The parents of a 15-year-old boy express concern after finding several items in their son’s room “which looked liked drugs” and were labeled as Spice and K2. Their son claims that “they are no big deal” and help him to relax.
These products are used to mimic the effect of which of the following illicit substances?
A) MDMA/ Ecstasy
B) Marijuana
C) Heroin
D) Phencyclidine
E) Cocaine
Answer: B) Marijuana
-Synthetic cannabinoids ( Spice, K2, Spice Gold, and Chill Out) : analogs of naturally occurring chemicals found in marijuana.
-When ingested in large quantities, synthetic cannabinoids may produce more severe adverse effects than marijuana.
BONUS POINT QUESTION (50 pts):
Synthetic cannabinoids can be detected on standard tox screens : True/ False
An 8-year-old child with sickle cell disease presents for a well-child examination prior to returning to school.
Which of the following would indicate that this patient has met current recommendations for the use of pneumococcal vaccine(s) in patients with sickle cell disease?
A) PPSV23 at 2, 4, 6, and 12 months of age
B) PCV13 at 2, 4, 6, 12, and 24 months of age; PPSV23 at 5 years of age
C) PCV13 at 2, 4, 6, and 12 months of age; PPSV23 at 2 years of age, followed by a 2nd dose 5 years later
D)PCV13 at 2, 4, 6, and 12 months of age
E) PCV13 at 2, 4, and 6 months of age; PPSV23 at 12 and 24 months of age
Answer: C) PCV13 at 2, 4, 6, and 12 months of age; PPSV23 at 2 years of age, followed by a 2nd dose 5 years later
-All children should receive PCV13 at 2, 4, 6, and 12–15 months of age.
-After completion of the PCV13 series, high-risk children ≥ 24 months of age should receive PPSV23 (minimum age for PPSV23 is 2 years).
-Very high-risk children who are immunocompromised, have sickle cell disease, or functional or anatomic asplenia should receive a 2nd dose of PPSV23 five years after the 1st dose.
-A 2nd dose is not indicated for immunocompetent children with cochlear implants, chronic illness (chronic heart/lung disease, diabetes) or cerebrospinal fluid leaks.
What is the etiology of the “honeymoon period” of new-onset Type 1 diabetes mellitus?
A) Residual islet cell function
B) Increased insulin sensitivity
C) Decreased ketone production
D) Excessive cortisol production
E) Decreased carbohydrate intake
Answer: A) Residual islet cell function
BONUS POINT QUESTION (50 pts):
Can you explain its mechanism/ why there is residual islet cell function?
-Longstanding hyperglycemia is toxic to islet cells (termed "glucotoxicity"), and this results in a decline in their function (a "shock" that prevents insulin secretion in the still-functioning cells)>> causes acute onset of DM or DKA
-After starting insulin therapy and improvement of hyperglycemia, the glucotoxicity is eliminated and the remaining islet cells are able to produce insulin again for some period of time >> referred to as the honeymoon period following diagnosis of T1DM.
-This can last for months to years and is not seen in all patients.
-The residual islet cell function can be measured with a C-peptide level.
Following hospitalization for a first-time seizure, a 4-month-old has an EEG that is read as “very high-voltage, random, slow waves and spikes in all cortical areas that are consistent with hypsarrhythmia.”
Which of the following best describes the type of seizure activity commonly associated with these EEG results?
A) Sudden flexion of the neck, trunk, and arms followed by abrupt extension of the neck and trunk, with abduction or adduction of the arms or legs
B) Impaired consciousness associated with generalized bilateral tonic-clonic motor activity
C) Focal motor activity associated with an anatomic spread (“march”) activity with consciousness fully maintained
D) Focal motor activity associated with an anatomic spread (“march”) activity with impaired consciousness
E) Rhythmic lip smacking associated with nystagmus and generalized transient hypotonia
Answer: A) Sudden flexion of the neck, trunk, and arms followed by abrupt extension of the neck and trunk, with abduction or adduction of the arms or legs
BONUS POINTS QUESTION (50 pts)
What is the initial drug of choice in the treatment of this condition?
Infantile spasms
-Onset: usually 3 to 7 mo age
-seizure activity often follows arousal, includes spasms, characterized by a sudden flexion and adduction of the extremities, along with simultaneous flexion of the neck and trunk.
-usually ≤ 10 seconds, occur in clusters with several spasms during a single cluster.
-characterized by hypsarrhythmia on EEG (high-voltage, asynchronous, chaotic, slow wave and spike activity in all cortical areas)
-Prognosis is poor
-Rx: i.m ACTH or oral vigabatrin (recommended in those with both infantile spasms and tuberous sclerosis)
Patient with chronic sinusitis and repeated pulmonary infections
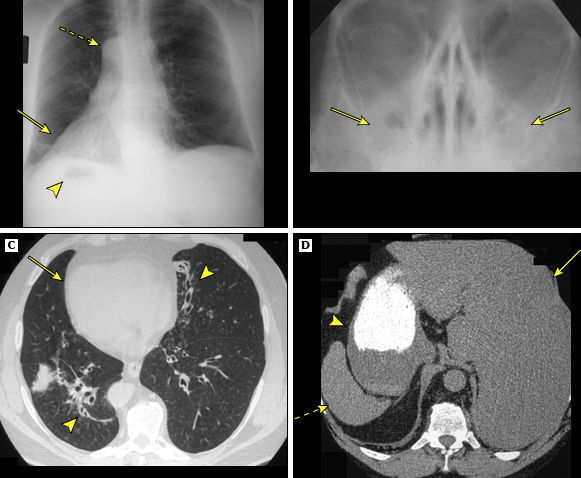
Answer: Kartagener syndrome
-Triad: situs inversus, chronic sinusitis, and bronchiectasis
-subgroup of PCD (Primary Ciliary Dyskinesia)
-infertility 2/2 decreased sperm motility may also been seen
BONUS POINTs QUESTION (50 pts):
What is the definitive diagnostic test for PCD?
transmission electron microscopic (TEM) visualization of specific defects, such as absence of dynein arms or radial spokes and absent, or additional, microtubule assemblies.
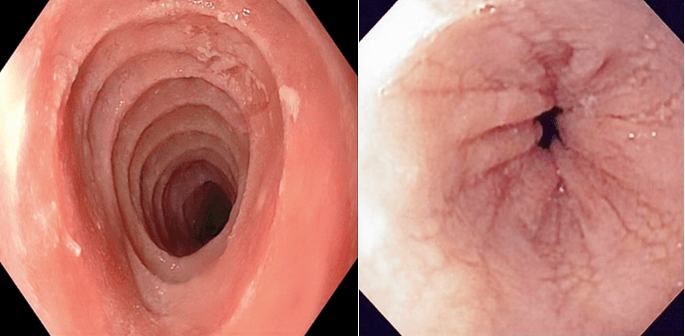
A 15 yo boy is transported to the ED after being found on the restroom floor at his high school. Upon arrival, his RR is 8 breaths/minute. Multiple ectopic beats are noted on ECG. He is stabilized and transferred to the ICU. His parents report that he has recently complained of abdominal pain, has twice vomited blood, and takes multiple over-the-counter antacids. They also state that he is doing poorly in school, has lost weight, is excessively irritable, and “appears to care about nothing except hanging out with his friends.” On physical examination, his pupils are dilated but reactive. The conjunctivae are injected, and his face appears flushed. Excessive secretions and perioral dermatitis are also noted.
Which of the following is the most likely cause of his clinical signs and symptoms?
A) Inhalant abuse
B) Cocaine abuse
C) Oxycodone abuse
D) Ecstasy abuse
E) Hallucinogen abuse
Answer: A) INHALANT USE
BONUS POINT QUESTION (100 pts):
What is a serious pulmonary complication of inhalant use?
-Inhalents: Volatile substances (hydrocarbons/ nitrates)
-often “huffed” or “bagged”
- not detected by standard tox screens
-Within minutes- feelings of euphoria, decreased inhibition, lightheadedness, and impulsivity
-Other side effects:
Pulm (accidental suffocation, chemical pneumonitis, bronchospasm, pneumothorax, and respiratory arrest),
cardiac (arrhythmias, MI),
CNS (disorientation, agitation, and violent and impulsive behavior, seizures and hallucinations)
GI (nausea and vomiting associated with abdominal pain/cramping, anorexia, and weight loss)
Renal (metabolic acidosis associated with potassium and phosphate wasting, urinary calculi, and glomerulonephritis)
Skin/HEENT (perioral eczematoid contact dermatitis, excessive lacrimation, salivation, rhinorrhea)
During a health maintenance examination, a mother expresses concern about the fact that 4 vaccines are recommended; she asks if her son can receive 2 of the 4 during the current visit and the remaining 2 a week later.
Which of the following pairs of vaccines, if given 1 week apart, may result in diminished immunogenicity and a less than optimal immune response?
A) MMR and DTap
B) MMR and varicella
C) Varicella and IPV
D) DTaP and HIB
E) PCV and Hepatitis B
Answer: B) MMR and varicella
- Live vaccines: may be administered simultaneously (during the same visit);
-otherwise administration of individual live vaccines should be separated by at least 4 weeks in order to prevent diminished immunogenicity and a less than optimal immune response.
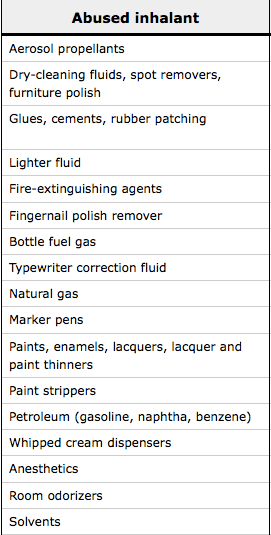
Parathyroid hormone (PTH) is normal in which form of rickets?
A) Hypophosphatemic rickets
B) Vitamin D–dependent rickets
C) Rickets due to deficiency of 1-OH
D) Rickets due to deficiency of 25-OH
E) Renal rickets (renal osteodystrophy)
Answer: A) Hypophosphatemic rickets
BONUS POINT QUESTION (100 pts):
Would each of the following be elevated/ normal/ decreased in hypophosphatemic rickets? : calcium, phosphorus, ALP
-Hypophosphatemic rickets: result of increased renal loss of phosphate and decreased renal tubular resorption of phosphorus.
-PTH is normal because phosphorus loss does not trigger an increase in PTH.
-The remaining labs are normal calcium, low serum phosphorus, and a high alkaline phosphatase (However, ALP is much more elevated in calcipenic rickets compared to phosphopenic rickets)
-The other answer choices will cause an increase in PTH because they result in hypocalcemia, which is the number one trigger for PTH to be released.
-most common rickets in North America.
-most commonly X-linked but can also be autosomal dominant or recessive.
A 4-year-old boy with trisomy 21 presents to the emergency department following his 3rd seizure in the last 4 months. He appears to be in a postictal state, and his initial neurological exam is concerning for lack of withdrawal of the left upper extremity upon painful stimulation. After 48 hours, he is back to his baseline, except that he is still unable to move his left upper extremity. There is no history of trauma, and plain films of the extremity are normal. A cranial CT shows a hypodensity in the right cerebral hemisphere.
Additional imaging in this patient is most likely to reveal which of the following disease processes?
A) Intracranial abscess
B) Atlantoaxial subluxation
C) Right epidural hematoma
D) Intracranial aneurysm
E) Moyamoya disease
Answer: E) Moyamoya disease
BONUS POINTS QUESTION (100 pts)
Name 2 other diseases/conditions associated with Moyamoya disease?
-hypodensity seen on CT and the patient's exam is suggestive of an ischemic infarct or stroke.
-Moyamoya =“puff of smoke" in Japanese >> on cerebral angiography
- bilateral stenosis or occlusion of the arteries around the circle of Willis with prominent arterial collateral circulation.

-may present with a stroke, transient ischemic attack, a history of chronic headaches, or with new onset of seizures.
- can be seen as a primary/ idiopathic disease or a secondary vasculopathy associated sickle cell disease, trisomy 21, cranial irradiation, collagen vascular diseases, and neurofibromatosis Type 1.
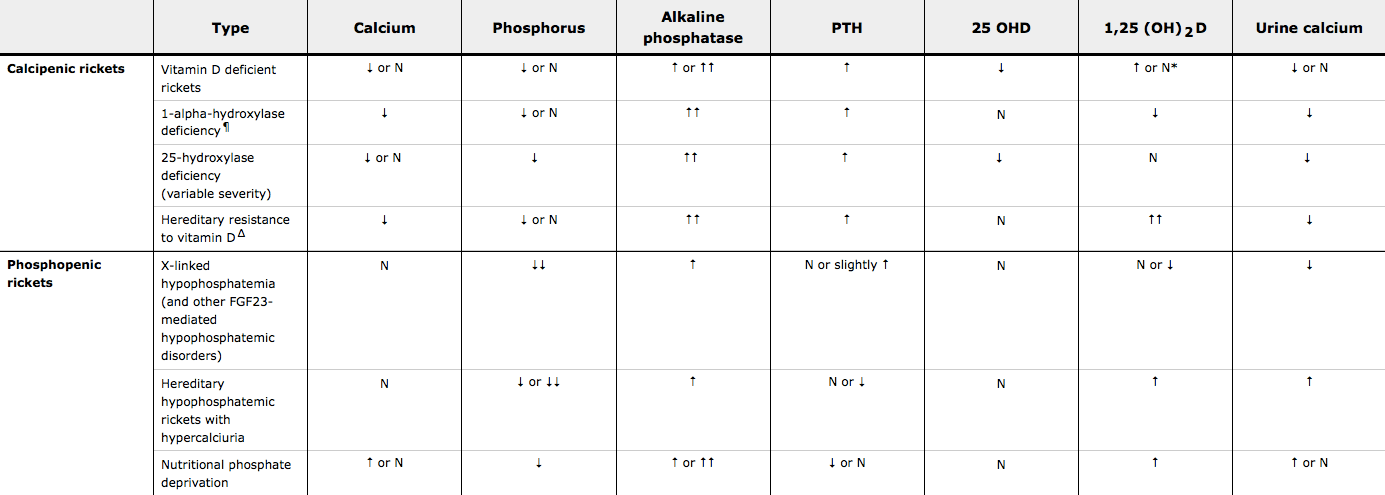
What is the diagnosis?
Following is the appearance of esophagus on endoscopy:
On histopathological exam:
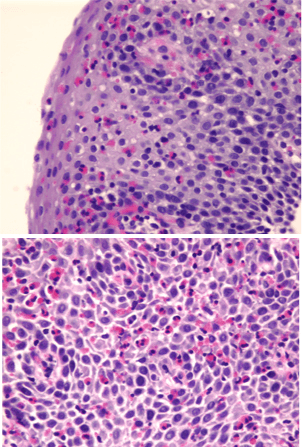
Answer: Eosinophilic Esophagitis
A variety of morphologic features in the esophagus have been described in patients with EoE
-Ringed esophagus/ "trachealization" of the esophagus
-Linear furrowing
-whitish papules (representing eosinophil microabscesses)
-Strictures (particularly proximal strictures)
-Histologic findings include: Peak eosinophil count of ≥15 eosinophils per HPF, eosinophil microabscesses
BONUS POINTS QUESTION (100 pts):
What is the recommended initial pharmacological treatment for EoE?
Answer: PPIs or Topical swallowed corticosteroids (fluticasone/ budesonide spray)
A 17 yo is transported to the emergency department after he was found lying on the bathroom floor during a “rave party” at a local club. Upon arrival, generalized tonic-clonic seizure activity is noted. Following stabilization, laboratory evaluation reveals a serum sodium level of 121 mmol/L.
Which of the following is the most likely cause of this patient’s clinical and laboratory findings?
A) MDMA (3,4-methylenedioxymethamphetamine)
B) Ketamine
C) GHB (γ-hydroxybutyric acid)
D) Methamphetamine
E) Benzodiazepine flunitrazepam
Answer: A) MDMA (3,4-methylenedioxymethamphetamine)
-MDMA acts as both a CNS stimulant and hallucinogen.
-Hyperthermia is a well-known side effect that often causes users to purposely consume large amounts of water, placing them at risk of status epilepticus from hyponatremia due to a combination of water-loading and salt loss.
-Seizure activity may also result from MDMA-induced hypoglycemia
BONUS POINTS QUESTION (150 pt):
Patients who use MDMA while on SSRIs are prone to develop what complication?
A 14-month-old girl presents for a health maintenance visit after being removed from her home by law enforcement personnel because of medical neglect. Upon entry into foster care 2 weeks ago, she received several vaccines after it was determined that her immunizations were not up to date. Since that time, it has been discovered that 2 individuals in her previous home were, up until 3 months ago, incarcerated and found to have tuberculosis. Therefore, a PPD (purified protein derivative) test is recommended for this patient.
Which of the following vaccines can temporarily suppress tuberculin reactivity and therefore result in a false-negative reading following PPD administration?
A) MMR
B) Hepatitis B
C) Hib
D) PCV13
E) DTaP
Answer: A) MMR
-MMR is a live-attenuated virus vaccine >> may temporarily suppress PPD reactivity if it is given prior to the visit when the TST is performed.
-TST may be performed on the day of immunization with MMR; otherwise testing should be delayed for 4–6 weeks because MMR immunization may temporarily suppress tuberculin skin test reactivity and results cannot be considered valid.
-The same recommendation holds true for both varicella and live-attenuated influenza vaccines.
An intellectually disabled 8-year-old, blind due to congenital aniridia, presents for a health maintenance examination. At birth, chromosome studies, ordered as part of an evaluation for ambiguous genitalia, confirmed a male karyotype.
Which of the following has most likely been periodically performed on this patient in order to screen for a known complication associated with his clinical history and current physical findings?
A) Hearing assessment
B) Echocardiogram
C) Renal ultrasonography
D) Thyroid function testing
E) Fasting lipid panel and hemoglobin A1c
Answer: C) Renal ultrasonography
-WAGR syndrome: Wilms tumor, Aniridia, Genitourinary malformations, and Reduced intellectual disability.
-deletion of the WT1 gene (chromosome 11)
-Wilms tumor is reported in up to 50% of cases>> so periodic screening with renal US is required (every three months until age five years).
BONUS POINTS QUESTION (300 pts):
Name 2 other syndromes associated with Wilms tumor.
A 7 yo previously healthy boy is brought to your office for follow-up 1 week after an ED visit for a seizure. On the day of the event, he had walked into his parents’ bedroom at 6:30 in the morning. He could not speak. They noted that his right cheek and eye were twitching, he was drooling, and his right arm had jerking movements. This lasted for 3 minutes and then stopped spontaneously. He was sleepy afterwards. His parents took him to the ED where a head CT w/o contrast was normal. He was observed there for several hours and then discharged. Outpatient EEG result states, “bilateral spikes in the perirolandic regions.” The boy has an appointment with a pediatric neurologist in 2 weeks. In your office today, the boy’s physical and neurologic exam findings are normal. Parents ask you if he will need to take anticonvulsants for the rest of his life.
Of the following, the BEST response is that
A) in this epileptic syndrome, anticonvulsants are often not needed
B) anticonvulsants are usually required for life
C) high-dose corticosteroids are often used as a first-line anticonvulsant
D) MRI brain is needed to determine if anticonvulsants are needed
E) there is no identifiable epileptic syndrome, so it is not certain if anticonvulsants will be required for life
Answer: A) anticonvulsants are often not needed
Benign rolandic epilepsy (BRE)
- a.k.a childhood epilepsy with centrotemporal (periolandic) spikes (BECTS).
-generally starts between ages 5 to 10 years.
-typical seizure is focal with rhythmic twitching of one side of the face and the ipsilateral arm.
-Drooling is prominent, and the child often cannot speak (aphasia) or has repetitive chewing or swallowing during the seizure.
-most often occur during sleep or soon after awakening.
-seizures are infrequent and almost always resolve spontaneously by age 16 to 18 years. Therefore, in many cases, anticonvulsants are not needed.
BONUS POINTS QUESTION (150 pts):
Centrotemporal/periolandic spikes are seen in BRE. What is the typical EEG findings in:
-Juvenile Myoclonic Epilepsy and
-Absence seizures?
JME: 4 to 6 Hz polyspike and wave pattern
Absence seizures: 3 hertz spike and wave (easily provoked by hyperventilation)
Child undergoing evaluation for failure to thrive.

Answer: Russel Silver Syndrome
-severe IUGR and postnatal growth retardation
-prominent forehead, triangular face, downturned corners of the mouth
-hemihypertrophy
-clinodactyly
-feeding difficulties/ poor appetite
-mild developmental delay
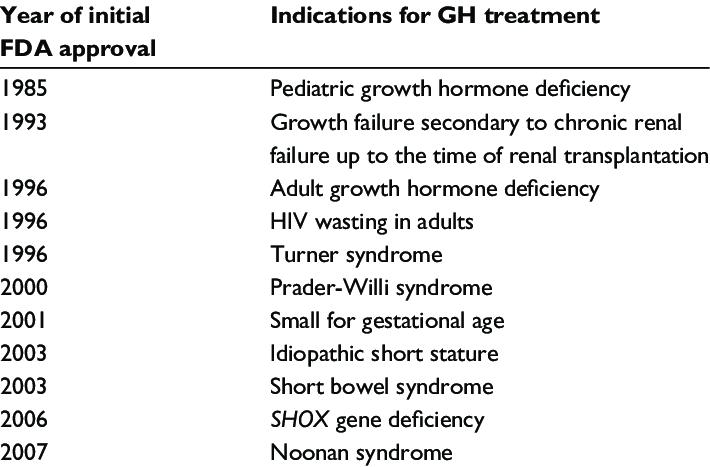
A few reports suggest modest efficacy of growth hormone (GH) treatment of individuals with Silver-Russell syndrome, however not FDA approved.
BONUS POINTS QUESTION (150 pts)
List 2 FDA indications for GH therapy other than GH deficiency?
A 16 yo girl presents to the ED after the principal at her school considered her to be “acting like she was high again.” She is suspected of chronically abusing barbiturates.
Assuming that she ingested a barbiturate within several hours prior to presentation to the emergency department, which of the following eye findings is most likely to be identified upon further evaluation of this patient?
A) Injection of the conjunctiva
B) Papilledema
C) Third nerve palsy
D) Lateral nystagmus
E) Constricted pupils
Answer: D) Lateral nystagmus
-Barbiturates: CNS depressant
-dizzy, floating, or sleepy feeling; ataxia; difficulty with comprehension; and slurred speech. Associated psychiatric symptoms are varied and may include anxiety, depression, euphoria, and/or delirium.
-Overdose is associated with respiratory depression, severe orthostatic changes in BP and bradycardia.
-Lateral nystagmus is a common physical finding of barbiturate abuse.
BONUS POINTS QUESTION (200 pts):
Vertical nystagmus is associated with which drug of abuse?
During review of the immunization status of a recently adopted 8-year-old boy, it is noted that he has never received a pertussis/tetanus-containing vaccine.
Which of the following best describes the recommended schedule for catch-up immunization in this patient?
A) Administer Tdap at this visit, followed by a 2nd Tdap in 10 years.
B) Administer Tdap at this visit, followed by Td in 4 weeks, and a 2nd Td 2 months after the 1st Td.
C) Administer Tdap at this visit, followed by Td in 4 weeks, and a 2nd Td 6 months after the 1st Td.
D) Administer DTaP at this visit, followed by Tdap at 11–12 years of age.
E) Administer DTaP at this visit and in 4 weeks, followed 6 months later with Tdap.
Answer: C) Administer Tdap at this visit, followed by Td in 4 weeks, and a 2nd Td 6 months after the 1st Td.
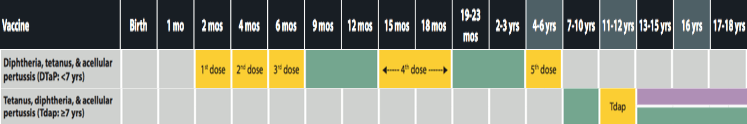
-For children ≥ 7 years of age who have never received a pertussis-containing vaccine, or for those who are not fully immunized (total of 5 doses) with DTaP vaccine prior to 7 years of age, a single dose of Tdap vaccine should be included in the catch-up series. If additional doses are needed, Td vaccine should be used.
-If the first dose of DTaP/DT or Tdap/Td was administered at ≥ 1 year of age, as in this case, a Td vaccine is indicated in 4 weeks, followed by a 2nd Td vaccine 6 months after the 1st Td.
-In the catch-up series, a 4th dose is only required if the 1st dose of DTaP/DT was administered at < 1 year of age.
-Dose 5 is not necessary if dose 4 was administered at age 4 years or older.
-For children who receive Tdap as part of a catch-up series at 7–10 years of age, an adolescent Tdap vaccine dose at 11–12 years of age may be administered.
-For women of child-bearing age, a single dose of Tdap is recommended during each pregnancy, preferably at 27–36 weeks gestation
-DTaP vaccines are only indicated for children < 7 years of age.
A 14-year-old boy with a 3-week history of limp and unilateral thigh pain is found on plain radiograph to have evidence of anterior displacement of the right femoral neck in relation to the femoral head.
These clinical and radiographic features represent a disorder that is more common among patients with which of the following?
A) Elevated serum levels of thyroid-stimulating hormone
B) Elevated levels of growth hormone
C) Low BMI
D) Elevated levels of urine catecholamine and metanephrine
E) 47,XXY karyotype
Answer: A) Elevated serum levels of thyroid-stimulating hormone
-slipped capital femoral epiphysis (SCFE): disruption of the epiphyseal plate between the femoral head and neck.
-Obesity is a significant risk factor
-The mean age of presentation is 12 years in girls and 13.5 years in boys, near the time of peak linear growth
-Hypothyroidism is associated with SCFE
-Patients prefer to hold the involved extremity in external rotation and abduction;
- Surgical correction is required to prevent avascular necrosis of the femoral head.
BONUS POINTS QUESTION (200 pts):
Which other endocrine abnormality is associated with SCFE?
-Atypical SCFE: <10 yo age, >16 yo age, or weight<50th percentile for age/gender
-Consider other risk factors: renal failure, history of radiation therapy, endocrine abnormalities (particularly hypothyroidism and growth hormone deficiency), genetic disorders (Down syndrome)
A 2-week-old male infant with bilateral clubfeet presents with poor feeding. His mother has noted that he has great difficulty maintaining a strong suck during breastfeeding. On physical examination, his face appears expressionless, and he does not blink or grimace. The workup for congenital myasthenia is unremarkable.
Which of the following findings is most likely to be identified during additional evaluation of this patient?
A) Bilateral choanal atresia
B) 6th cranial nerve palsy
C) Heart defects
D) Urinary tract anomalies
E) Bilateral retinal coloboma
Answer: 6th cranial nerve
Mobius syndrome
-rare congenital dysinnervation syndrome that results from hypoplasia or agenesis of the brainstem nuclei and muscle fibers.
-characterized by unilateral/ bilateral facial nerve (CN 7) paralysis.
-Abducens nerve (CN 6) paralysis leads to impairment of ocular abduction.
-other cranial nerves may also be involved
-expressionless, dull appearance and are unable to smile, frown, suck, grimace, or blink.
-Associated anomalies include cleft lip/ palate, clubfeet, absent fingers and/or toes, and unilateral absence of the pectoralis muscle (Poland syndrome), ET dysfunction and recurrent otitis media, dental abnormalities
BONUS POINTS QUESTION (200 pts):
Name this condition: facial paralysis associated with a painful vesicular eruption within the external auditory canal and vestibulocochlear dysfunction.
11 year old girl with 3 month hx of progressive muscle weakness Eg: difficulty getting up from a chair, climbing stairs, combing hair
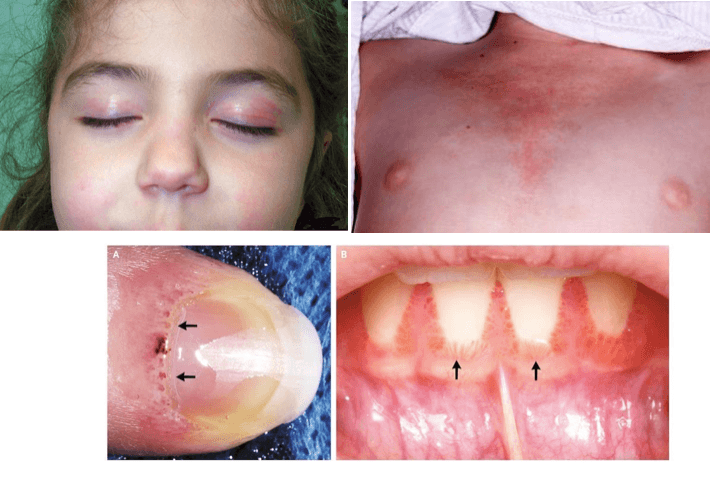
Answer: Juvenile Dermatomyositis
-Symmetrical proximal muscle weakness is the most striking clinical feature
-heliotrope rash (reddish-purple rash on the upper eyelids, often accompanied by swelling of the eyelid)
-Gottron's papules (erythematous, papulosquamous eruption over the dorsal surfaces of the knuckles)

-may also have constitutional symptoms (fever, weight loss, fatigue, and headache), which may appear prior to the onset of muscle weakness and rash
-Other signs: nailfold/ gingival capillary changes, erythematous V- neck rash, skin ulcerations, calcinosis, nonerosive arthralgia and arthritis, lipodystrophy, and insulin resistance
-mostly a clinical diagnosis
-muscle enzymes are not always elevated
BONUS POINTS QUESTION (200 pts):
What is initial treatment of choice in JDM?
During an evaluation of a 17-year-old male, a friend shares that the patient was “snorting some bath salts” obtained at a local convenience store.
Which of the following is most often associated with this recreational drug?
A) Hallucinations and paranoia
B) Wakefulness, sexual arousal, and disinhibition
C) Sedation and a sense of calm and lessened anxiety
D) Increased muscle strength and endurance
E) Heightened sense of focus, alertness, and decreased need for sleep
Answer: A) Hallucinations and paranoia
-Synthetic cathinones (e.g., “bath salts,” “plant food”) - amphetamine analogs
-stimulant + hallucinogenic effects
They may be snorted, smoked, mixed with food and drink, or injected.
-Signs/sx: agitation, combative/violent behavior, psychosis, extreme paranoia, delusions, and vivid, often frightening, hallucinations—all leading to an increased risk of suicide. Mydriasis, hypertension, hyperthermia, diaphoresis, tachycardia, chest pain, and diaphoresis
-Complications may include rhabdomyolysis, electrolyte abnormalities, renal failure, and/or seizures.
-may not be detected on routine urine drug screening
BONUS POINT QUESTION (250 pts)
What drug/ class of drugs is used as first line to control the aggression/ tremors/ seizures secondary to bath salt intoxication?
Which of the following represents current recommendations for administration of the varicella and MMR vaccines in a 15 month old child with HIV infection?
A) The MMR and varicella vaccines may be administered only if the CD4+ T-lymphocyte percentage is ≥ 7.5% .
B) The MMR and varicella vaccines may be administered only if the CD4+ T-lymphocyte percentage is ≥ 15% .
C) The varicella vaccine is contraindicated in children with HIV infection; the MMR vaccine should be administered only if the CD4+ T-lymphocyte percentage is ≥ 7.5%.
D) Both the MMR and varicella vaccines are contraindicated in children with HIV infection regardless of the CD4+ T-lymphocyte percentage/count.
E) Administration of the MMR and varicella vaccines should be delayed until 24 months of age regardless of the CD4+ T-lymphocyte percentage/count .
Answer: B) The MMR and varicella vaccines may be administered only if the CD4+ T-lymphocyte percentage is ≥ 15% .
-For children with HIV infection who are not severely immunocompromised, MMR and varicella vaccines are recommended;
-the MMRV vaccine is not recommended in children with HIV infection.
-For vaccination purposes, severe immunosuppression is defined in:
children 1–13 years of age as a CD4+ T-lymphocyte percentage <15% and
in adolescents ≥ 14 years of age as a CD4+ T-lymphocyte count < 200 lymphocytes/mm3.
-MMR vaccine is recommended at 12 months of age followed by a 2nd dose as soon as 28 days later to induce seroconversion as early as possible, thus decreasing the risk of severe infection with wild-type measles virus.
-Varicella vaccine (2 doses, 3 months apart) is therefore also recommended in HIV-infected patients whose CD4+ T-lymphocyte cell percentages/counts meet the criteria outlined above.
-HIV-infected children and adolescents should receive all inactivated vaccines independent of CD4+ T-lymphocyte percentages/counts according to recommended schedules.
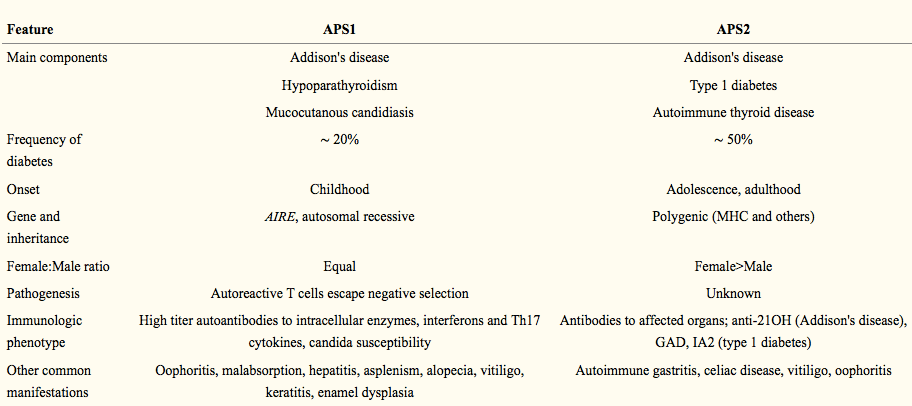
You are taking care of a 12-year-old female with Type 1 diabetes mellitus. She was recently diagnosed with Addison disease. You suspect autoimmune polyglandular syndrome Type 2.
For which of the following is she most at risk with this syndrome?
A) Hypothyroidism
B) Chronic mucocutaneous candidiasis
C) Chronic active hepatitis
D) Nail disease
E) Hypoparathyroidism
Answer: A) Hypothyroidism
-Autoimmune polyglandular syndrome Type 2 (APS2): autoimmune thyroid disease, Type 1 DM, and Addison disease.
-tend to be female
-multiple genes implicated, strong linkage to HLA focus (HLA-D3 and HLA-D4 are common)
BONUS POINTS QUESTION (250 pts):
What are the components of Autoimmune Polyglandular Syndrome Type 1 (APS1) ?
- APS1 or autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy [APECED]
- Triad: chronic mucocutaneous candidiasis + hypoparathyroidism + Addison disease.
-They can also get gonadal failure, hair loss, vitiligo, nail disease, chronic active hepatitis, pernicious anemia, and insulin-dependent diabetes mellitus.
-Thyroid disease is rare in APS1 and Hypoparathyroidism is rare in APS 2.
-AIRE (autoimmune regulator) gene involved
A 14-year-old boy presents for the new onset of right eye pain, swelling, and redness. He has intractable epilepsy and has been taking multiple antiseizure medications.
Which of the following medications is most likely responsible for the patient’s symptoms?
A) Topiramate
B) Valproic acid
C) Phenobarbital
D) Lacosamide
E) Phenytoin
Answer: A) Topiramate
-acute-angle closure glaucoma is a known (possibly idiosyncratic) side effect of topiramate.
-In most cases symptoms resolve after cessation of topiramate
BONUS POINTS QUESTION (250 pts):
Which syndrome presents with a facial birthmark (erythematous patch), seizures and increased risk of developing glaucoma in childhood?
Name the syndrome associated with the following anomalies.
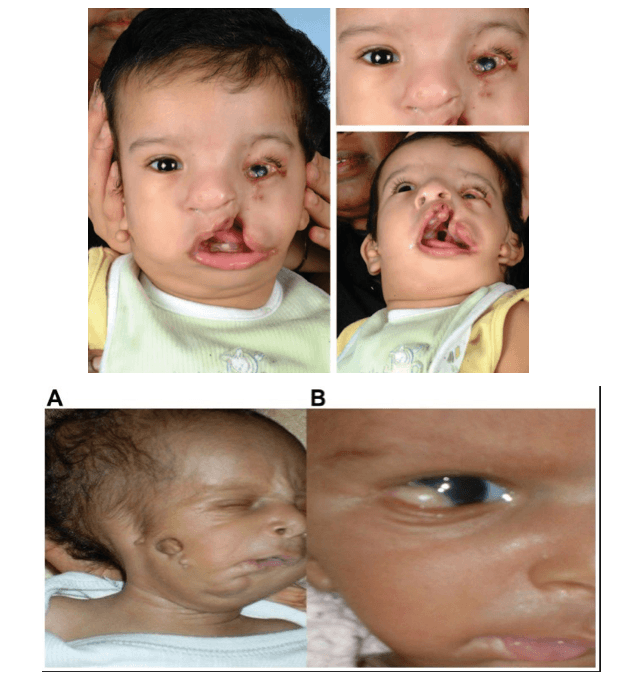
Answer: Goldenhar syndrome
-part of a group of conditions known as craniofacial microsomia (CFM).
-abnormal development of the eye, ear and spine.
-Hemifacial microsomia, cleft lip/ palate
-Benign cysts or growths on the eyes (ocular dermoid cysts), anopthalmia/ micropthalmia
-Partially formed or totally absent ear (microtia), deafness
-Spinal or rib abnormalities
-may also affect the heart, lungs, kidneys, and CNS
BONUS POINTS QUESTION (250 pts):
Name these 2 syndromes also associated with facial anomalies:
