helicobacter pylori, as well as chronic autoimmune disease (eg, Sjögren syndrome).
- Achalasia is caused by the degeneration of motor neurons in the esophageal wall.
- Squamous cell carcinoma of the esophagus is associated with tobacco and alcohol use. It tends to involve the proximal and middle sections of the esophagus.
- Gastric adenocarcinoma is associated with H pylori infection, nitrosamine exposure, excessive salt intake, and low intake of fresh fruits and vegetables.
- Metaplastic atrophic gastritis can be autoimmune or due to H pylori infection. It is a risk factor for pernicious anemia (with decreased vitamin B12 absorption) and for neuroendocrine stomach tumors (carcinoid) and adenocarcinoma of the stomach.
A research study used healthy volunteers to determine baseline concentrations of electrolytes in gastrointestinal secretions. Subjects consumed a bolus of food, and investigators measured flow rate, electrolyte concentrations, and pH at multiple sites along the gastrointestinal tract. The data obtained from one collection site were used to construct the figure shown. 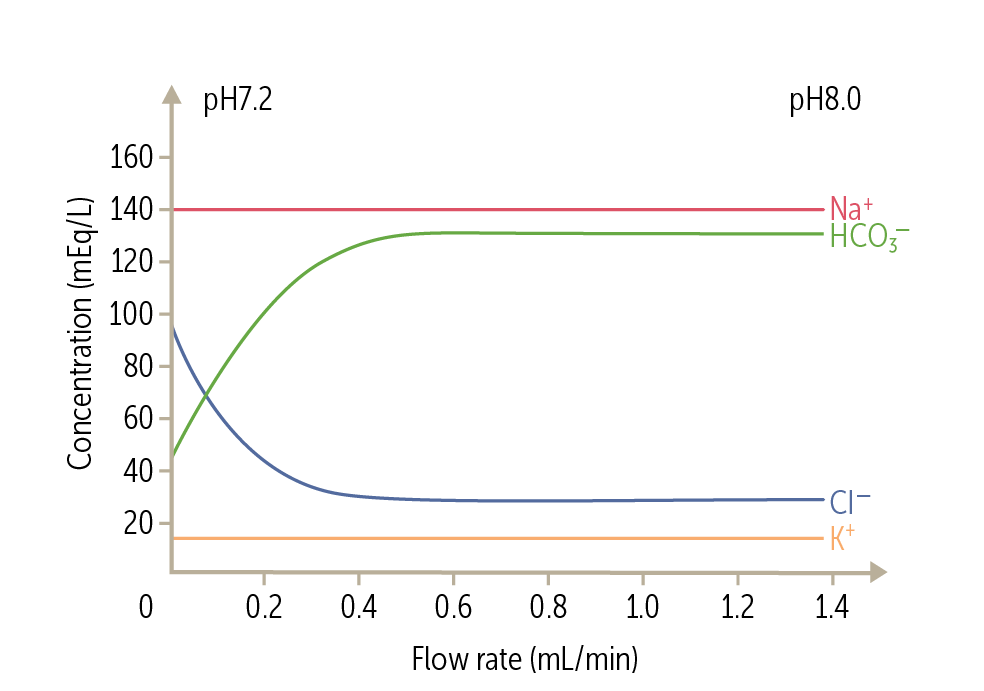
Which of the following organs is most likely responsible for the changes recorded on the graph?
A. Duodenum
B. Gallbladder
C. Pancreas
D. Salivary Glands
E. Stomach
C. Pancreas
- After food consumption, the exocrine pancreas responds to secretin by increasing flow rate. The bicarbonate concentration of pancreatic juice increases and its chloride concentration correspondingly falls as the rate of secretion increases. The sum of these anions is constant and almost equals that of the sodium and potassium concentrations, which are independent of flow rate.
The other choices are incorrect:
- At low flow rates, the salivary ducts reabsorb more NaCl, which makes the solution hypotonic, while the solution is more isotonic at higher flow rates.
- The concentrations of electrolytes in stomach and duodenal secretions do not change at varying flow rates.
- The gallbladder secretes acidic bile, so there would be a decrease in pH at increasing flow rates.
What is my favorite animal?
Dogs (duh)
A 24-hour-old boy is brought to the pediatrician because of poor appetite and constipation since birth. On physical examination, the abdomen is distended but nontender, and bowel sounds are normoactive. Barium enema shows a narrow rectosigmoid colon with dilation of the proximal segment.
What condition is associated with this patient's disease? (no answer choices)
Down syndrome
- Hirschsprung disease, also known as congenital megacolon, occurs due to failure in the migration of neural crest cells to the distal colon, which causes constriction of the aganglionic segment with proximal dilation, inducing severe constipation soon after birth.
- Hirschsprung disease is associated with Down syndrome.
The other choices are incorrect:
- Cystic fibrosis often presents with meconium ileus due to inspissated (dried-out) stool but not a narrowing of the rectosigmoid area.
- Fragile X syndrome and Turner syndrome are not associated with narrowing of the rectosigmoid area.
- Patau syndrome is not associated with the failure to pass stool or a narrowing of the rectosigmoid area, making this answer choice less likely.

A 29-year-old woman presents with difficulty swallowing solids and liquids for the past 9 months. A barium swallow study shows dilation and tapering of the esophagus and concentric distal stenosis.
The best drug for treating this patient’s condition has which of the following mechanisms of action?
A. Blocking the action of histamine at H2 receptors on parietal cells
B. Blocking the synthesis of pyrimidines (eg, thymidine)
C. Decreasing calcium availability in smooth muscle cells
D. Decreasing proton secretion into the stomach lumen
E. Enhancing the phosphorylation of myosin light chains
C. Decreasing calcium availability in smooth muscle cells
- Patients with achalasia often present with difficulty swallowing both solids and liquids.
- Achalasia is characterized by a loss of ganglion cells in the myenteric (Auerbach) plexus.
- Medical treatments for achalasia include calcium channel blockers, nitroglycerin, and botulinum toxin injection, which help to relax the lower esophageal sphincter
The other choices are incorrect.
Some of the choices are drugs used to treat gastroesophageal reflux disease:
- Proton pump inhibitors (eg, omeprazole) work by decreasing proton secretion into the stomach lumen.
- H2 receptor antagonists work by blocking the action of histamine at H2 receptors on parietal cells, resulting in decreased gastric acid secretion
The other choices are implicated in other disorders:
- Enhancing phosphorylation of myosin light chains would enhance muscle contraction within smooth muscle and worsen the symptoms of achlasia cardia.
- Inhibiting the degradation of acetylcholine describes acetylcholinesterase inhibitors (eg, physostigmine), which are used to treat atropine poisoning, reverse the effects of neuromuscular junction blockers (eg, pancuronium), and treat myasthenia gravis.
- 5-Fluorouracil acts by blocking the synthesis of pyrimidines (eg, thymidine) and is used to treat esophageal cancer.
A 27-year-old woman with a history of diarrhea and gastrointestinal bleeding undergoes a colonoscopy. Results reveal hundreds of adenomatous polyps located diffusely throughout her colon. Her family history is significant for colon cancer in her father and paternal grandmother.
Which of the following patterns of genetic mutation is characteristic of the most likely diagnosis in this patient?
A. Autosomal dominant
B. Autosomal recessive
C. Germline mutation
D. Somatic mutation
E. X-linked recessive
A. Autosomal dominant
- FAP is an inherited cancer syndrome that presents with early onset of hundreds to thousands of adenomatous polyps found throughout the colon.
- FAP is an autosomal dominant condition caused by mutation of the APC gene.
The other choices are incorrect:
- Autosomal recessive disorders are usually seen in only one generation.
- Germline mutations arise sporadically in gametes of individuals without disease and are passed on to offspring, who will phenotypically express the disease.
- Somatic mutations arise sporadically.
- The full effects of X-linked recessive conditions are usually absent or reduced in females due to the presence of another X chromosome.
A 25-year-old female comes to her primary care physician after learning about an extensive history of colon cancer in her family. Her mother and maternal uncle were diagnosed with colon cancer before the age of 50. The woman’s sister had endometrial cancer and a tumor of the small intestine. The physical examination is normal. A colonoscopy shows flat polyps in her cecum. One year later, a repeat colonoscopy shows malignant transformation of some polyps. Molecular testing shows a mutation in a DNA mismatch repair gene.
Which of the following is the most likely diagnosis?
A. Familial adenomatous polyposis
B. Gardner syndrome
C. Hereditary nonpolyposis colorectal cancer
D. Peutz-Jeghers syndrome
E. Turcot sydrome
C. Hereditary nonpolyposis colorectal cancer (lynch syndrome)
- Lynch syndrome is an autosomal-dominant mutation of DNA mismatch repair genes that conveys an increased risk for colorectal cancer and other cancers, including those found in the gastrointestinal, urinary, and female reproductive tracts.
The other choices are incorrect. The following choices are not associated with a DNA mismatch repair gene mutation:
- Familial adenomatous polyposis is an autosomal-dominant mutation that predisposes patients to colorectal cancer but not to the other malignancies seen in this family history.
- Gardner syndrome is an autosomal-dominant mutation predisposing patients to colorectal cancer, as well as bone and soft tissue tumors, but not to the other malignancies seen in this family history.
- Peutz-Jeghers syndrome is an autosomal-dominant syndrome featuring multiple nonmalignant hamartomas throughout the gastrointestinal tract, along with hyperpigmented macules around the mouth, lips, hands, and genitals.
- Turcot syndrome is a rare genetic disorder in which patients present with hundreds of colonic polyps in addition to malignancies of the central nervous system, but not the other malignancies seen in this family history.
What is my favorite color?
Black/gray
A 1-year-old boy is brought to the office because of irritability for the past 3 days. He has episodes of inconsolable crying with vomiting and has passed only one stool in the past 2 days, which contained blood and mucus. He has no past medical history and has achieved all age-appropriate milestones. Temperature is 38.9°C (102.1°F), pulse is 150/min, and respirations are 44/min. On physical examination, the abdomen is distended, and the patient cries with palpation. An x-ray of the abdomen reveals dilated loops of small bowel.
Which of the following is this patient’s most likely diagnosis?
A. Appendicitis
B. Duodenal atresia
C. Hirschsprung Disease
D. Intussusception
E. Pyloric Stenosis
D. Intussusception
- Intestinal obstruction in an infant, especially when associated with gastrointestinal bleeding, suggests intussusception as the most likely cause.
The other choices are incorrect:
- Duodenal atresia is characterized by failed recanalization of the mucosal lumen. This diagnosis manifests with symptoms of an acute bowel obstruction within hours to days after birth.
- Hirschsprung disease, caused by lack of ganglion cells in the submucosal and muscularis mucosa layers of the bowel, presents within the first 24 hours of life.
- Pyloric stenosis usually manifests within weeks to months after birth with projectile vomiting and a palpable mass similar to an olive in shape.
- Appendicitis in a young child manifests with persistent symptoms and is not associated with intestinal obstruction gastrointestinal bleeding.
A 57-year-old man comes to the physician because of a 2-week history of decreased libido. He was recently started on a medication for gastroesophageal reflux disease. He reports that he has been taking higher than the prescribed doses of this medication for persistent symptoms of heartburn.
The drug most likely prescribed for this patient’s reflux also puts him at increased risk for which of the following additional adverse effects?
A. Constipation
B. Gynecomastia
C. Interstitial Nephritis
D. Involuntary Movements of the Lips and Tongue
E. QT Prolongation
B. Gynecomastia
- Cimetidine toxicity can result in antiandrogen effects because of strong inhibition of the cytochrome P-450 system, leading to symptoms of gynecomastia and decreased libido.
The other options are incorrect:
- Constipation may be seen in patients who are taking aluminum hydroxide as an antacid for heartburn.
- QT prolongation may be seen in patients who are taking metoclopramide, a second-line medication for heartburn.
- Involuntary movements of the lips and tongue, tardive dyskinesia, may be caused by prolonged used of the D2-receptor antagonist metoclopramide, a second-line medication for heartburn.
- Interstitial nephritis may be seen with proton pump inhibitors (eg, omeprazole), leading to reduced glomerular filtration rate.
A 56-year-old man presents to his physician with vague abdominal discomfort and fatigue. He has a history of hepatitis C. Physical examination reveals a tender liver, palpable to 6 cm below the costal margin, and scleral icterus. CT scan of the abdomen is shown. Laboratory studies show:
Aspartate aminotransferase: 200 U/L
Alanine aminotransferase: 450 U/L
Total serum bilirubin: 2.8 mg/dL
Direct bilirubin: 2.2 mg/dL
Serum alkaline phosphatase: 405 U/L
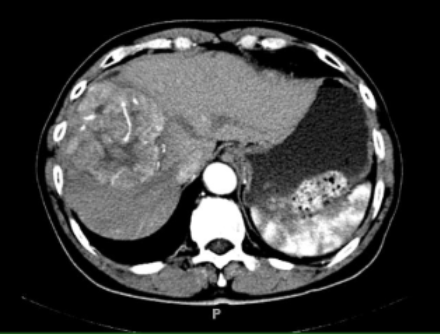
The tumor marker most likely to be increased in this patient is also likely to be elevated in which of the following malignancies?
A. Breast cancer
B. Choriocarcinoma
C. Colorectal adenocarcinoma
D. Neuroblastoma
E. Prostate carcinoma
F. Yolk sac carcinoma
F. Yolk sac carcinoma
- Hepatocellular carcinoma is common in patients with chronic liver disease.
- α-Fetoprotein is a marker for hepatocellular carcinoma.
- α-Fetoprotein is also elevated in patients with germ cell tumors, such as yolk sac carcinoma.
Alfa-fetoprotein levels can also be elevated in patients with germ cell tumors, such as yolk sac tumors. Yolk sac tumors (also known as endodermal sinus tumors) arise from the germ cells that eventually become the adult gonads. Yolk sac tumors are the most common malignant testicular tumors in children.
The other choices are incorrect:
- Choriocarcinoma is evaluated with the tumor marker β-human chorionic gonadotropin.
- Colorectal adenocarcinoma is evaluated with the nonspecific tumor marker carcinoembryonic antigen.
- Breast cancer is evaluated with the tumor marker CA-15-3.
- Neuroblastoma is evaluated with the tumor marker bombesin.
- Prostate carcinoma is evaluated with the tumor marker prostate-specific antigen.
A 50-year-old woman comes to the clinic because of burning epigastric pain for the past 2 months. The pain is relieved with meals. She denies nausea and vomiting. A gastric acid secretion test reveals a stomach pH of 1.1 (normal: 1.5 to 3.5).
Secretion of which of the following substances can counteract the hyperacidity noted in this patient?
A. Acetylcholine
B. Gastrin
C. Intrinsic Factor
D. Nitric oxide
E. Secretin
F. Pepsin
E. Secretin
- Gastric ulcers may present with abdominal pain that worsens with meals, but when patients report their abdominal pain is improved with meals, it points to a duodenal ulcer; the majority (90%) of cases are secondary to H pylori.
- Most patients with peptic ulcer disease have excess gastric acid secretion.
- Increased acid levels in the stomach are ameliorated by secretin, which, along with increasing pancreatic and biliary bicarbonate secretion, inhibits the effects of gastrin on acid production and the growth of the gastric mucosa via increasing somatostatin and prostaglandin E2.
The other choices are incorrect:
- Intrinsic factor is produced in the parietal cells of the stomach and is required for vitamin B12 absorption in the ileum; it has no effect on stomach pH.
- Nitric oxide causes relaxation of the lower esophageal sphincter and has no effect on gastric pH.
- Acetylcholine increases gastric acid secretion, pancreatic enzyme and bicarbonate secretion, and saliva production.
- Gastrin is released by G cells in the antrum of the stomach. It stimulates the secretion of gastric acid, causes growth of the gastric mucosa, and increases gastric motility.
- Pepsin is produced by the chief cells of the stomach and is involved in protein digestion. It is released in response to low gastric pH, but pepsin is an enzyme and, by itself, has no effect on stomach pH.
How old am I?
25 (I think)
An otherwise healthy 20-year-old man comes to the emergency department because of severe lower abdominal pain. The pain began in the periumbilical region and has migrated to the right lower quadrant over the past 12 hours. He reports nausea; one episode of nonbilious, nonbloody vomiting; loss of appetite; and a mild fever. Temperature is 38.3°C (100.9°F), pulse is 90/min, and blood pressure is 135/85 mm Hg. On examination, the patient is in acute distress. His abdomen is not distended but is severely tender in the right lower quadrant with rebound tenderness and involuntary guarding.
Which of the following is the most common underlying pathophysiology behind this patient’s disease?
A. Cystic Duct Obstruction
B. Helicobacter pylori infection
C. Obstruction of the luminal gastrointestinal tract
D. Postoperative adhesions
E. Stress Ulcer
C. Obstruction of the luminal gastrointestinal tract
- Abdominal pain starting in the mid-abdomen and migrating to the right lower quadrant suggests a diagnosis of acute appendicitis.
- In acute appendicitis, the appendiceal lumen is obstructed, most commonly by a fecalith, leading to a bacterial infection of the appendix, leading to inflammation and irritation of the visceral peritoneum.
The other choices are incorrect:
- Cystic duct obstruction by gallstones causes acute cholecystitis, typically presenting as severe right upper quadrant pain preceded by eating fatty food.
- Helicobacter pylori infection causes peptic ulcer disease, which can present as epigastric pain or gastrointestinal bleeding. The same is true for a stress ulcer, which is another underlying cause of peptic ulcer.
- Postoperative adhesions are the leading cause of small bowel obstruction, which presents with diffuse abdominal pain and distension, obstipation/constipation, nausea, and emesis.
A 69-year-old male with a history of colorectal carcinoma reports severe episodes of nausea and vomiting shortly after receiving chemotherapy. The vital signs are stable. Physical examination shows a cachectic man with temporal wasting. Cardiopulmonary examination is unremarkable. He is prescribed a medication for vomiting that may prolong the QT interval on ECG.
Which of the following mechanisms corresponds to the most likely prescribed medication?
A. Acetylcholine receptor antagonist
B. Dopamine receptor antagonists
C. Histamine receptor antagonists
D. Norepinephrine reuptake inhibitor
E. Serotonin receptor antagonist
E. Serotonin receptor antagonist
- Ondansetron is among the strongest antiemetics available and is used as first-line therapy for chemotherapy-induced nausea and vomiting; the ECG must be monitored during use because ondansetron may prolong the QT interval.
- Ondansetron acts by blocking serotonin 5-HT3 receptors.
The other choices are incorrect.
The following choice is not used to treat nausea or vomiting:
- Tricyclic antidepressants are norepinephrine reuptake inhibitors that are primarily used to treat depression and sometimes functional disorders like irritable bowel syndrome.
The following choices are used to treat nausea but would not be first-line treatment for this patient:
- Acetylcholine receptor antagonists may be used to treat motion sickness.
- Dopamine receptor antagonists can be used as antiemetics.
- Histamine receptor antagonists are used in the postoperative period for nausea and vestibular/labyrinthine disorders.
A 40-year-old male comes to the office because of daily diarrhea over the past 5 months. During this time, his stools have smelled worse than they used to and appear oily. He has lost 9 kg (20 lb) over the past 5 months despite having a good appetite. He is in recovery from alcohol use disorder and has had multiple bouts of acute pancreatitis in the past.
Which of the following initial tests would help direct investigation toward the most likely cause of this patient’s weight loss?
A. Anti-tissue transglutaminase IgA assay
B. Colonoscopy
C. Serum Lipase
D. Stool ova and parasite tests
E. Sudan III staining
E. Sudan III staining
- In a patient with a history of alcohol use disorder and recurrent pancreatitis, exocrine pancreatic insufficiency is the most likely cause of steatorrhea resulting from fat malabsorption.
- The most sensitive screening test for evaluating steatorrhea is a qualitative Sudan III staining assay.
The other choices are incorrect.
The following choices may be helpful for pancreatic disease but not malabsorption:
- Serum lipase is used to diagnose acute pancreatitis, not chronic pancreatitis, which is this patient’s current presentation.
The other choices could diagnose gastrointestinal issues with different clinical scenarios:
- A colonoscopy helps diagnose structural colonic issues, such as bleeding.
- Celiac disease can cause steatorrhea and is worked up with by an antitissue transglutaminase IgA assay.
- Stool ova and parasite tests can be used to assess for parasites. Some parasites, like Giardia and Cryptosporidium, may present with foul-smelling stool.
A 44-year-old man presents to the emergency department immediately after an episode of hematemesis. Medical history includes cirrhosis secondary to hepatitis C. Physical examination shows scleral icterus and spider angiomas. His abdomen is distended with shifting dullness to percussion. Rectal examination reveals maroon stool.
Which of the following vessels from the portal circulation contributed most directly to this patient’s bleeding?
A. Hemiazygos vein
B. Inferior Vena Cava
C. Left Gastric Vein
D. Right Gastric Vein
C. Left Gastric Vein
- In a patient with cirrhosis, upper GI bleeding is often caused by ruptured esophageal or gastric varices.
- The left gastric vein is the portal branch most directly involved in the formation of esophageal and gastric varices.
The other choices are incorrect:
- The hemiazygos vein is a systemic vein in the thorax.
- The superficial epigastric veins are systematic veins that can contribute to caput medusae.
- The inferior vena cava is not involved in portal-systemic collaterals.
- The left gastro-omental (gastroepiploic) vein runs parallel to the greater curvature of the stomach.
- The right gastric vein runs along the lesser curvature of the stomach and anastomoses with the left gastric vein.
What is the name of the county I am from?
Beford county (yee yee)
A 34-year-old man comes to the physician because of itchiness and fatigue for 3 months. Medical history is significant for chronic bloody diarrhea, which the patient has been experiencing intermittently for the past 3 years. He also has a history of knee joint pain for the past 1 year. Physical examination reveals scleral icterus, excoriations, and hepatomegaly. Cholangiography shows obliteration of the intrahepatic and extrahepatic bile ducts. Laboratory studies show an ALT value of 130 U/L, AST of 120 U/L, and alkaline phosphatase of 400 U/L.
Which of the following is a risk factor for this patient’s most likely diagnosis?
A. Hepatitis C Infection
B. Primary Biliary Cholangitis
C. Systemic Lupus Erythematosus
D. Ulcerative Colitis
E. Wilson Disease
D. Ulcerative Colitis
- PSC causes periportal fibrosis and stenosis of hepatic bile ducts.
- PSC is associated with UC, and 70% of patients with PSC have UC.
A 67-year-old woman comes to the clinic because of fatigue and weight loss. She is ultimately diagnosed with colon cancer with liver metastasis. Treatment options are discussed, including infusion of a monoclonal antibody. The monoclonal antibody is directed against a cellular factor that is also involved in wet age-related macular degeneration.
Which of the following peptides is most likely targeted by the monoclonal antibody under consideration?
A. Epidermal growth factor
B. Interleukin-1
C. Interleukin-6
D. Tumor necrosis factor-α
E. Vascular endothelial growth factor
E. Vascular endothelial growth factor
- Bevacizumab is a monoclonal antibody that inhibits VEGF. It is used in the treatment of colon cancer and wet AMD.
- VEGF is a cellular factor that promotes blood vessel proliferation and expansion, and overexpression of VEGF enables tumor growth.
The other choices are incorrect:
- Epidermal growth factor is involved in oncogenesis and metastasis, but not wet AMD.
- Interleukin-1 (IL-1), IL-6, and tumor necrosis factor-α are inflammatory markers that are not current targets of AMD treatment.
A 50-year-old male comes to the physician for his annual visit. The patient is asymptomatic and has an unremarkable medical history. The patient has no known family history of colorectal cancer. Routine colonoscopy reveals a pedunculated polyp. The histologic appearance of the polyp is shown.
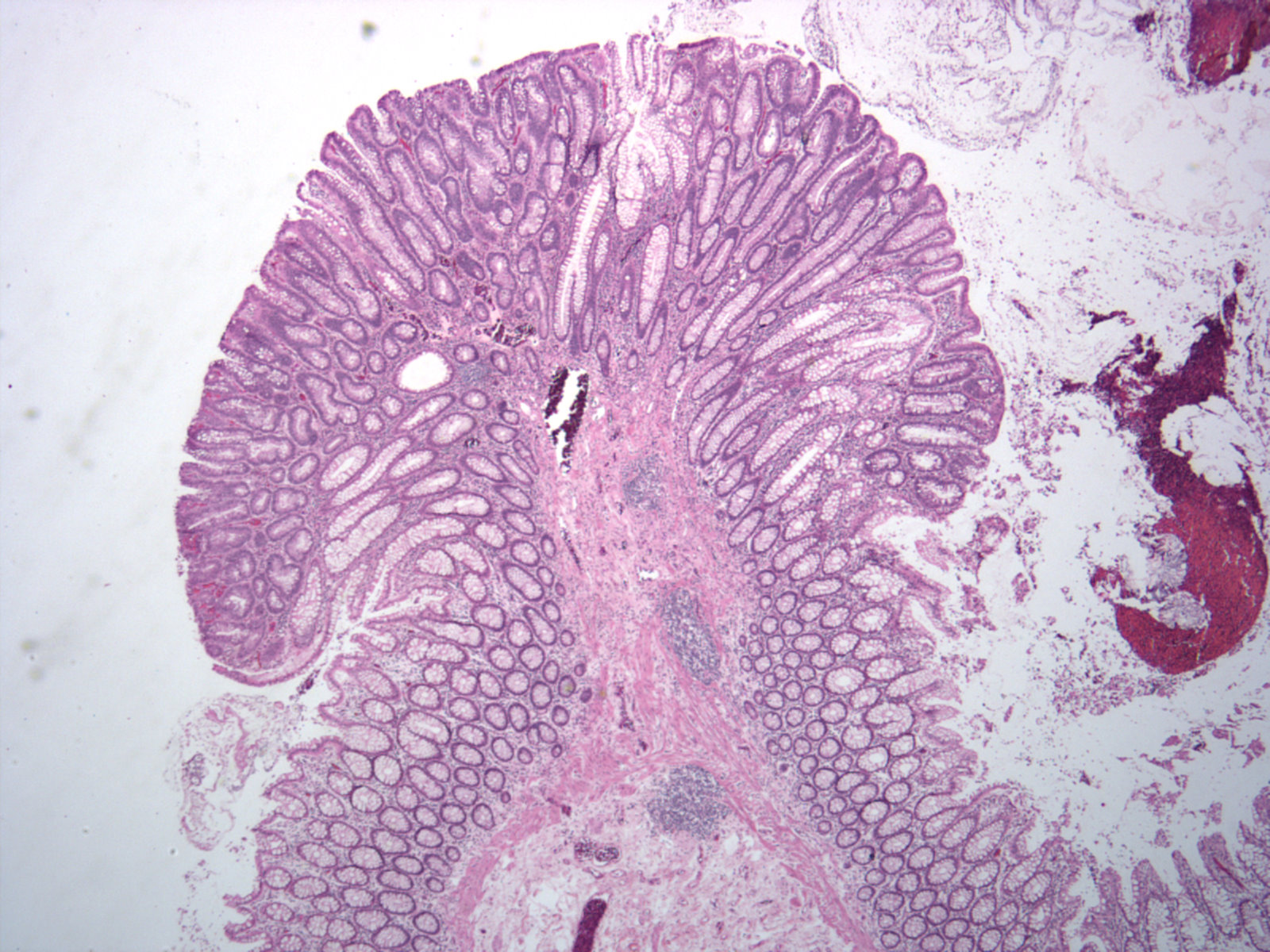
Which of the following is the most likely diagnosis?
A. Hamartomatous polyp
B. Hyperplastic polyp
C. Sessile serrated polyp
D. Tubular adenoma
E. Villous adenoma
D. Tubular adenoma
- Histologic examination shows that tubular adenomas consist of mostly adenomatous epithelium arranged in glandlike structures.
The other choices are incorrect:
- Hyperplastic polyps are histologically serrated but otherwise have normal architecture. The serrations are typically restricted to the upper one-third or less of the crypt. There is no associated risk for malignancy.
- Sessile serrated polyps have a serrated appearance throughout the full length of the gland on histologic examination and have malignant potential.
- Hamartomatous polyps consist of normal colonic tissue with distorted architecture.
- Villous adenomas are generally broad based and sessile (without a stalk) lesions with a higher degree of dysplastic changes.
A 22-year-old woman comes to the clinic because of increasing shortness of breath, weakness, and fatigue. She has a history of heavy menstrual bleeding. Physical examination reveals hair loss, koilonychia, and pale mucous membranes. Laboratory studies show a hemoglobin concentration of 6 g/dL, a mean corpuscular hemoglobin concentration of 24 Hb/cell, a mean corpuscular volume of 65 fL, and an RBC distribution width of 17%.
What part of the gastrointestinal tract is responsible for absorbing the nutrient in which this patient is most likely deficient?
A. Duodenum
B. Gastric body
C. Gastric fundus
D. Ileum
E. Jejunum
A. Duodenum
- Iron-deficiency anemia is characterized by shortness of breath, weakness, fatigue, pale mucous membranes, low mean corpuscular volume, and high RBC distribution due to reduced oxygen delivery to the body.
- Iron is predominantly absorbed in the duodenum, and damage to the duodenal enterocytes can lead to malabsorption of iron and iron-deficiency anemia.
The other choices are incorrect:
- The gastric fundus contains parietal cells that secrete hydrochloric acid and intrinsic factor, both of which are required for the absorption of vitamin B12.
- The ileum is the major site of absorption of vitamin B12 and contributes significantly to the absorption of fat-soluble vitamins, fatty acids, proteins, and carbohydrates.
- The jejunum is a major site of folate absorption and contributes significantly to the absorption of fat-soluble vitamins, fatty acids, proteins, and carbohydrates. Decreased folate absorption causes macrocytic anemia.
- The gastric body is the main part of the stomach and is located below the gastric fundus. The gastric body has parietal cells that secrete hydrochloric acid and intrinsic factor, both of which are required for the absorption of vitamin B12. A deficiency in intrinsic factor will lead to malabsorption of vitamin B12, causing macrocytic anemia.
Psyche! It's a question:
A 27-year-old male presents to his primary care physician for evaluation of abdominal pain and intermittent, nonbloody diarrhea. The patient has had similar episodes over the past 4 years. He has also been experiencing fatigue and had a 4.5-kg (10-lb) weight loss over the past few months. His temperature is 38.2°C (100.8°F), pulse is 82/min, respirations are 18/min, and blood pressure is 126/84 mm Hg. On physical examination, the patient appears ill and has aphthous ulcers in the mouth. Abdominal examination reveals moderate right-lower-quadrant tenderness to palpation. Rectal examination reveals no abnormalities. A colonoscopy is ordered.
Which of the following findings would most likely be associated with this patient’s presentation?
A. Mucosal and submucosal inflammation
B. Mucosal polyps
C. Normal mucosa
D. Saccular outpouchings
E. Transmural inflammation
E. Transmural inflammation
- Crohn disease is a type of inflammatory bowel disease and most commonly presents with abdominal pain, fever, weight loss, diarrhea (bloody or nonbloody), fistulas, abscesses, and malabsorption.
- Crohn disease is characterized by transmural inflammation of the bowel wall and cobblestone mucosa, with skip lesions occurring anywhere along the digestive tract.
Crohn disease is characterized by transmural inflammation of the bowel wall and cobblestone mucosa, with skip lesions occurring anywhere along the digestive tract. Creeping fat, bowel wall thickening, and noncaseating granulomas (T-helper type 1 cell mediated) are also seen in this disease.The other choices are incorrect:
Some of the other findings could present with chronic diarrhea:
- Mucosal and submucosal inflammation describes ulcerative colitis, a form of inflammatory bowel disease that presents with bloody diarrhea.
- Irritable bowel syndrome presents with recurrent abdominal pain and altered habits (constipation, diarrhea, or both). Colonoscopy would show normal mucosa.
The other findings have varied clinical presentations:
- Diverticulosis involves saccular outpouchings of the colon, commonly seen in people older than 60 years. The condition is asymptomatic unless infection (diverticulitis) or diverticular bleeding develops.
- Mucosal polyps are common precancerous lesions of the colon. They would not be symptomatic unless they were very large and led to bleeding.