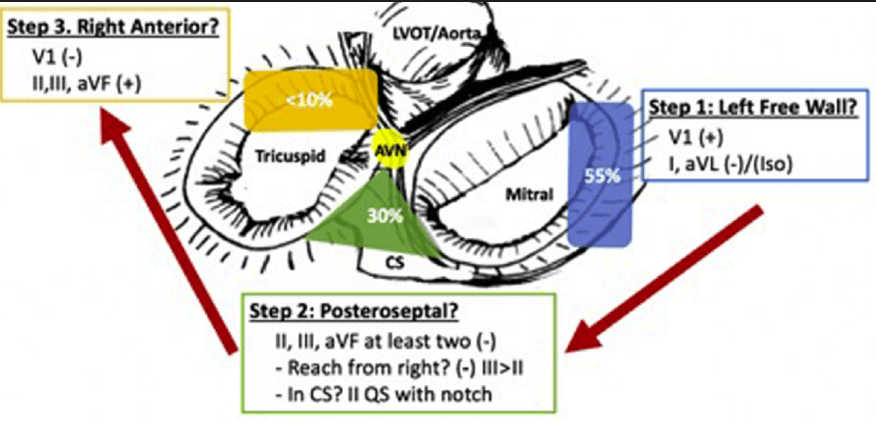
This eponymous algorithm is commonly used to localize accessory pathways.
What is the Arruda algorithm?
This complication can be identified by a bruit noted on femoral auscultation.
What is an AV fistula?
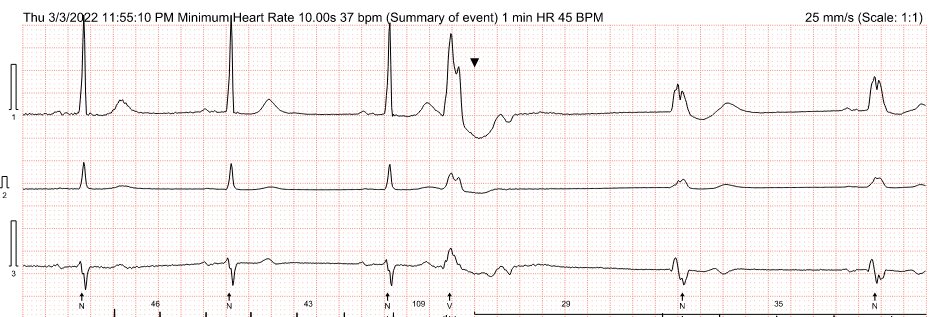
This type of device can be used to evaluate syncope occurring a few times per year.
What is an ILR (Implantable Loop Recorded)?
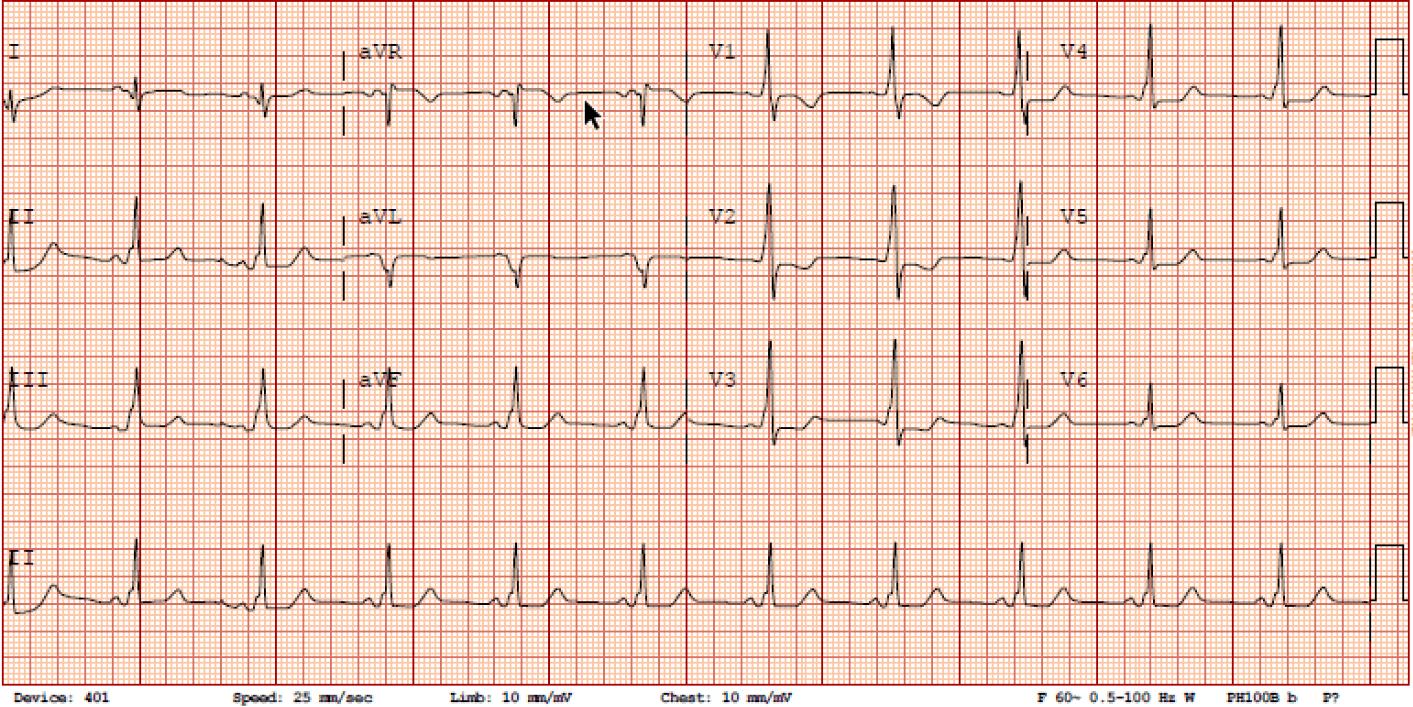
Evidence of this arrhythmic condition is seen on this ECG.
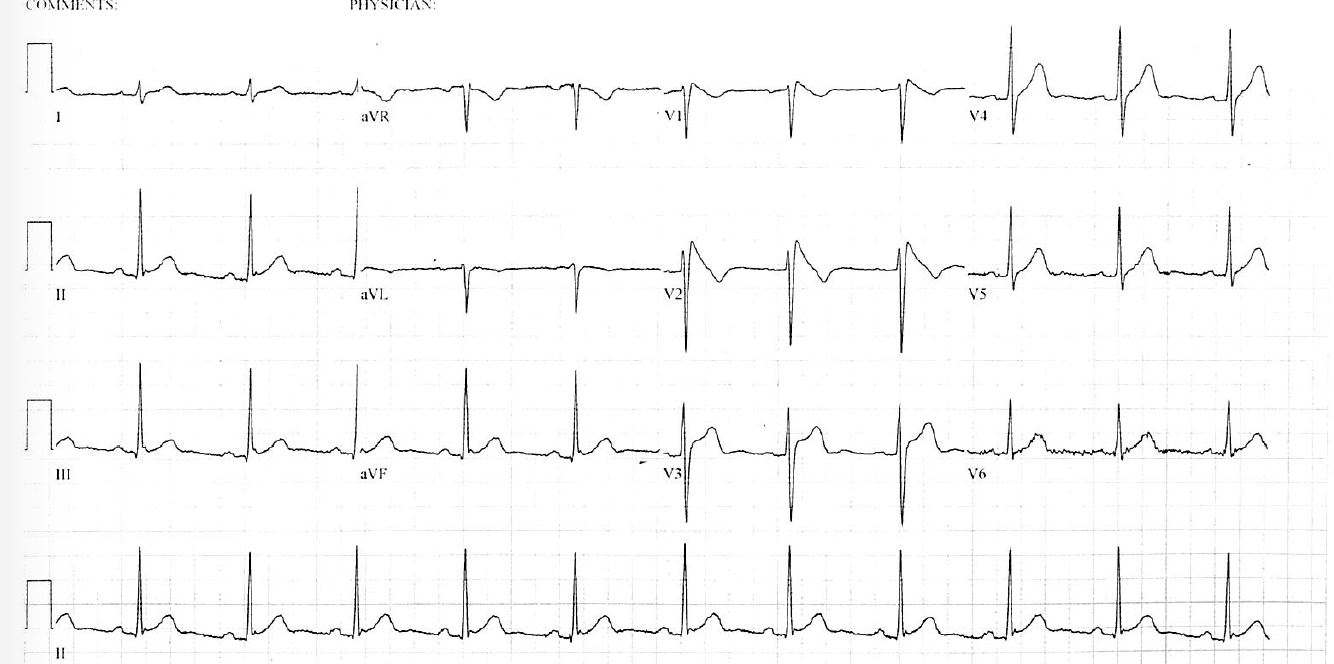
What is Brugada Syndrome?
This congenital condition is known to be associated with multiple accessory pathways.
What is Ebstein anomaly?
This term describes accessory pathways which only conduct retrograde.
What is a concealed accessory pathway?
This 'pressing issue' might develop after sheaths are removed following a left atrial procedure.
What is cardiac tamponade?
This type of device would be considered in a patient with poor bilateral subclavian vascular access.
What is a Leadless pacemaker?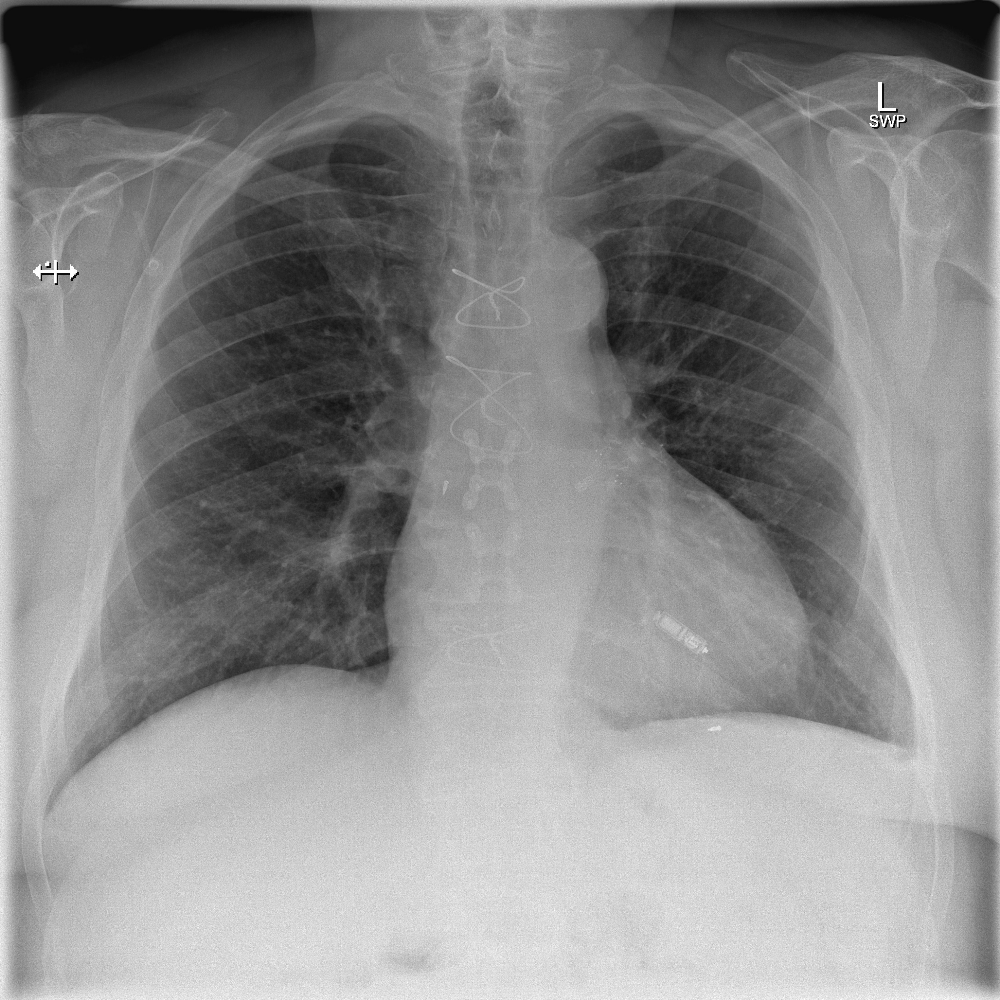
This is the most likely arrhythmia seen here.

What is AVNRT?
First PAC conducts over fast pathway; second PAC conducts over slow pathway.
In addition to prior cardiac arrest and sustained VT, these are 3 (of 5) recommendations for ICD implantation in Hypertrophic Cardiomyopathy patients (from the AHA/ACC/HRS 2020 HCM guidelines).
1) LV wall thickness ≥30mm
2) Any apical aneurysm
3) LVEF ≤50%
4) Recent, likely arrhythmic syncope
5) Family History (sudden death likely due to HCM in 1st degree relative ≤50yo)
Weaker
i) Extensive LGE
ii) NSVT on ambulatory monitoring
This confusing initialism refers to a re-entrant arrhythmia mediated by a retrograde, slowly conducting accessory pathway.
What is PJRT (Permanent Reciprocating Junctional Tachycardia)?
This is the appropriate management for the below patient presenting 1 week post-device implant.

What is conservative? (+/- antibiotics)
Intervention for hematoma should be withheld unless forced (ex erosion, severe pain, infection) as infection risk is high.
Never aspirate a hematoma!
This procedure can be considered for patients with recurrent bleeding and atrial fibrillation with high CHADS score.
What is Left atrial appendage occluder (or left atrial appendage excision)?
This type of block is seen here:
What is Phase IV (pause-dependent) block?
Due to slow depolarization of diseased conduction system tissue resulting in inadequate 'closed' (as opposed to 'inactivated') Na channels to be able to achieve threshold.
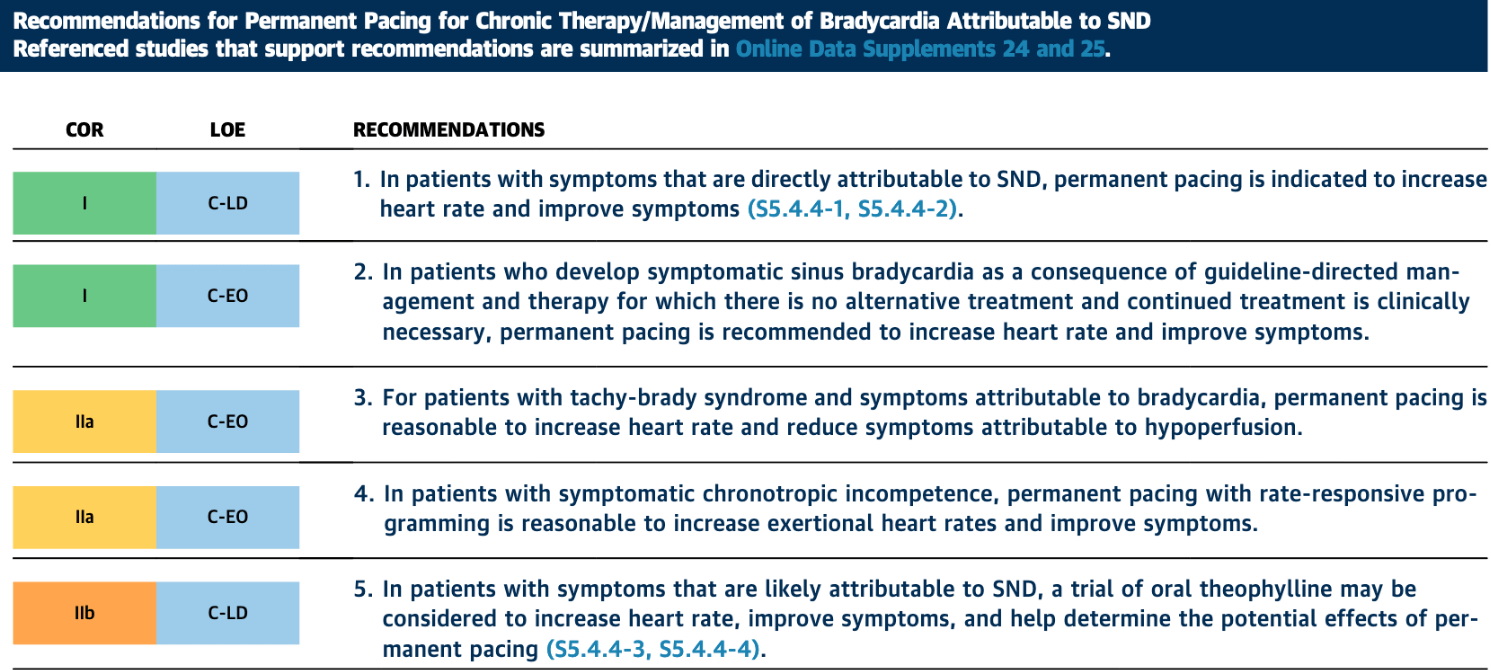
List 3 indications for pacing in sinus node dysfunction from the ACC/AHA/HRS 2018 Bradycardia and Cardiac Conduction Delay guidelines.
What are:
1) Symptoms directly attributable to SND (I)
2) Symptomatic sinus bradycardia due to GDMT (I)
3) Tachy-brady syndrome with brady symptoms (IIa)
4) Symptomatic chronotropic incompetence (IIa)
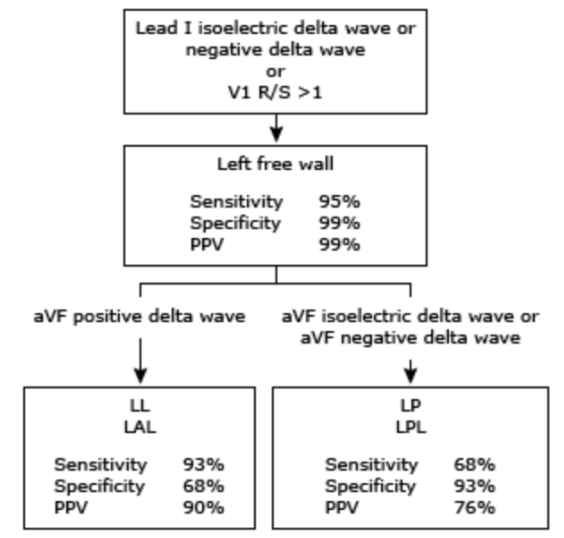
This is the location of the accessory pathway seen below:
What is left lateral?
This complication of atrial fibrillation ablation is a reason not to perform gastroscopy or bronchoscopy in a patient with hematemesis/hemoptysis shortly after the procedure.
What is atrial-esophageal fistula?
Very rare (~1:10k), typical window 5 days-5 weeks, very high mortality if not identified and intervened upon early.
Symptoms: chest pain, fever, malaise, odynophagia, stroke, hematemesis, hemoptysis, melena
Perform CT with IV contrast or MRI if suspicious.
Endoscopy involves air insufflation which can lead to embolism.
This type of pacing could be considered in a pacemaker dependent patient without options for a coronary sinus LV lead.
What is left bundle pacing or His bundle pacing (1/2 points for LV endocardial or epicardial lead)?
This is why the problem seen in the image below occurred.
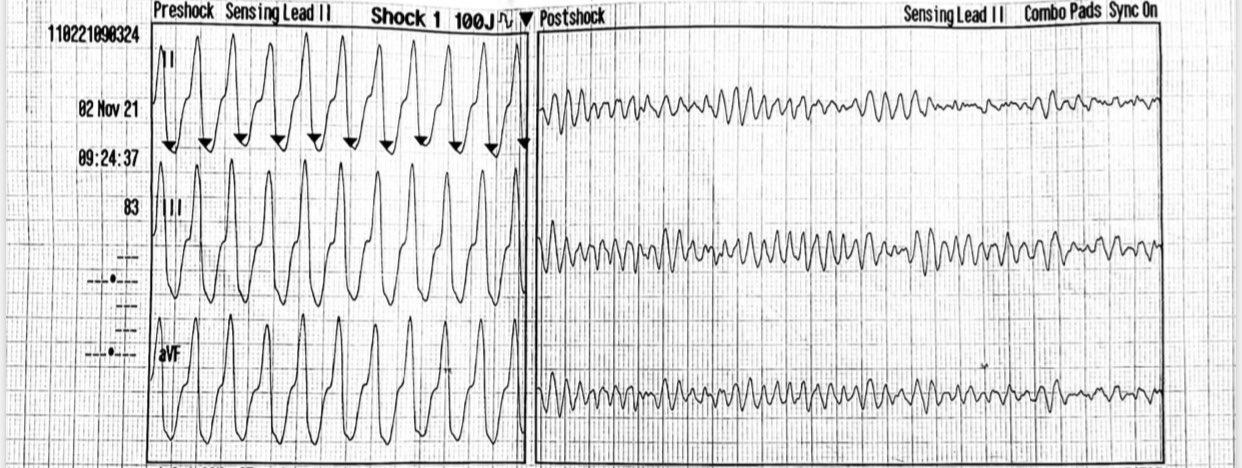
What is defib syncing to T wave?
Antiarrhythmics with this characteristic (for example, sotalol) may help prevent arrhythmia, but will be less helpful for termination.
What is reverse use dependence?
'Coumel's law', seen here, refers to this phenomenon.
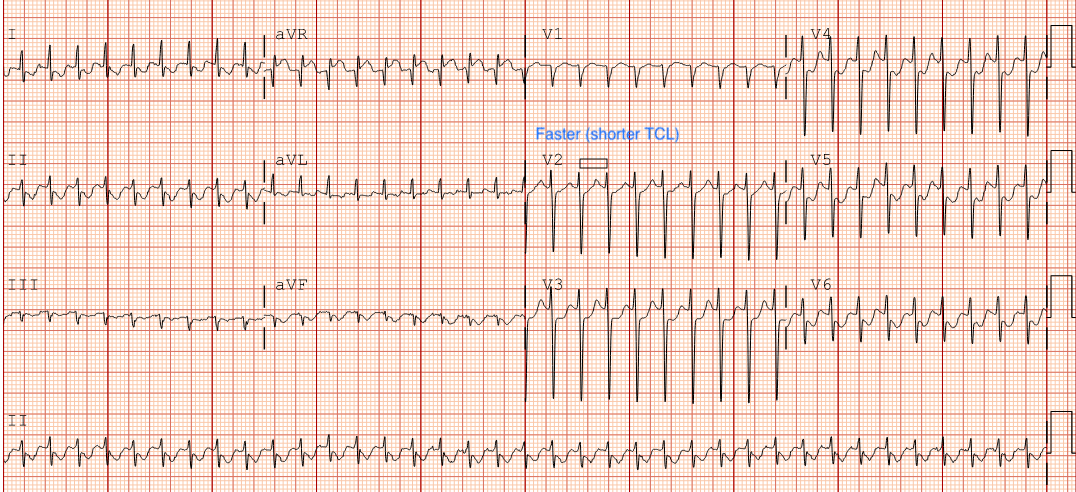
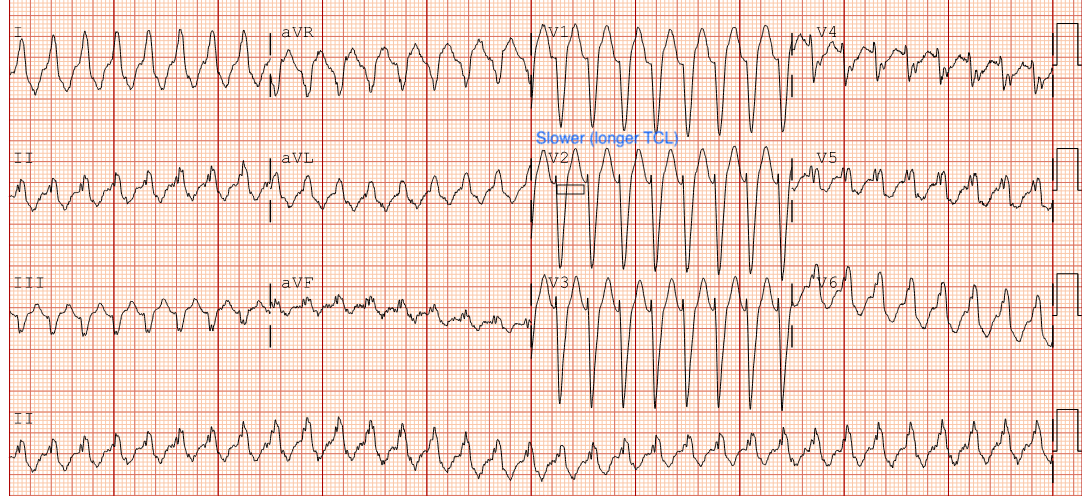
What is shortening of tachycardia cycle length (increasing rate) with resolution of BBB ipsilateral to the pathway?
Evidence of this complication is seen on the ECG below. 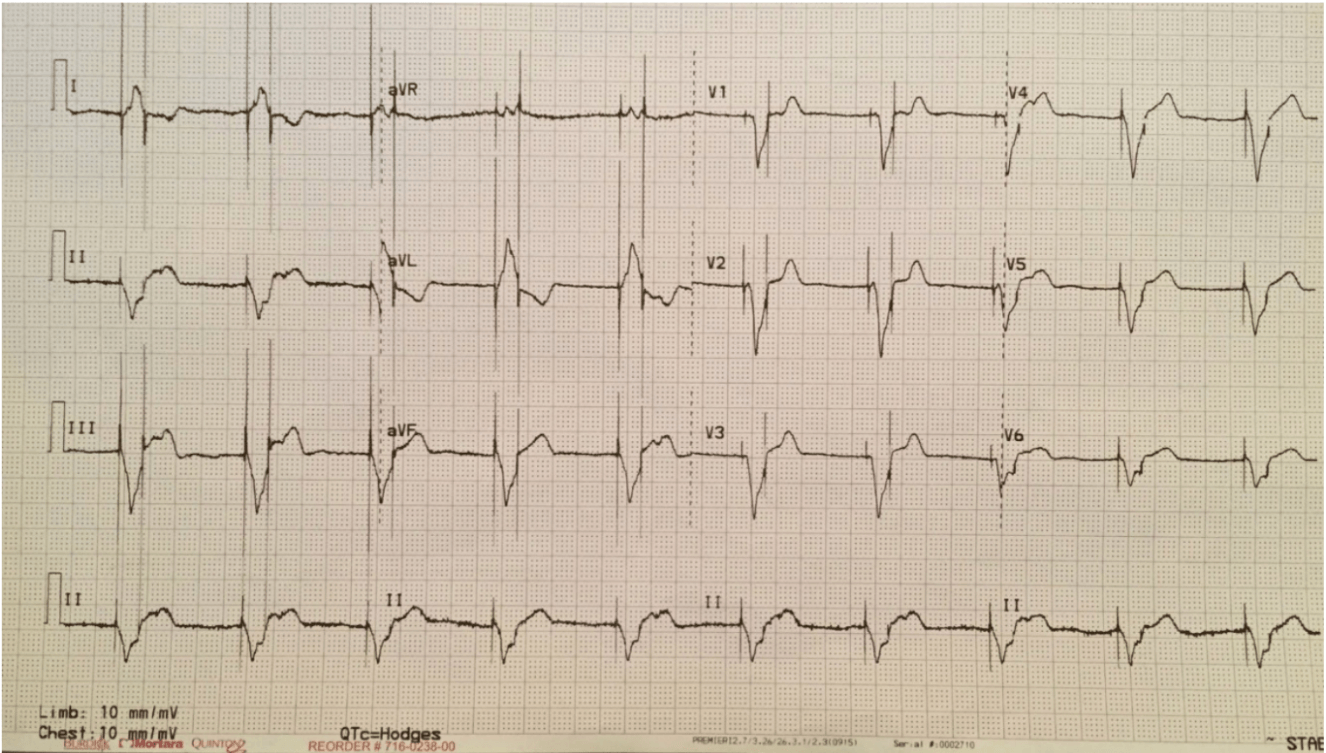
What is lead switch in header?
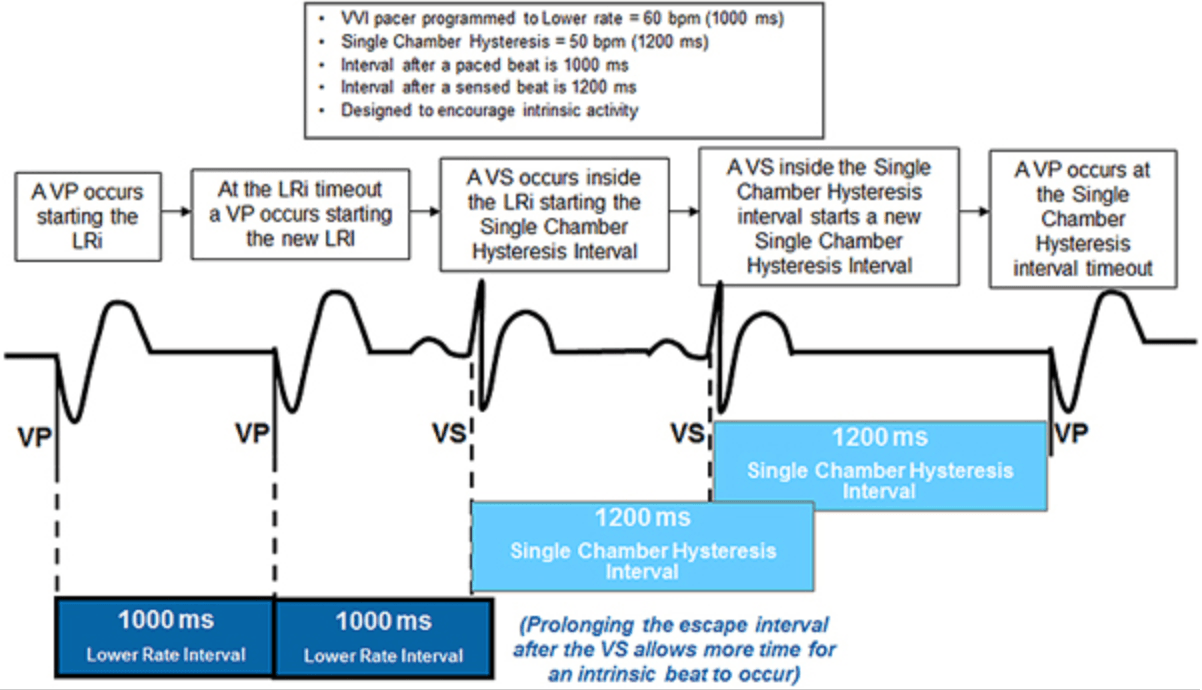
This programming feature would explain seeing an intrinsic rate of 55bpm despite pacemaker set at VVI-60.
What is Rate hysteresis?
This is a description of the tracing below (including rhythm).
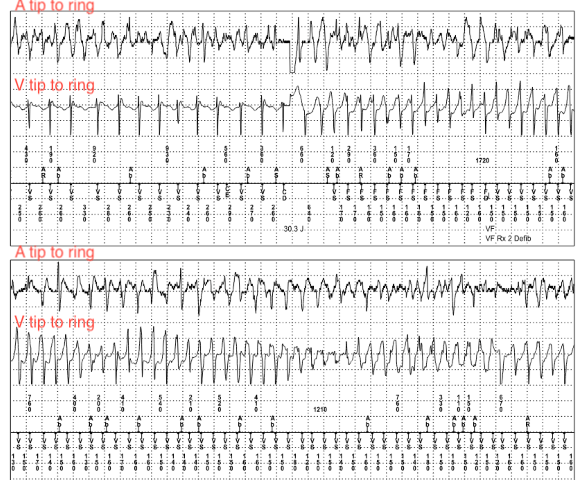
What is inappropriate shock for rapid atrial fibrillation with shock-on-T resulting in PMVT (and atrial fibrillation continues - 'dual tachycardia')?
These are the 6 categories of diagnostic criteria for ARVC (from the 2010 modified Task Force criteria).
What are:
1) Depolarization 2) Repolarization 3) Arrhythmia
4) Family History 5) Imaging 6) Pathology
Definite Diagnosis: 2 Major; 1 Major + 2 Minor; 4 Minor
Borderline: 1 Major + 1 Minor; 3 Minor
Possible: 1 Major; 2 Minor
FINAL JEOPARDY CATEGORY
Cardiac Resynchronization Therapy
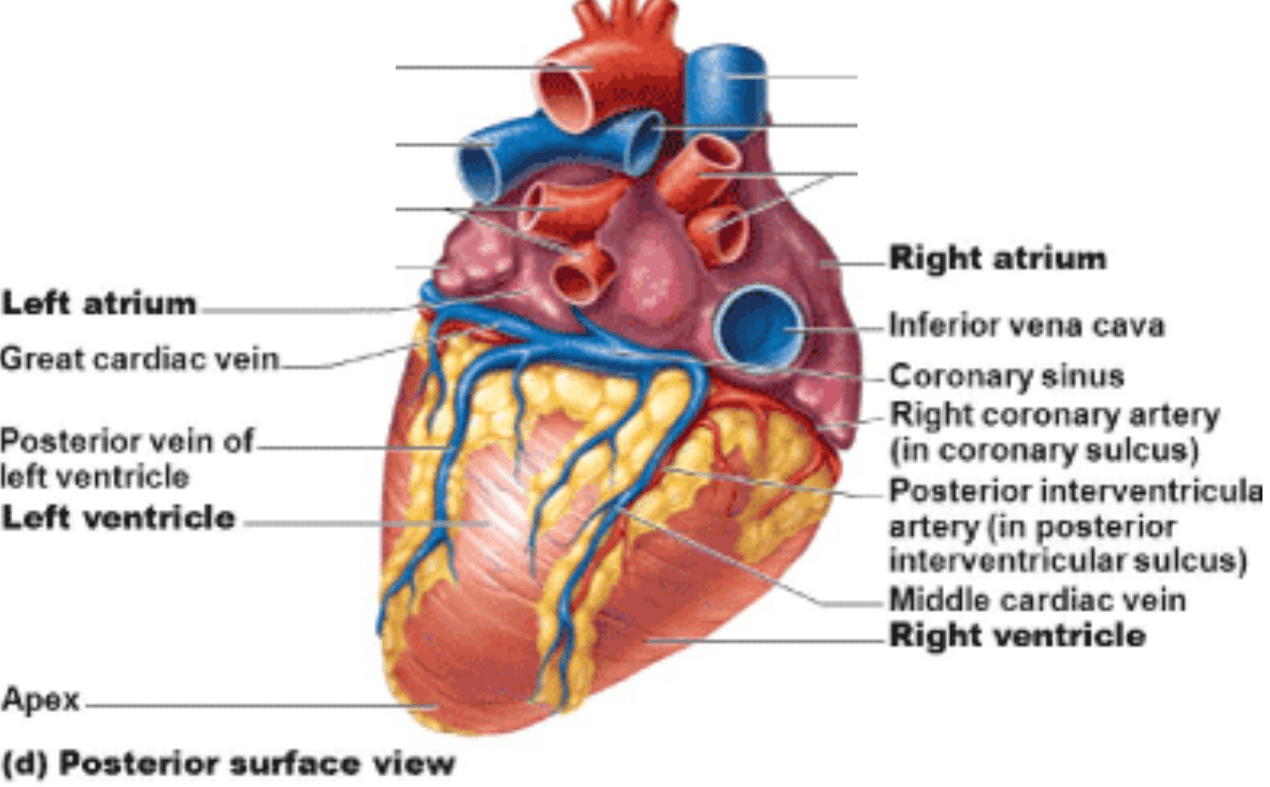
These 2 coronary sinus branches would be considered suboptimal for appropriate CRT pacing.
What are middle cardiac vein/posterior interventricular vein and anterior interventricular vein? (also accept: great cardiac vein, small cardiac vein)