at the base of the falciform ligament, these structure drain into the IVC.
hepatic veins
this is the percentage of people with some variation in hepatic arterial anatomy
40-45%
these are the constituents of the MELD-Na score.
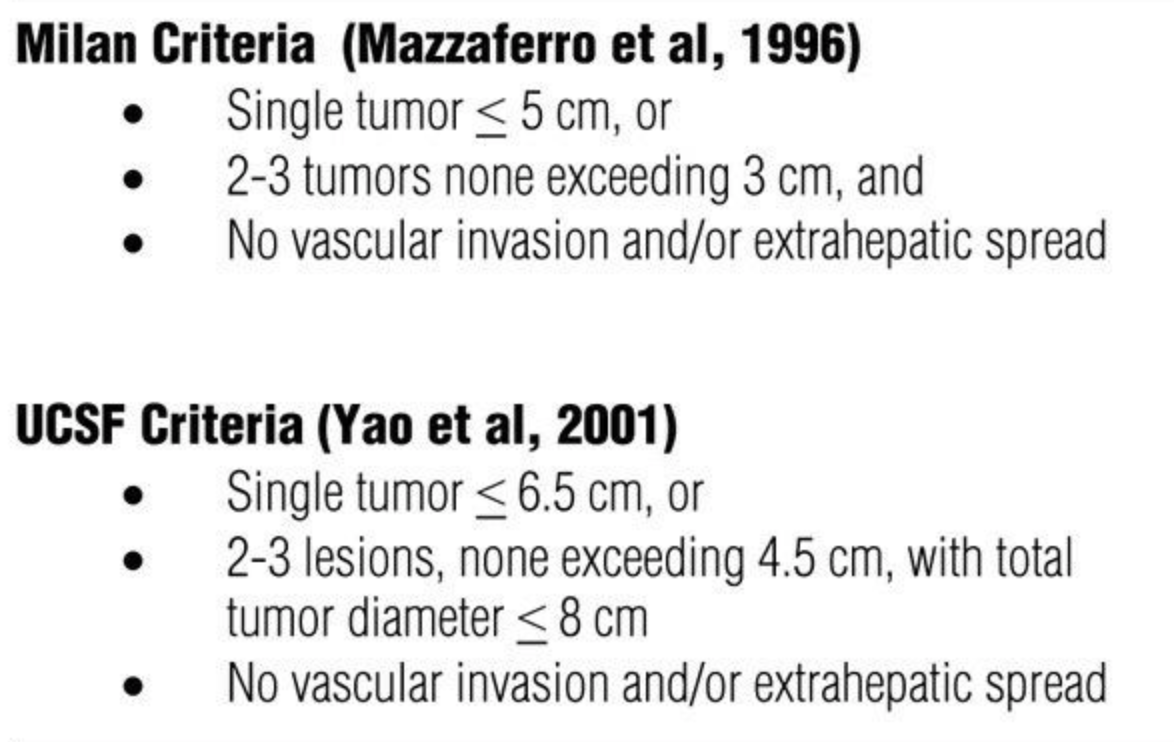
inr, creatinine, bilirubin, Na. bonus. score with Hepatocellular carcinoma (HCC) with one lesion between 2 - 5 cm or two to three lesions <3 cm (Milan criteria), provided no vascular invasion or extrahepatic disease.
ICC is the 2nd most common primary malignant liver tumor and accounts for this percentage of such cases
10-20%
this is the percentage of patients with CRC that will develop metastatic disease.
~50%
this is the most common liver tumor
hemangioma are congenital vascular malformations, with cavernous vascular spaces, a flat endothelial lining, and fibrous septations. They are usually asymptomatic, incidental findings, but pain and local compressive symptoms may result from the size and particular location of a tumor.
this is the name of the classification system for choledocal cysts.
Todani classification
name the risk factors for cholangio (name 2)
primary sclerosing cholangitis (PSC), Patients with PSC have a lifetime risk of 8 to 20% of developing cholangiocarcinoma, choledochal cysts or Caroli disease has a 3 to 28% lifetime risk, Hepatolithiasis, also known as recurrent pyogenic cholangiohepatitis or Oriental cholangiohepatitis, is prevalent in Asia, thorium, radon, nitrosamines, dioxin, and asbestos
risk factors of gallbladder ca (name 4)
gallstones, gallstone size, porcelain gallbladder, adenomatous polyps of the gallbladder, chronic infection with Salmonella typhi, carcinogen exposure (e.g., miners exposed to radon), and abnormal pancreatico-biliary duct junction (APBDJ). Bonus, size of gb polyp you worry about cancer.
the treatment for distal cholangiocarcinoma is this operation.
Whipple
this is the layer of connective tissue surrounding the liver and ensheathing the hepatic artery, portal vein, and bile ducts within the liver
glisson’s capsule
the ligamentum teres, or round ligament, is a remnant of this obliterated embryologic structure
umbilical vein
Current guidelines recommend __ and ___ testing every 6 to 12 months for patients with cirrhosis of viral or nonviral etiology and HBV carriers without cirrhosis as screening for HCC.
US and AFP
name the risk factors for HCC (4/9)
hepatitis C virus infection, hep b, alcoholism, aflatoxin B1 exposure, a1-antitrypsin deficiency, obesity, hemochromatosis, primary biliary cirrhosis, and nonalcoholic steatohepatitis (NASH)
name 2 RF’s for the development of ICC
primary sclerosing cholangitis (8% to 20% lifetime risk), choledochal cysts (3% to 28% lifetime risk), cirrhosis, alcohol abuse, diabetes, obesity, chronic calculi, and liver fluke infections
the principles determining resectability include the following (2/3)
(1) complete anatomic resection must be possible while maintaining adequate hepatic function, (2) the primary tumor must be amenable to R0 resection, and this. (3) there should be no unresectable extrahepatic disease.
in hepatic adenomas, all lesions greater than this size should be resected
4cm. The risk of symptoms increases with increasing size, particularly greater than 5 cm, with as high as a 20 to 40% risk of spontaneous bleeding. Malignant transformation occurs in approximately 10% of cases.
simple hepatic cysts are typically treated with aspiration and injection of 1 of these 2 agents.
Ethanol or minocycline
Most hilar cholangiocarcinomas, also known as upper duct cholangiocarcinomas, arise just below the union of the right and left hepatic ducts, at the union of the ducts, or in the main right or left hepatic duct. They are also known as ____.
klatskin tumors
this occurs in about 50% of patients and is a poor prognostic sign because it signifies extension of the tumor beyond the gallbladder and obstruction of the extrahepatic ducts
jaundice
patients who are found to have unresectable distal cholangiocarcinoma at operation should undergo this...
choledocho- or hepaticojejunostomy
the gastrohepatic ligament, or lesser omentum, which is an attachment of connective tissue between the lesser curvature of the stomach and the left hepatic lobe, carries important neural and vascular structures, including the hepatic division of the vagus nerve and, when present, this aberrant structure.
left hepatic artery; bonus from what?; bonus bonus, percentage of patients?
an aberrant right hepatic artery comes from this structure
SMA; bonus, percentage?; bonus bonus, most common location and risk of injury?
these are the 4 phases of a four-phase study (CT or MRI)
unenhanced, arterial, venous, and delayed phases. HCCs are hypervascular lesions whose blood supply is primarily from the hepatic artery; therefore, on multidetector computed tomographic (CT) imaging, the lesion typically appears hyperintense during the arterial phase and hypodense (referred to as “washout”) during the delayed phases
these are the constituents of the milan criteria
the only potential curative option for ICC
partial hepatectomy with negative margins
small lesions which disappear with chemotherapy should still be resected because these lesions will recur in nearly this percentage of pts.
~80%
this is the malignant potential of FNH
nil. Should be managed non-operatively. There is no malignant potential and no risk of rupture, bleeding, or other complications.
Bile duct cysts may be first identified on US or CT for symptoms mimicking cholecystitis. However, for precise anatomic information to guide treatment planning, (name 3, complete names no acronyms), these are the studies of choice.
Magnetic resonance cholangiopancreatography, Endoscopic retrograde cholangiopancreatography, Percutaneous transhepatic cholangiography
this is the most common presenting symptom of distal cholangiocarcinoma
Painless jaundice, Other manifestations of biliary obstruction, such as acholic stools, dark urine, and pruritis, are also prevalent. Abdominal pain, fatigue, malaise, and weight loss can also occur with advanced disease.
this is the treatment for tis or t1a lesions
cholecystectomy
Current indications for biliary decompression for unresectable patients include (2/4)
symptomatic relief for intractable pruritis, treat cholangitis, gain access for intraluminal radiotherapy, and allow hepatic function recovery in patients receiving chemotherapy
name the structure of the porta hepatis and their respective positions.
portal posterior, hepatic medial, CBD lateral
percentage of blood supply from the portal vein and hepatic artery to the liver, respectively.
70-75 and 25-30
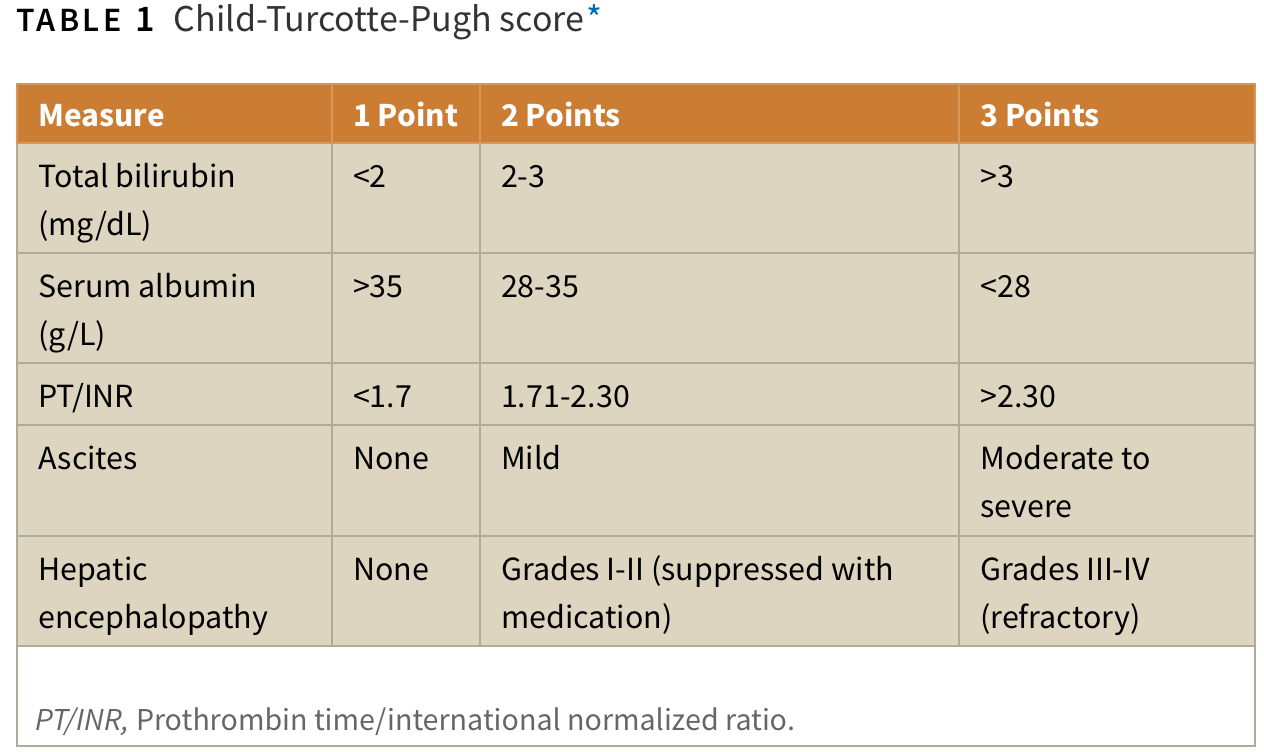
these are the constituents of the child-turcotte-pugh score
this is the minimal recommended volume of the FLR for patients with a healthy liver, mild dysfunction, and cirrhosis, respectively.
20, 30, 40. Volumetry is calculated with three-dimensional CT scan or MRI. The volume of nonfunctional liver (parenchyma that is either nonperfused or replaced by tumor) is subtracted from the total liver volume, which is especially important for patients with large lesions. Alternatively, the estimated total liver volume can be calculated with the patient’s body weight or body surface area (i.e., total liver volume in cm3 = −794.41 + 1267.28 × body surface area in m2). Patients with insufficient FLR volumes should undergo portal vein embolization (PVE) of the branches of the segments planned for resection to induce growth to the contralateral side. Volumetry is repeated about 4 weeks after PVE and in a few more weeks if the minimal recommended FLR has not been achieved. The degree of hypertrophy (hyperplasia) of the remnant (at least a 5% increase in the volume of the FLR or an increase of 2% per week or more) has been associated with decreased rates of postoperative liver insufficiency.
mass forming, periductal infiltrating, and intraductal growing
three macroscopic histologic subtypes
criteria for ablation of CRC
small (<3 cm and ideally <1 cm) lesions that are not near major vessels or bile ducts
Treatment of asymptomatic hemangioma, irrespective of size, is observation, with no need for surveillance imaging. Indications for operation include (3/4)
severe pain, compressive symptoms, hemorrhage, or uncertain diagnosis with a suspicion of malignancy
this is the most commonly accepted hypothesis for the etiology of choledocal cysts.
APBDJ. Anomalous pancreaticobiliary duct junction: the pancreatic duct joins the common bile duct more than 15 mm proximal to the ampulla, resulting in a long common channel and free reflux of pancreatic secretions into the biliary tract. This reflux of pancreatic juice into the biliary tract results in increased biliary pressures and inflammatory changes in the biliary epithelium, causing ectasia and dilatation
this is the most accurate modality for diagnosing cholangiocarcinoma in patients with PSC who present with a dominant biliary stricture.
EUS-fine needle aspiration
In t1b and t2 ca, the gallbladder is resected en bloc with a minimum of a 2 cm hepatic parenchyma margin, and lymphadenectomy is performed. Lymphadenectomy consists of dissection of these lymph node beds (3/4)
The porta hepatis, gastroduodenal ligament, and gastrohepatic ligament and a Kocher maneuver with removal of the lymph nodes along the posterior duodenum and behind the pancreatic head
the patient related contraindications for resection include (2/3)
major cardiopulmonary disease, cirrhosis, and metastatic disease. A reasonable strategy is to proceed to operation if (1) the patient is relatively young (< 70 years), (2) there are no serious comorbid conditions, (3) the jaundice had been present for less than 4 weeks, (4) the serum bilirubin concentration is lower than 10 mg/dL, and (5) the future remnant liver will include more than 35% of the total liver mass.
the portal vein is formed as a confluence of these 2 structures
splenic and SMV; bonus, where?
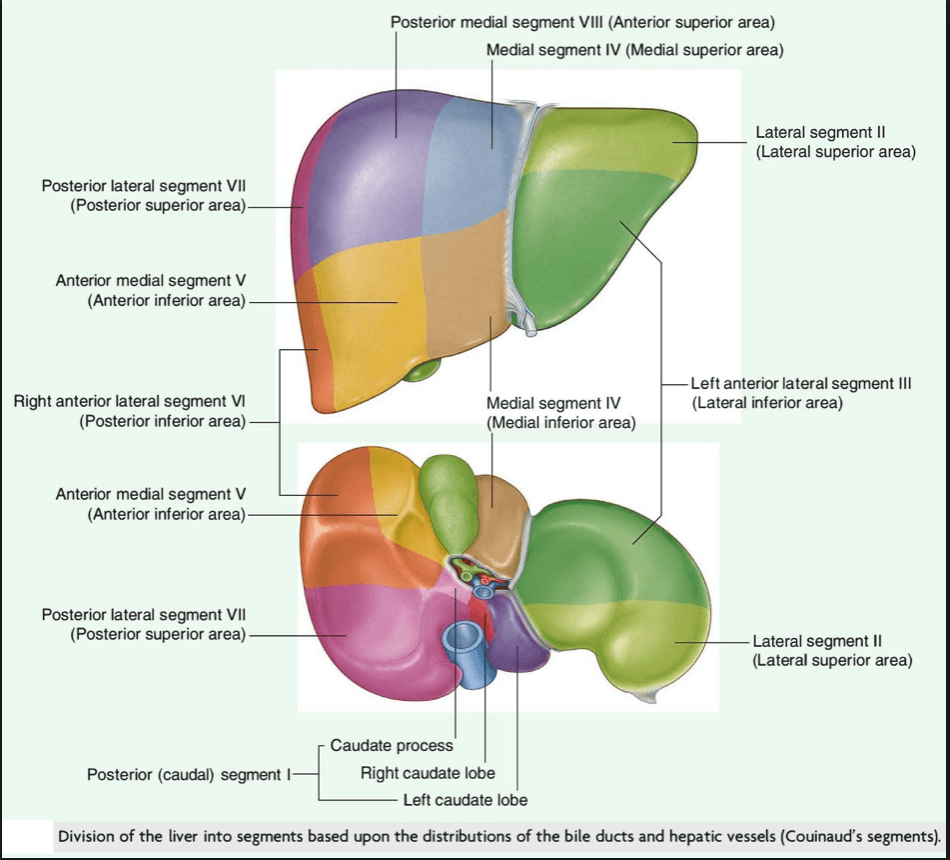
draw all couinaud segments, number and name them.
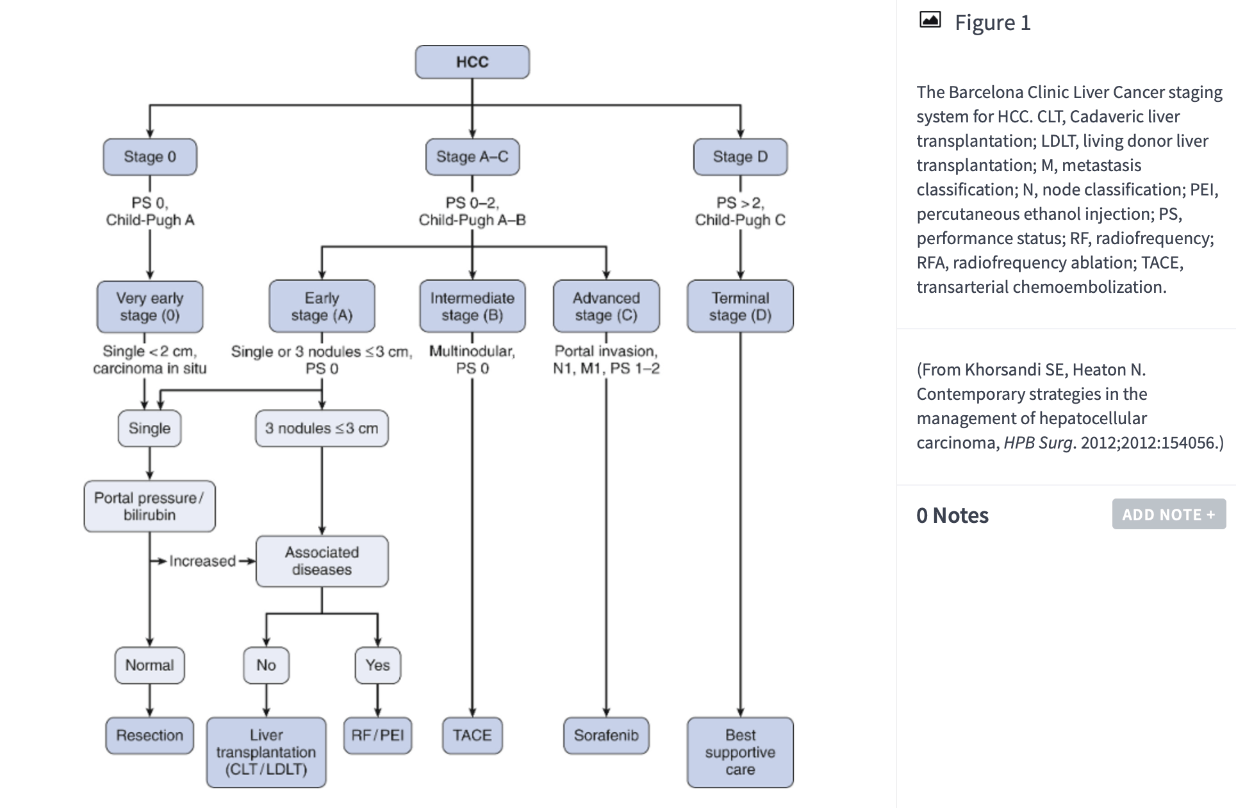
This is the 5-year survival for early stage disease, 3-year survival for intermediate stage disease, and advanced disease.
50 to 75% with treatment, up to 50% without treatment, and only 50% of patients surviving 1 year.
What are the stages of the barcelona clinic liver cancer staging system
Metastatic disease to these lymph nodes is considered a contraindication to resection (name both)
celiac or retroperitoneal
This is the phenomenon where RFA is not effective due to a tumor being very close to a large blood vessel allowing tumor cells on the vessel wall to remain very close to physiologic temperatures.
“heat-sink” effect.
Metal electrodes (probes) are placed into the tumor and dispersive grounding pads placed on the patient. A generator creates high-frequency alternating currents of 350 to 500 kHz, which creates friction from ionic agitation within the current, primarily adjacent to the probe. Charring is undesirable because it creates high electrical impedance and impedes current flow. This is critical because incomplete tumor ablation is the primary cause of local tumor recurrence. Studies have demonstrated significantly higher local recurrence rates when RFA is performed on tumors at least 3.5 cm in size. In addition, RFA is less effective when a tumor is very close to a large blood vessel because the continuous blood flow in the vessels keeps the tumor cells on the vessel wall very close to physiologic temperatures. This phenomenon is known as the “heat-sink” effect, the dissipation of thermal energy by blood flow.
MWA uses dielectric hysteresis to generate microwaves with frequencies ranging from 900 to 2500 mHz to cause coagulative necrosis. In contrast to RFA, microwave antennas are used as probes, which cause active heating of all tissues within their broadcasting range, thereby inducing a more homogenous zone of thermal destruction. When compared with RFA, experimental studies in mouse models have demonstrated that MWA is associated with a more rapid rise in temperature and larger ablation zone. In addition to producing less charring, MWA is better able to penetrate through biologic materials with low conductivity (i.e., charred tissue) and is nearly 25% less susceptible to the “heat-sink” effect because it does not rely as much on heating by thermal conduction.
The International Working Group on Image-Guided Tumor Ablation recommends a baseline study (CT or MRI) to be performed within 1 week and no more than 4 weeks postablation. NCCN guidelines are similar and recommend imaging every 3 to 6 months for the first 2 years after ablation, which then can be spread out to annually thereafter
Hemangioma, FNH, Adenoma. Describe the CT findings for each.
hemangioma: hypodense lesion in the precontrast phase; nodular, peripheral enhancement followed by central enhancement in the arterial phase; and persistent contrast enhancement on delayed series
FNH: hypodense lesion in the precontrast phase, rapid arterial enhancement, often with a less dense central scar, and an isodense or hyperdense lesion in the portal venous phase
Adenoma: hypodense mass, which enhances heterogeneously in the arterial phase and washes out to an isodense or hypodense appearance in the portal venous phase.
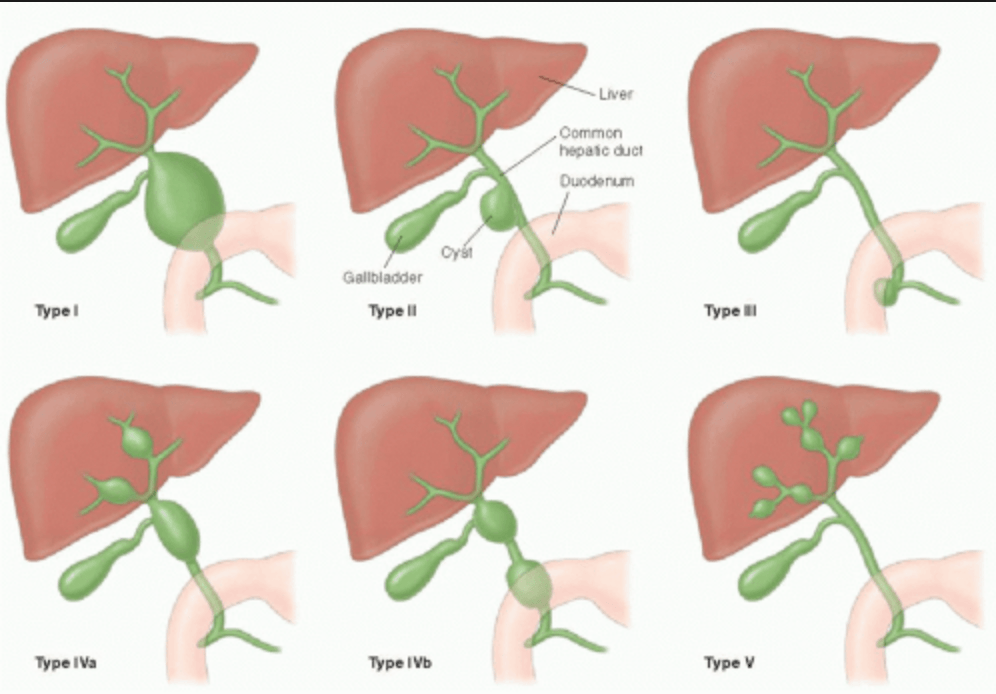
describe the 5 types of choledocal cysts
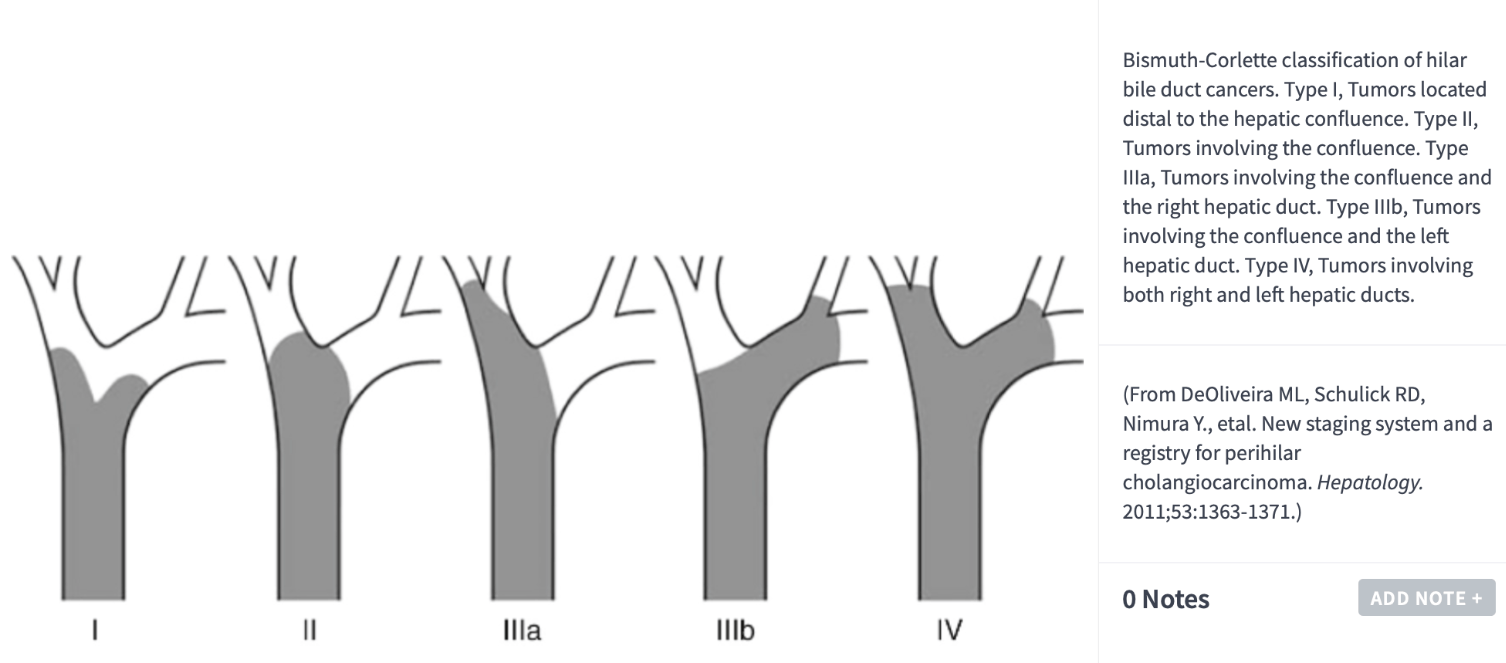
describe the types of peri-hilar cholangiocarcinoma according to the Bismuth-Corlette classification
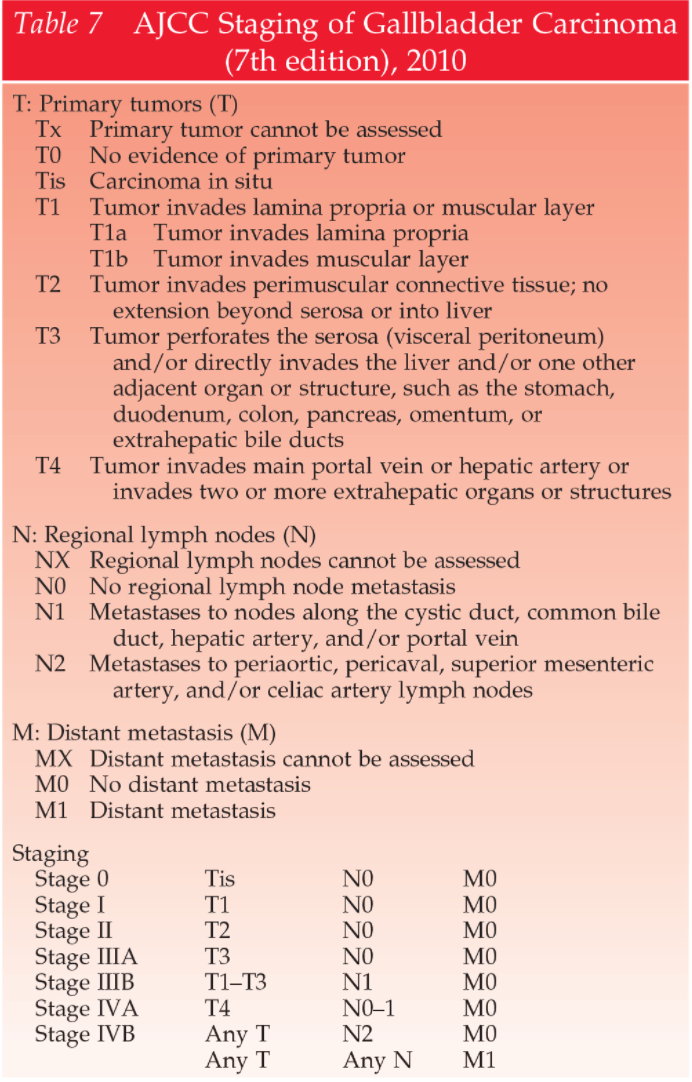
t staging for GB CA
the tumor related contraindications for resection include (2/3)
encasement or occlusion of the main portal vein or hepatic artery either bilaterally or proximal to the bifurcation, involvement of the bilateral secondary ducts or unilateral ducts with contralateral vascular compromise, and hepatic lobe atrophy with contralateral secondary duct or portal vein involvement
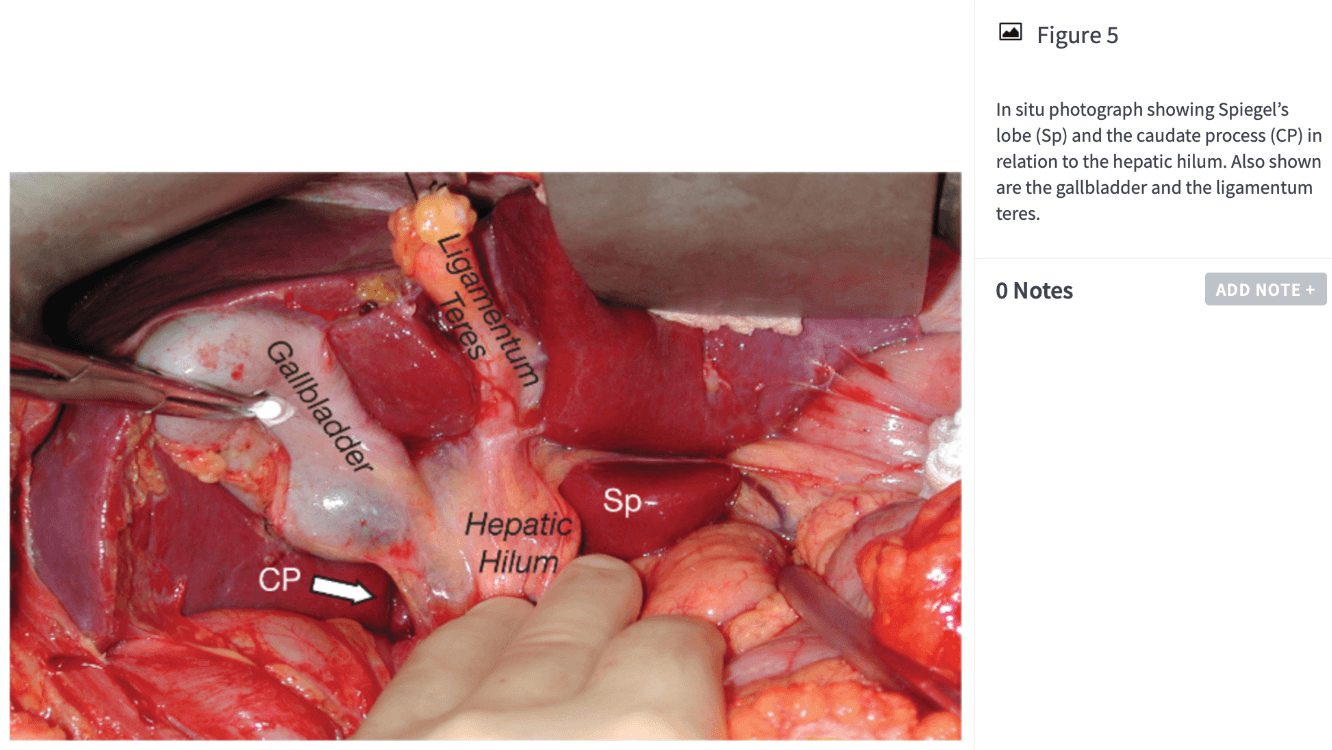
anatomically, the caudate lobe has 3 portions, name them. surgically it has 2 portions.
bonus, this structure decides the left and right hemiliver.