Which of the following is not a valid reason to temporarily defer a patient from donating whole blood?
A. Patient taking Dutasteride
B. Recent travel to a malaria-endemic area
C. Treated colon cancer in 2023
D. Pregnancy
Treated colon cancer in 2023
Generally, patients who have been >12 months in remission (solid organ malignancies) can donate blood.
What is the most likely infectious agent?
Pathology outlines
HSV!
Classic multinucleated cells of HSV infection with nuclear molding and margination.
Squamous epithelial cells with intranuclear eosinophilic inclusion / Cowdry A inclusion (arrow) at the edge of the ulcer.
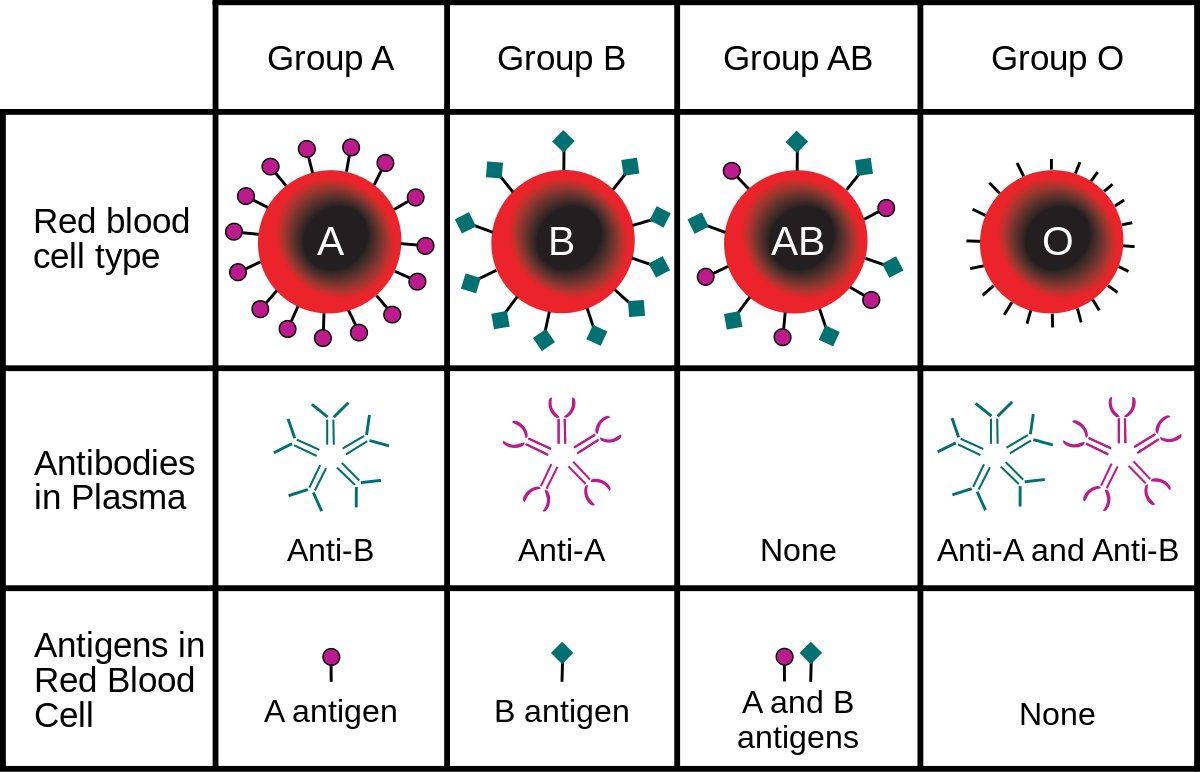
What is the diagnosis?
Pathology outlines
Hemoglobin C disease!
- Homozygosity for C (βC) allele of hemoglobin beta chain (HBB) gene
- Microcytosis
- Numerous target cells
- Irregularly contracted cells
- Occasional rhomboid crystals, more numerous postsplenectomy
- Relative reduction in glycated HbA1C
Mutation most commonly associated with GISTs
KIT!
Activating mutations in the proto-oncogene KIT (~75%) or platelet derived growth factor receptor-α (PDGFR-α) (~10%)
- Leads to constitutive phosphorylation of the receptor tyrosine kinase and activation of downstream pathways → cell proliferation and survival
- KIT and PDGFRA mutations are mutually exclusive in GIST
What initiates primary hemostasis?
Disruption of endothelial cells!
What is the blood type?
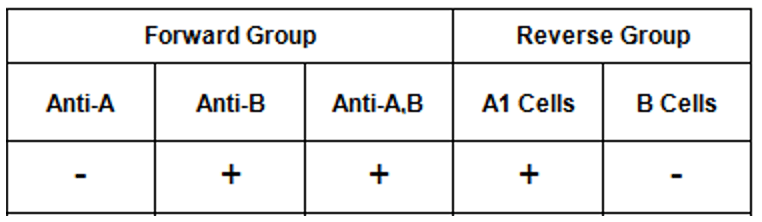
Type B!

What is the most likely infectious agent? What are the cytoplasmic inclusions called?
 Pathology outlines
Pathology outlines
Poxvirus, Henderson-Paterson bodies!
• Small waxy papules with central umbilication
• Children (MCV1): face, trunk, limbs; young adults: lower abdomen, pubis, inner thighs, genitalia
• Opportunistic in HIV (MCV2)
• Resolves spontaneously in a few months
• Histology: large eosinophilic cytoplasmic inclusion bodies in skin biopsy (Henderson-Paterson bodies)
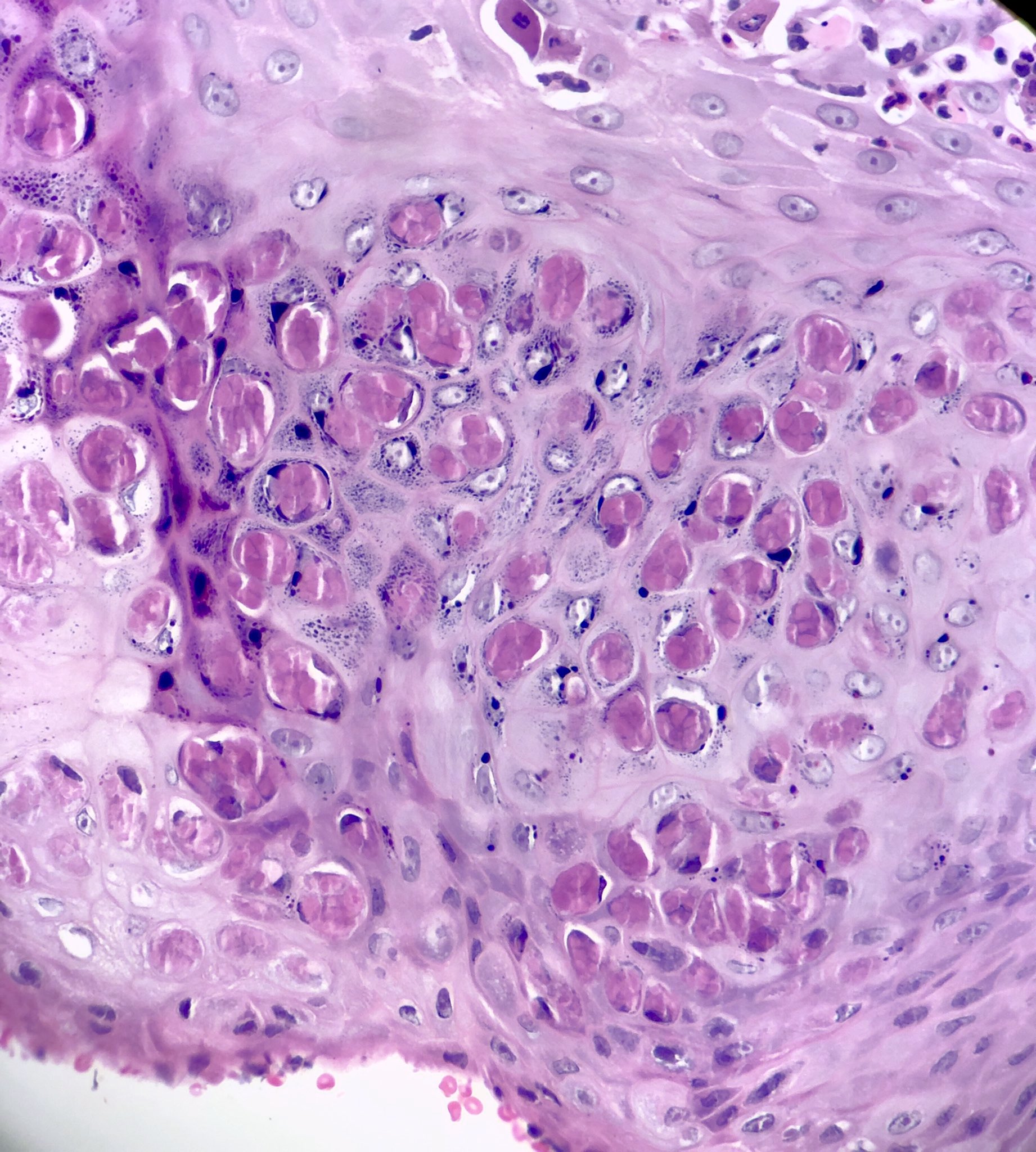
Precursor lesion of conventional follicular lymphoma, but progresses to follicular lymphoma in < 5% of cases
Follicular neoplasia in situ!
- Always an incidental finding
- BCL2 and CD10 are strongly positive in lesional cells
- Neoplastic cells confined to follicle centers of secondary follicles
- Lymph node architecture is preserved

Pathology outlines
Amplification of the MYCN (n-Myc) proto-oncogene is found in 30% of these tumors.
Neuroblastoma!

What are the vitamin K dependent clotting factors/proteins?
Prothrombin (factor II), factor VII, factor IX, and factor X, require vitamin K for their synthesis and activation. Additionally, proteins C, S, and Z are also vitamin K-dependent and play roles in regulating the clotting process, with proteins C and S acting as anticoagulants.
This Duffy antigen phenotype [Fy(a-b-)] confers resistance to what disease?
Plasmodium Vivax Malaria!
The Duffy system is comprised of 2 antigens, Fya and Fyb. These are present on DARC (Duffy associated receptor for chemokines), which is a receptor for Plasmodium Vivax.
Fy(a-b-) is rare in whites, but common in blacks (68%).
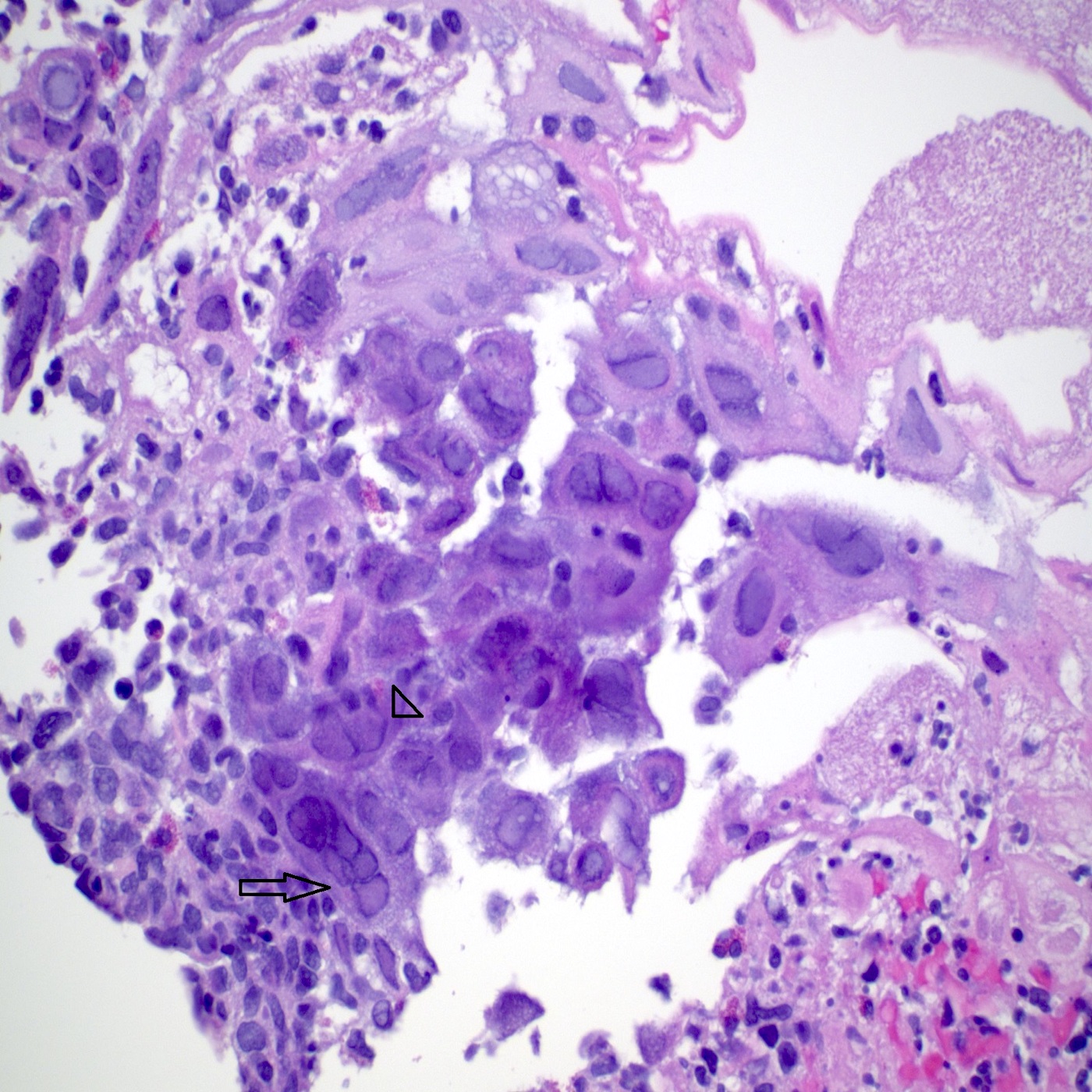
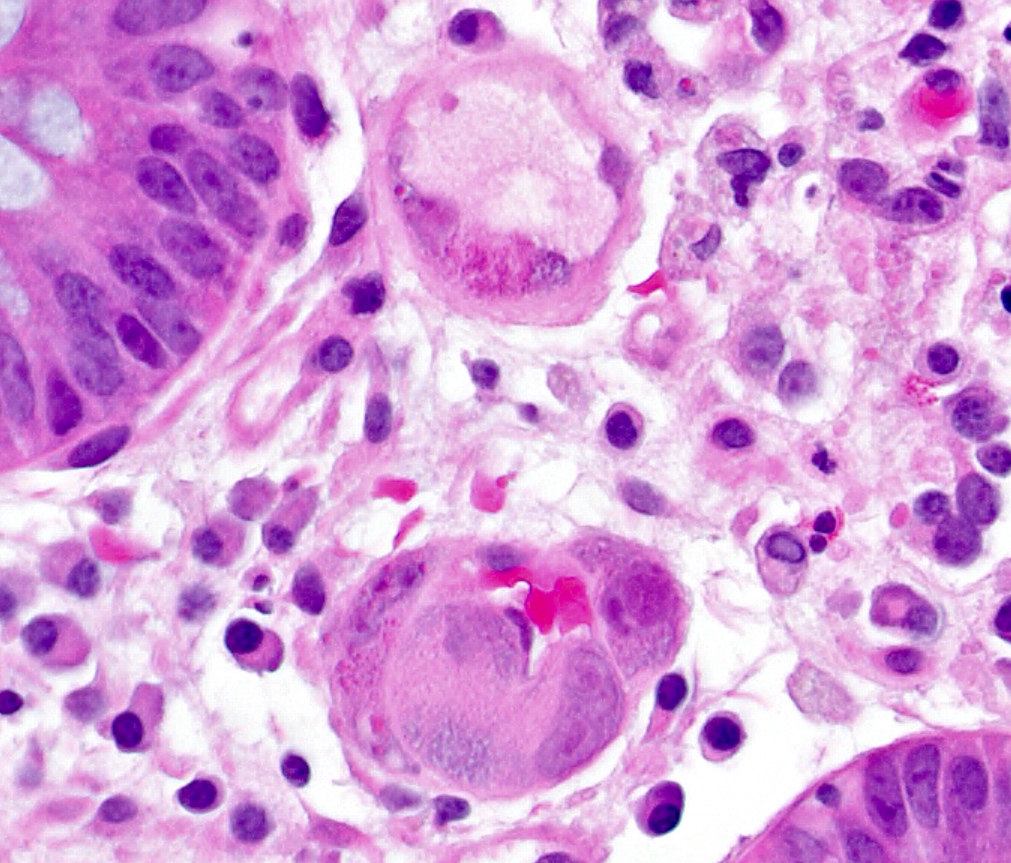
What is the most likely infectious agent?

Pathology Outlines
CMV!
Larger (cytomegalic) cells: Usually 25 - 35 micrometers. Typically 2 - 4 times larger than normal
Owl’s eye:Large ovoid or pleomorphic nucleus with basophilic intranuclear inclusions (Cowdry bodies) surrounded by a clear halo
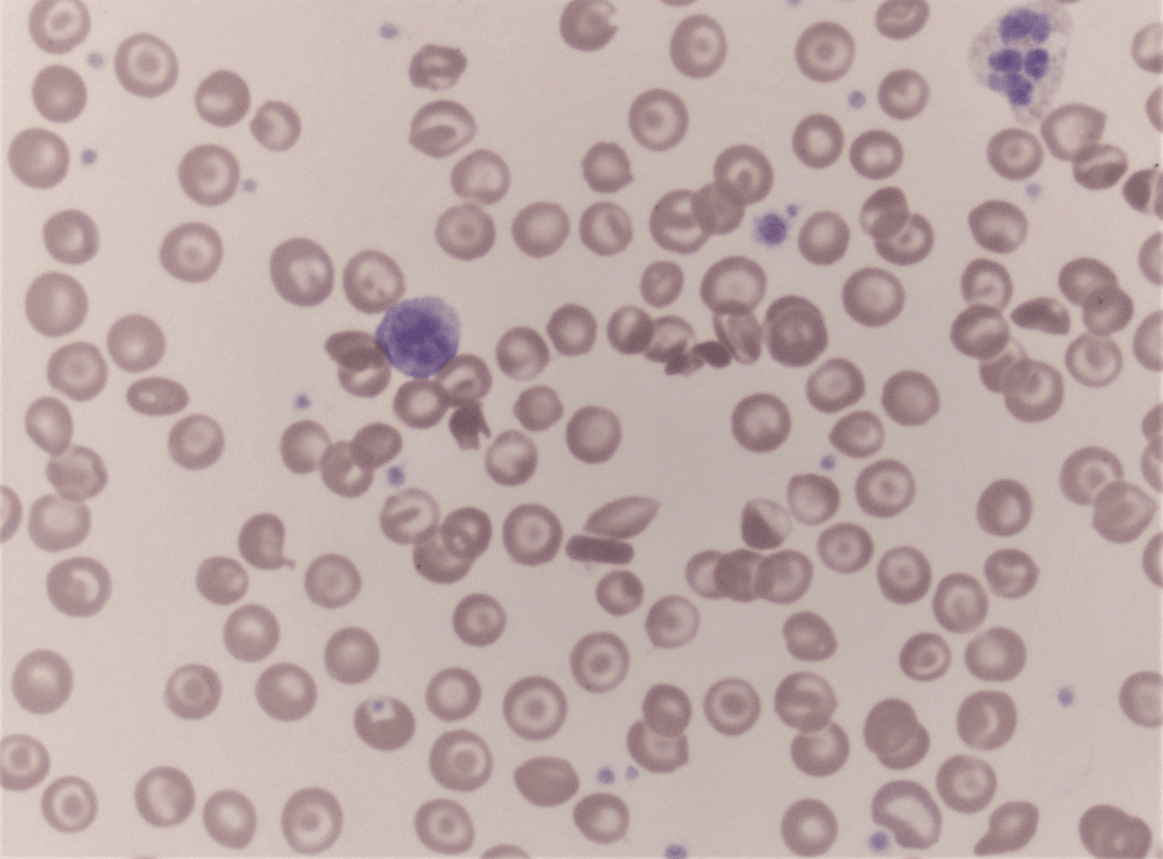
Peripheral blood of a child, diagnosis?
American Society of Hematology
Paroxysmal cold hemoglobinuria (PCH)!
- Paroxysmal cold hemoglobinuria (PCH) is an acquired complement-mediated hemolytic process associated with polyclonal biphasic IgG autoantibodies against the P antigen, which bind at cold temperatures, resulting in activation of the complement cascade and intravascular hemolysis on warming to 37 °C
- Most commonly seen in children < 5 years old with acute hemolysis 1 - 3 weeks after a viral or bacterial infection
- Rarely seen in adults (because of the common use of antibiotics) but historically seen in association with congenital or tertiary syphilis, which causes chronic relapsing PCH
>95% of cases have mutations of the PKHD1 gene
Autosomal recessive polycystic kidney disease
PKD1 (85%) and PKD2 (15%) are associated with autosomal dominant polycystic kidney disease.
Platelet α (alpha) granules contain all but which of the following?
A. Fibrinogen
B. vWF
C. Calcium
D. P-selcetin
C!
Platelet a granules contain proteins such as fibrinogen, platelet derived growth factor (PDGF), VWF, P-selectin, and platelet factor 4 (PF4)
Platelet dense bodies contain nonprotein molecules such as ADP, adenosine triphosphate (ATP), serotonin (5HT), and calcium
Neonatal alloimmune thrombocytopenia (NAIT) is most often caused by what alloantibody? Mothers carrying which allele are at higher risk of NAIT?
HPA-1a!
A strong association exists between HPA-1a alloimmunization and the HLA-DRB3*01:01 allele in mothers, increasing the risk of NAIT.
What is the most likely infectious agent? What are these inclusions called?

Pathology outlines
Rabies, Negri bodies!
Infects nerve fibers (especially the hippocampus): transmitted from the site of animal bite to the CNS via retrograde fast axonal transport. Eosinophilic cytoplasmic inclusions = Negri bodies.
Mostly dogs and cats in areas with poor control.
In areas with good control, most infections are from bats, wolves, coyotes, foxes, skunks, and raccoons.
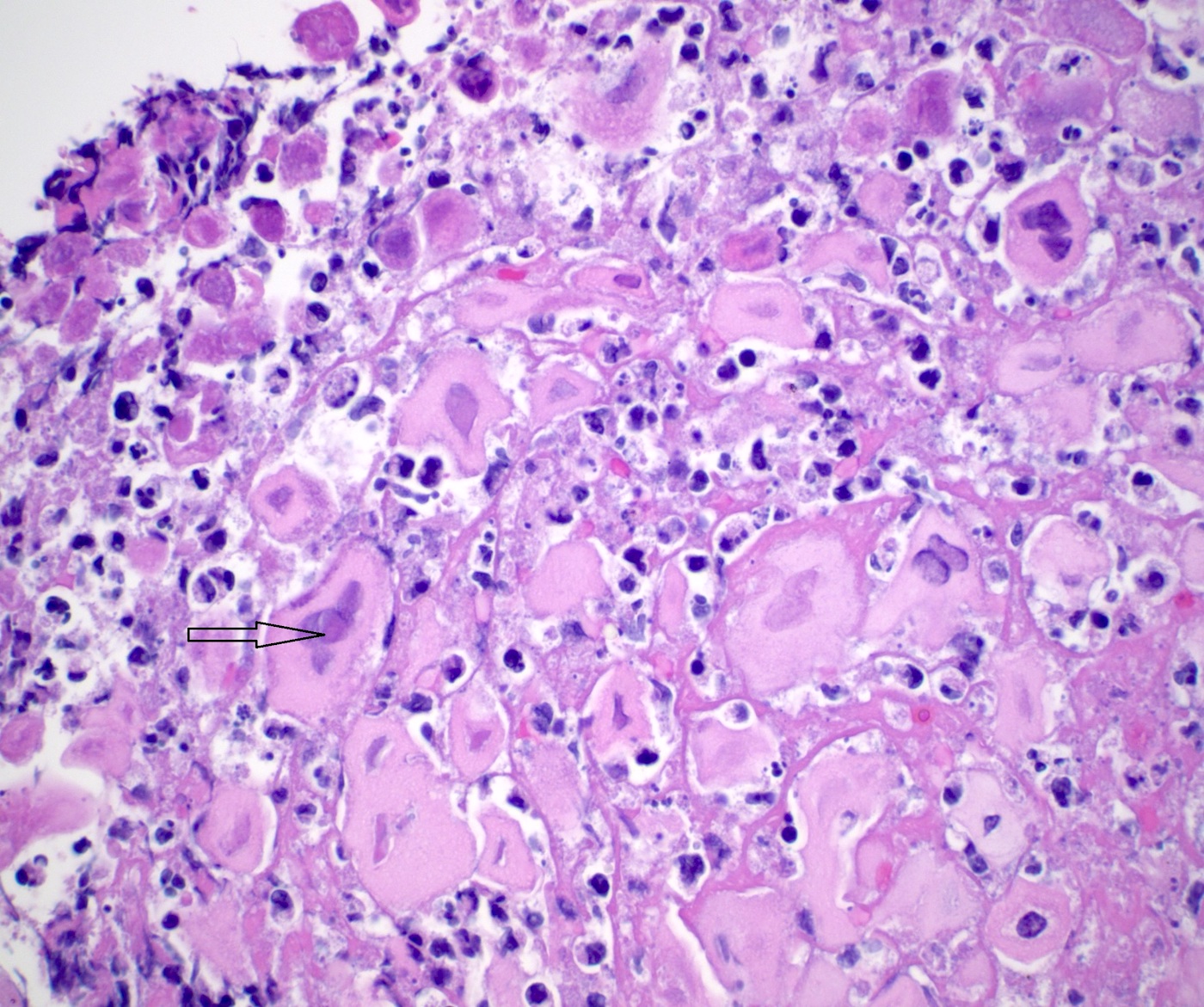
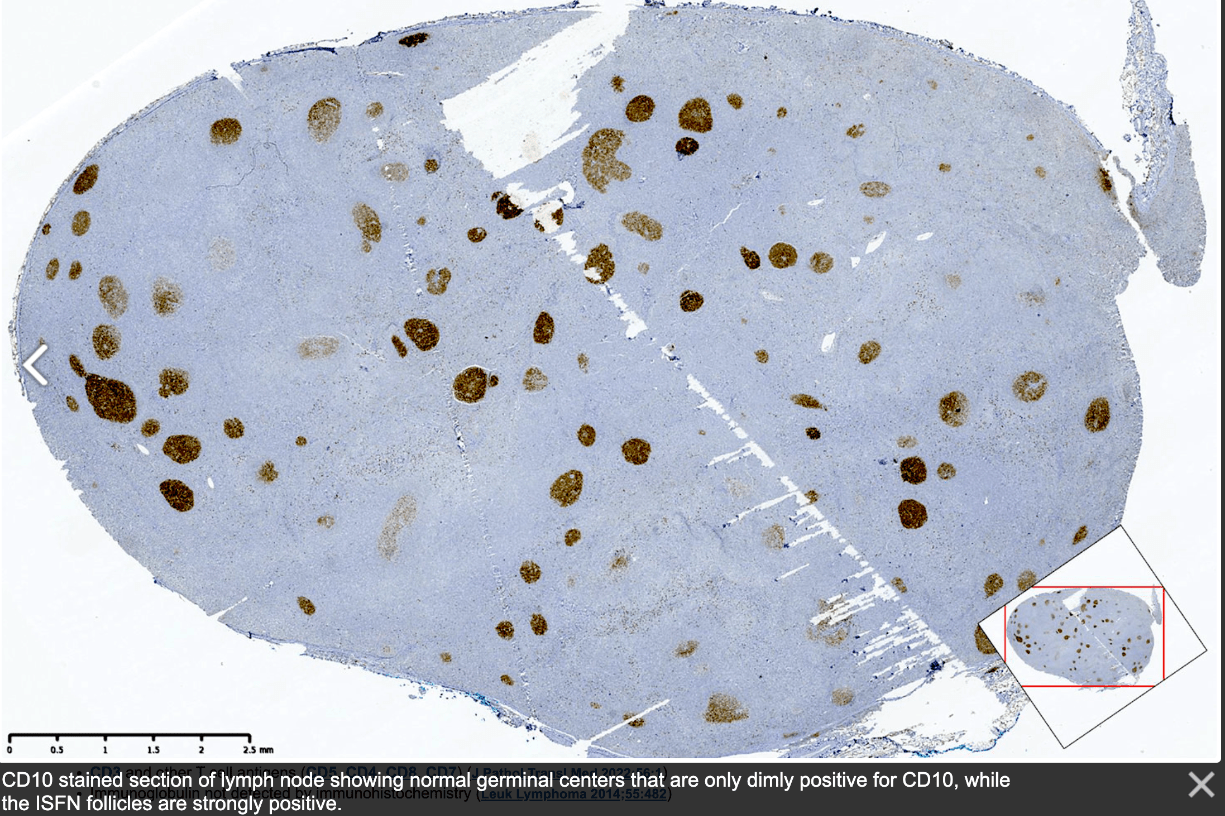
These cells are characteristic of which entity?
A. Blastic plasmacytoid dendritic cell neoplasm
B. Iron deficiency anemia
C. Megaloblastic anemia
D. Acute erythroid leukemia
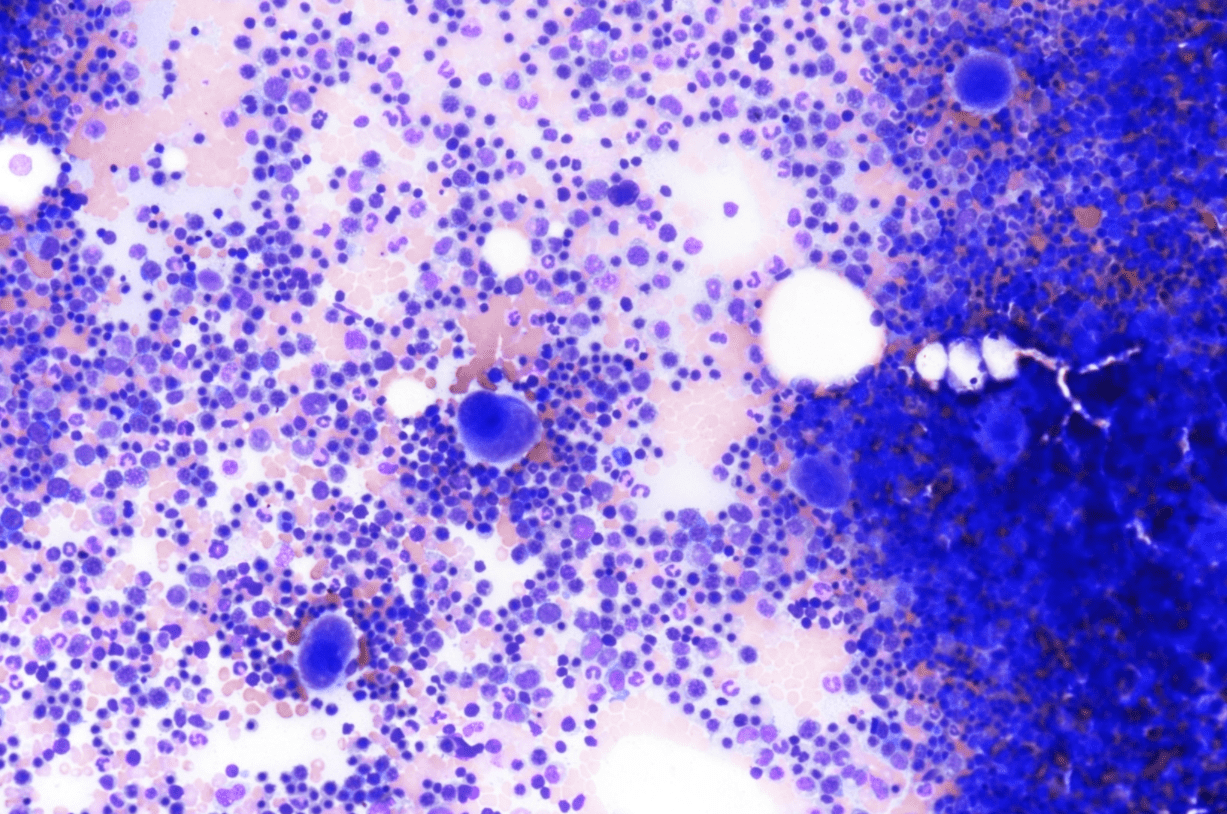
Pathology outlines
- Bone marrow is markedly hypercellular with erythroid hyperplasia and reversal of M:E ratio
- Hallmark is nuclear: cytoplasmic dyssynchrony/dissociation = megaloblastosis
- Erythroid lineage abnormalities: most apparent
- Megaloblasts: have a large, immature nucleus with open, sieve-like chromatin
- Early megaloblasts > intermediate megaloblasts > late megaloblasts
- Some megaloblasts show Howell-Jolly bodies and chromatin stippling
- Frequent normal and abnormal mitoses
- Myeloid lineage abnormalities:
- Giant metamyelocytes
- Giant band forms
- Neutrophil hypersegmentation: often precedes anemia
- Misshapen neutrophils → ineffective myelopoiesis → neutropenia
- Megakaryocyte abnormalities: least common
- Nuclei with open chromatin and nuclear lobular hypersegmentation
- Fragmentation → ineffective thrombocytopoiesis
Dermatofibrosarcoma Protuberans is most often associated with this fusion.
COL1A1::PDGFB
A 75 yo F patient is admitted for a heart valve replacement surgery. The WBC = 9,400/µL, platelet count = 350,000/µL, Hemoglobin = 16 g/dL, and Hematocrit = 42%. The patient has a follow-up a week after surgery and is found to have a platelet count of 100,000/µL. What is the most likely diagnosis?
Type 2 heparin-induced thrombocytopenia (HIT)!
Type 1: occurs early during heparinization, and the platelet count diminishes only mildly. Platelets decrease within 1-2 days of heparinization. This type of HIT is not a danger to the patient, is not immune-mediated, and is not a contraindication to future heparin use.
Type 2: usually noted after day 7 of heparinization, and the platelet count falls by greater than 50% of baseline. It is immune-mediated, and there is a high risk of thrombosis, both arterial and venous.
Risk factors for HIT: Surgery (3-5 fold risk as compared to medical patients) and female gender (2 fold risk)
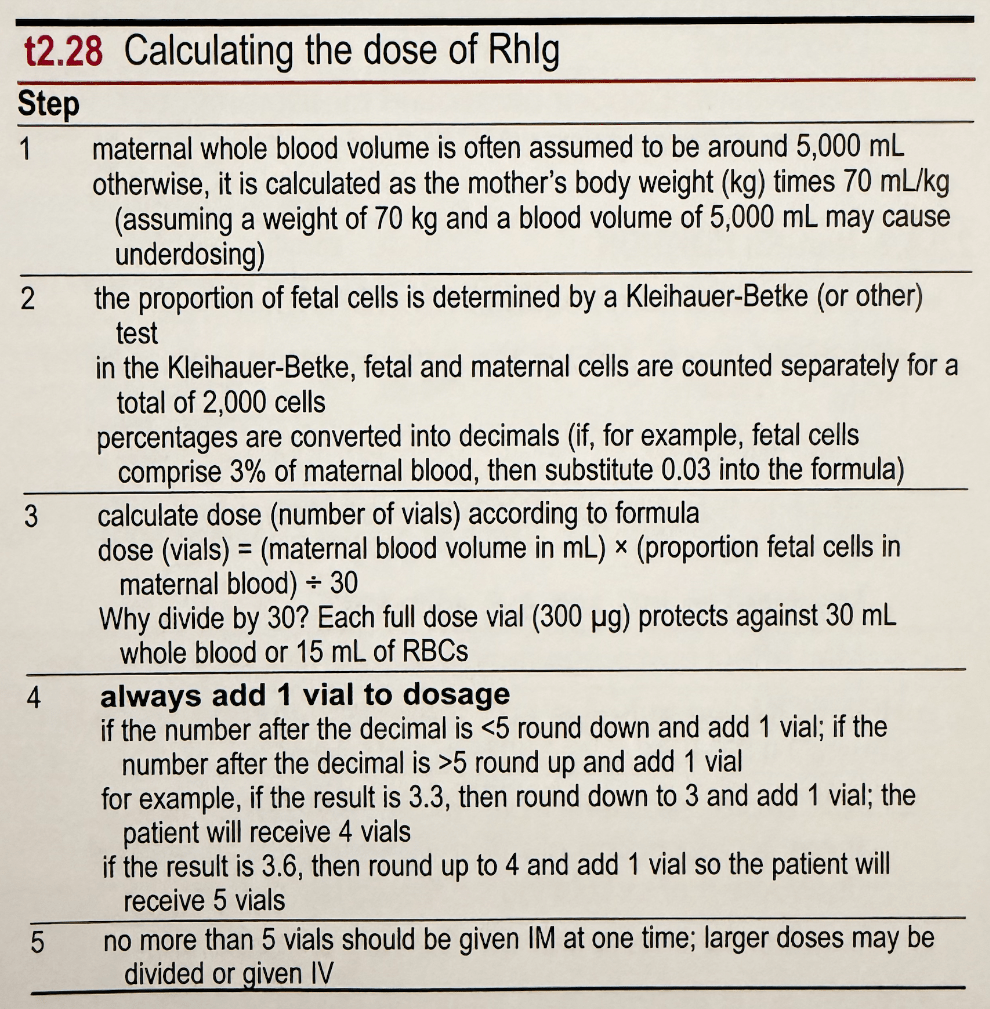
Calculate how many vials of Rhlg are needed for a mother with a presumed blood volume of 5L, and a K-B test of 4.5%.
9 vials!
5,000 x 0.045 / 30 = 7.5
What is the most likely infectious agent? What is the treatment?

Pathology outlines
RSV, supportive care, and Palivizumab if indicated!
- Giant cells (syncytium) with inconspicuous, round, pink intracytoplasmic inclusions and acute inflammation
- Affects small bronchiole epithelium, type 1 and 2 pneumocytes, not basal cells.
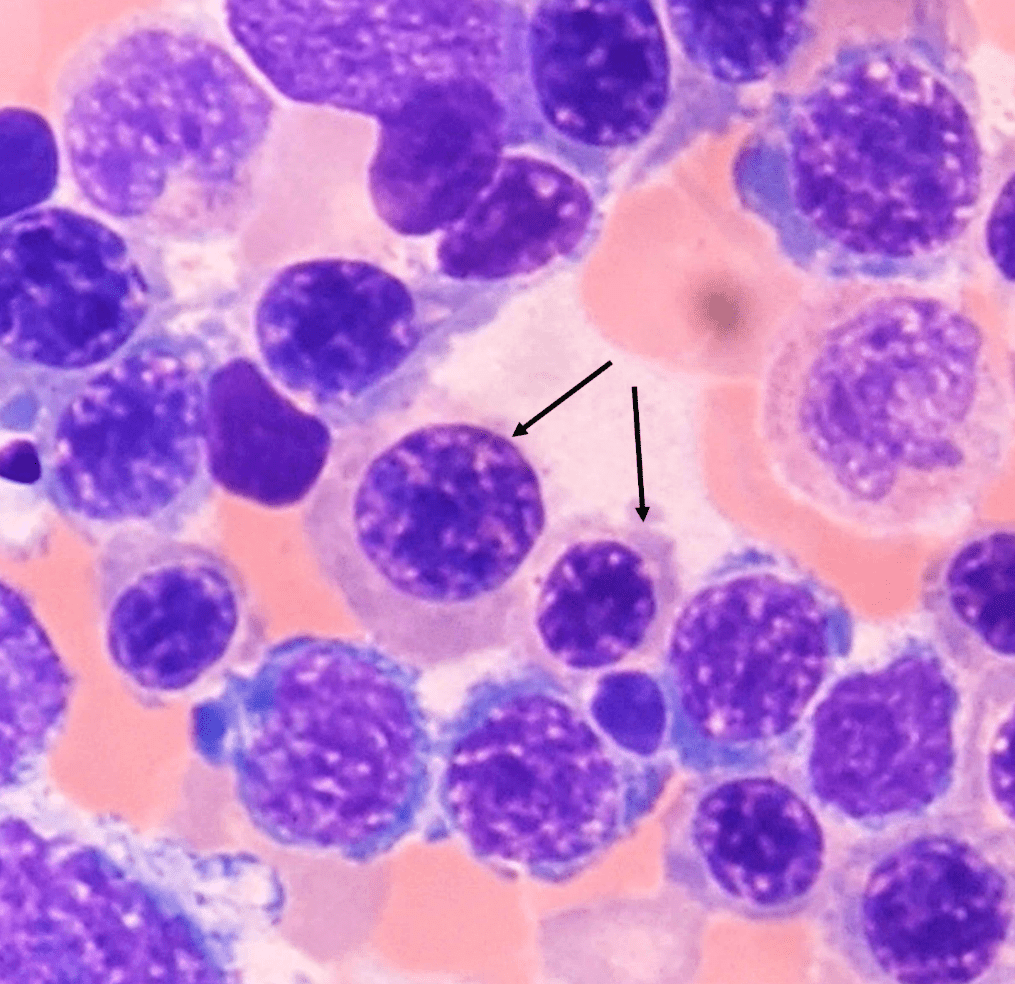
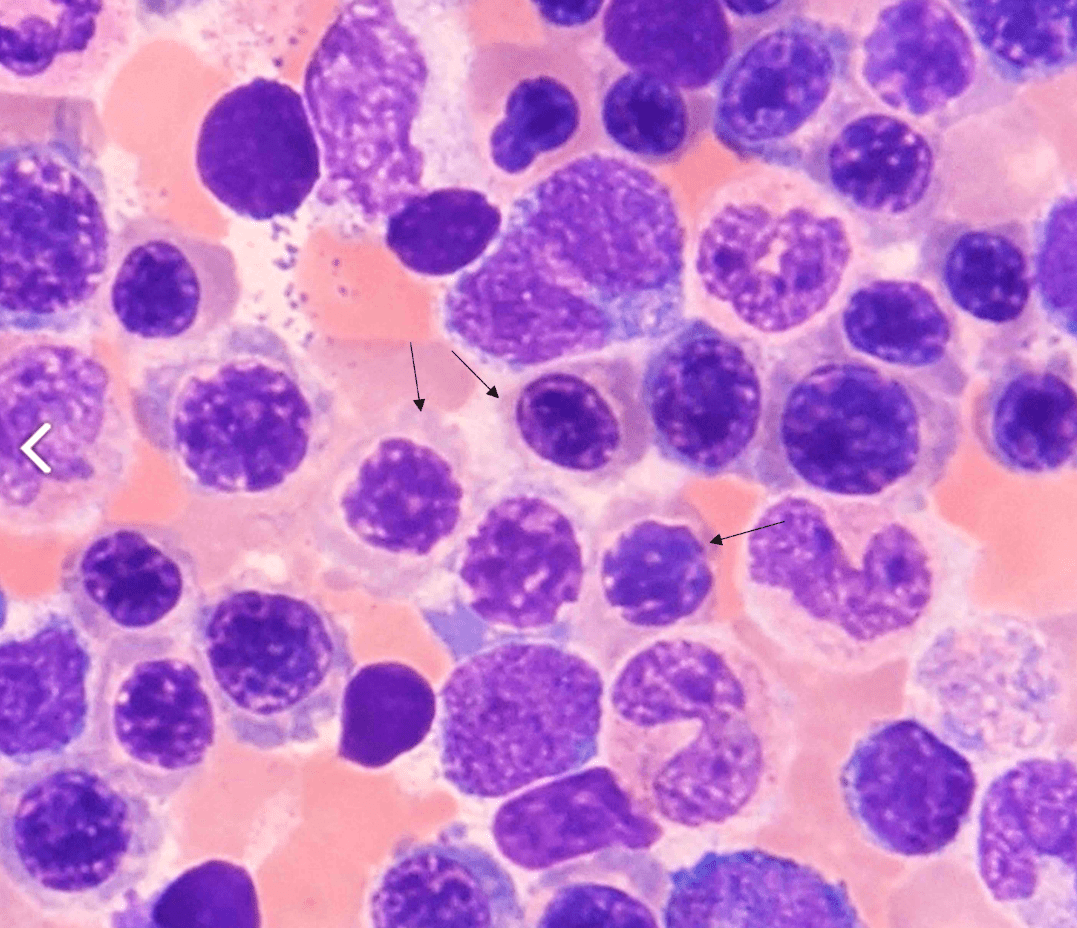
What is the diagnosis?
May-Hegglin anomaly!
May-Hegglin anomaly, along with Sebastian syndrome, Fechtner syndrome, and Epstein syndrome, are autosomal dominant genetic disorders involving mutations in the MYH9 gene encoding for the nonmuscle myosin heavy chain IIA (NMMHC-IIA). All of these entities are associated with macrothrombocytopenias, leukocyte inclusions (Döhle-like bodies), and variable clinical features of sensorineural hearing loss, cataracts, and renal failure.
PAX-FOXO1 fusion gene is found in which entity?
Rhabdomyosarcoma!
Upshaw-Schulman syndrome (USS) is also known as what?
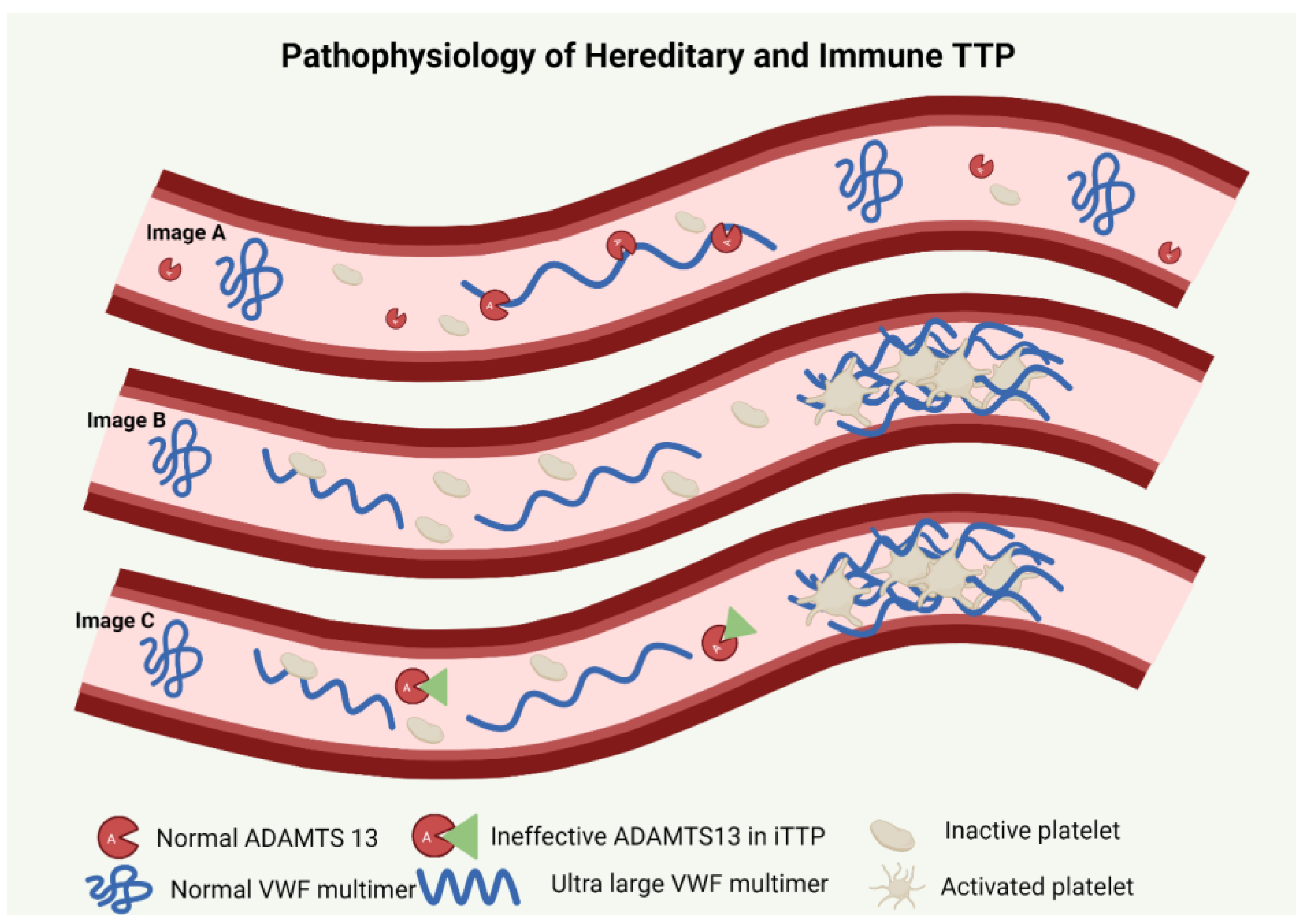
Upshaw-Schulman syndrome (USS), also known as hereditary thrombotic thrombocytopenic purpura (hTTP). It is a life-threatening genetic disorder characterized by a deficiency in the ADAMTS13 protein.