35yo Black woman with HMB, anemia with hgb 7.0, ongoing pelvic pressure.
Two other names for fibroids?
myoma
leiomyoma
solid neoplasm composed of smooth muscle cells and fibroblasts
30yo patient with pap smear cytology showing ASC-US, HPV HR positive.
HPV neg: repeat test in 3 years
HPV pos: colposcopy
DOUBLE JEOPARDY:
How would management be different if patient age 22?

When after unprotected intercourse will a pregnancy test turn positive?
Depends.
Safest answer- can begin to check after day 1 of missed period
Could be as early as 1 week p UPI, could be as late as 2-3 weeks later
LMP- gives GA
conception- happened 2 wks after LMP, time of ovulation, ~14d before missed period day
Fibroids are dependent on what hormone?
Primarily estrogen
DOUBLE 200 pts:
What percentage of patients w uterus have fibroids?
What TVUS findings of a pelvic mass may suggest malignancy?
Cyst greater than 10 cm
papillary or solid components
irregularity
presence of ascites
high color doppler flow



Patients may have concerns that IUD use affects time to conception.
How to counsel about this?
Peipert et al. (AJOG, 2021) assessed the association between IUD use and time to conception
METHODS:
- Multicenter, prospective cohort study
- Fertility After Contraceptive Termination Study
- Participants
- 18 to 35 years
- Contraception discontinued (within past 120 days prior to enrollment) to attempt conception
- No history of infertility or sterilization
- ≥6 months follow-up
- Exposure
- Ever IUD use
- Study design
- Baseline data collected
- Demographic and reproductive characteristics
- Past contraceptive use
- Nucleic acid amplification testing for sexually transmitted infections
- Serology for past infection with Chlamydia trachomatis, Trichomonas vaginalis, and Mycoplasma genitalium
- Follow-up to 24 months
- Baseline data collected
- Primary outcome
- Time to conception
RESULTS:
- 461 participants
- Mean age: 28.2 years
- 38.7% Black | 34.1% low socioeconomic status
- History of IUD use: 59.7%
- Without adjustment, the median time to conception was shorter for participants who had a history of IUD use
- History of IUD use: median 5.1 months to conception
- Never use: Median 7.5 months
- After controlling for confouders, the association of past IUD use with time to conception was not statistically significant
- Adjusted HR 1.25 (95% CI, 0.99 to 1.58)
- Following factors associated with longer time to conception (P<.05)
- Age | Nulligravidity | Black race | Low socioeconomic status
- Past Mycoplasma genitalium infection (P=0.019)
CONCLUSION:
- A history of IUD use was not associated with reduced fertility and the direction of association was in the opposite direction (positive) although not statistically significant
- Other factors were associated with longer time to conception and infertility, including evidence of past Mycoplasma genitalium infection
- The authors state
Patients and providers should be reassured that contemporary IUDs have no impact on the ability to conceive
Which type of fibroid causes the most problems with heavy menses bleeding?
What is the name for a fibroid located beneath the endometrium?
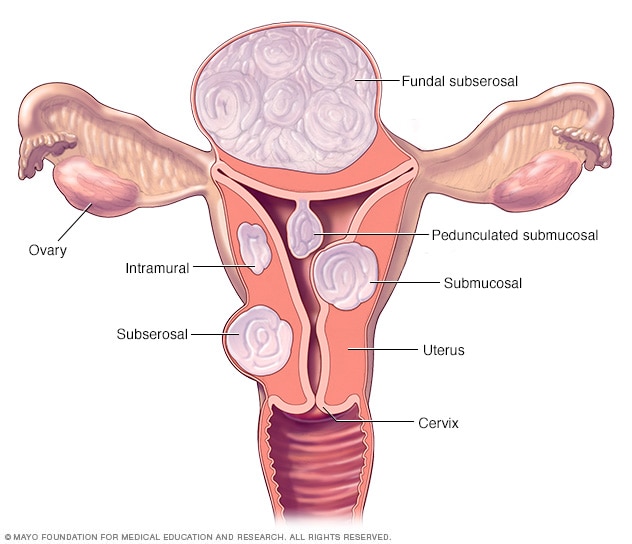
300 point double jeopardy:
which fibroid location is most common?
40yo G0 female with intermenstrual bleeding x 6mo, having "2 periods" every month in addition to spotting.
EMBx results: "proliferative endometrium"
Using it to see if endometrial hyperplasia, atypia, EIN, etc. but outside of that EMBx gives you info re the cycle.
Proliferative endometrium -> follicular phase
secretory endometrium -> luteal phase
Disordered or dyssynchronous endometrium-> ovulatory dysfunction.
Disordered or crowded glands -> anovulatory cycles due to prolonged estrogen stimulation without postovulatory progesterone exposure

Name one MEDICINE and one NON-MEDICINAL treatment for hot flashes in menopause
EBM recommended meds:
Venlafaxine (Effexor)- pt with hx of breast CA
HRT
EBM treatments: Acupuncture
- 17 studies | 1,123 participants
- Studies medium to high quality
- No clear risk of bias
- Baseline number of hot flashes impacted efficacy of acupuncture and sham acupuncture and was adjusted for in subsequent analyses
- Higher the baseline, the greater the acupuncture effect
- Baseline corrected to 8 hot flashes per day
- Frequency decreased at 8 weeks for the following
- Traditional acupuncture: 3.1 hot flashes per day decrease from baseline (95% CI, 2.8 to 3.4)
- Electro-acupuncture decrease: 3.6 hot flashes per day decrease from baseline (95% CI, 3.2 to 4.0)
- Combined analysis of traditional and electro-acupuncture: 3.2 hot flashes per day decrease from baseline (95% CI, 2.9 to 3.5)
- Sham acupuncture: 2.6 hot flashes per day decrease from baseline (95% CI, 2.2 to 3.0)
- Efficacy of electro-acupuncture was comparable to that of
- Selective serotonin reuptake inhibitors (SSRIs)/serotonin–norepinephrine reuptake inhibitors (SNRIs)
- Neuroleptic agents (e.g., gabapentin and escitalopram)
- Efficacy of traditional acupuncture was comparable to tibolone
- Sham acupuncture was more effective than placebo pills but did not reach statistical significance
Time Course
- Efficacy of acupuncture was related to treatment duration with plateau over time
- Onset time: Approximately 2 weeks
- After 8 weeks: Efficacy approximately 80% of maximum
CONCLUSION:
- Acupuncture was efficacious for reducing hot flashes compared to sham acupuncture and placebo pills
- Electro-acupuncture showed similar efficacy to SSRIs/SNRIs and neuroleptic medications (e.g., gabapentin)
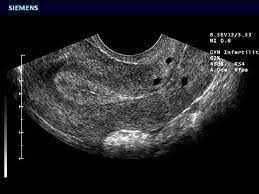
How do you diagnose fibroids?
- Transvaginal ultrasound is used as a screening test
- Sonohysterography can be used to identify and distinguish between type 0, type 1, and type 2 leiomyomas
- 3D Hysteroscopy can be used to distinguish between type 2 and type 3 leiomyomas
- MRI
- Can be used to distinguish between type 4 and 5 leiomyomas
- Can aid with surgical planning, as well as determine vascularity and degeneration
32yo G2P1 with LNG-IUD
Pap result: Normal cytology, HPV negative, +actinomyces seen on pap smear
(Actinomyces: anaerobic gram pos bacteria)
If asx, can leave alone. No abx or IUD removal.
BONUS 200 points:
Which bacteria do predispose to PID for patients with an IUD?
Do you need to take IUD out?
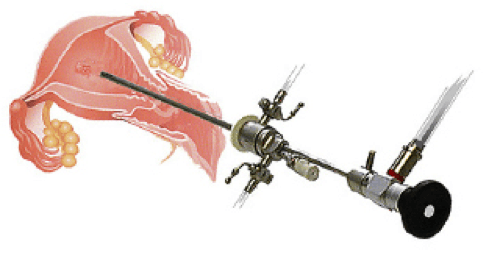
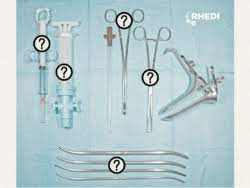
hysteroscopy
can visualize endometrium for diagnostic purposes
or to provide an intervention- Essure (no longer on the market), iud removal, polypectomy etc
DOUBLE JEOPARDY:
What is sonohysterography?

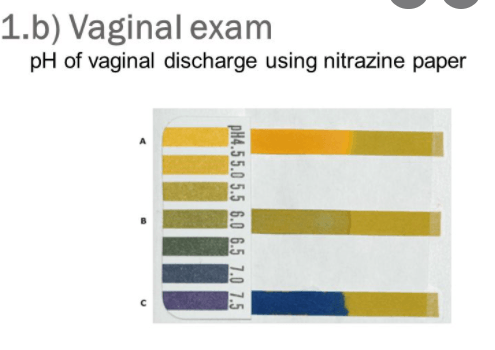
Which letter (A, B, C) is a patient with bacterial vaginosis?
Which letter is a patient with ROM?
Medical management options for fibroids?
- Expectant management can be considered in asymptomatic patients who do not desire intervention
- GnRH agonists (e.g., leuprolide) can be used for both bleeding symptoms and bulk symptoms as short term treatment of leiomyomas, or as a bridge to further treatment
- A 52 mg LNG-IUD can be used for the treatment of AUB-L, although there is a higher rate of expulsion
- Tranexamic acid can be used for the treatment of AUB-L
- Dose (based on RCT cited in the guideline): 1.3 g per dose (two tablets, 650 mg each) three times daily at least 6 hours apart for up to 5 days per cycle over the course of six menstrual cycles
- Begin treatment at the onset of heavy menstrual bleeding
- Maximum daily dose used in study: 3.9 g
- Oral GnRH antagonists (elagolix or relugolix) can be used for treatment of AUB-L for up to 2 years | FDA limit of 24 month regimen due to risk for bone loss which may not be reversible
- Combined and progestin only hormonal contraceptives can be considered for treatment of AUB-L, although there is limited data to support this
- Selective progesterone receptor modulators (mifepristone and ulipristal acetate) have some short-term benefits but are not approved in the US
30yo with dysmenorrhea and dyspareunia
Radiology report reads: Round, homogenous appearing 6cm cyst containing low-level echos within the ovary
Endometrioma ("chocolate cyst")- advanced form of endometriosis
Hemorrhagic debris gives it the ground glass appearance
Refer to gyn, surgery offered typically if >5cm to help with pain and fertility, 75% are in the ovaries
If <2cm endometrioma can repeat US in 6mo, trial COCP or lng-iud if not trying to conceive
1% chance of malignant transformation


nabothian cysts
mucinous retention cysts
"PCOS labs" to order?
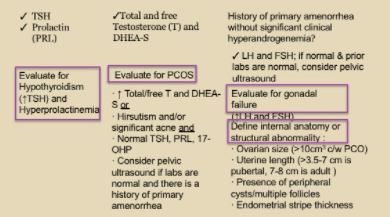

PCOS: clinical diagnosis with anovulatory cycles +/- hyperandrogen signs/sx +/- ovarian cysts on imaging
labs that do correlate well: 86% elevated total testosterone, higher LH
