A 39-year-old woman with new diagnosis of chronic hepatitis B virus (HBV) presents to clinic as a referral from her obstetrician.
She is currently 14 weeks pregnant and has had an uncomplicated pregnancy thus far.
Her laboratory tests were drawn at her initial prenatal visit.
The results are shown in the table below in Figure 1.

What do you recommend to her specific to her liver disease in the setting of pregnancy?
a) US liver
b) HBV DNA quantification
c) entecavir
d) bile acid quantification
e) C-section delivery
In the second trimester, pregnant mothers should have HBV DNA tested.
If maternal HBV DNA is higher than 200,000 IU/mL, antiviral therapy should be started between weeks 28 and 32 to reduce mother-to-child transmission of HBV.
A 40-year-old man with alcohol-related cirrhosis presents with large-volume hematemesis, presumed related to an acute variceal bleed. He is intubated on arrival for concerns regarding his airway protection.
On examination, he is intubated and sedated with scleral icterus and multiple spider angiomas.
He remains tachycardic.
Laboratory tests show a hemoglobin of 6.1 g/dL (reference range [male], 14-18 g/dL), platelet count of 71,000 plts/µL (reference range, 150,000–450,000 plts/ µL), and an elevated lactic acid.
Which of the following is the most accurate regarding the initial management of this patient?
a) He should undergo a blood transfusion with a goal hemoglobin > 10 g/dL
b) He should be started on a PPI
c) He should be started on prophylactic antibiotics
d) He should undergo endoscopic sclerotherapy within 12 hours of presentation
Answer: C
This patient is at high risk of infection, and pro-phylactic antibiotics have been shown to improve a variety of clinical outcomes, including reduced rates of bacterial infections, rebleeding, and death.
A more restrictive transfusion strategy (targeting a hemoglobin of 7-9 g/dL and transfusing when hemoglobin fell below 7 g/dL) was shown to improve survival in a randomized controlled trial that included individuals with cirrhosis.
Although proton pump inhibitors are often started at presentation, it is more important to start a vasoconstrictor like octreotide.
Sclerotherapy has been associated with more side effects than endoscopic variceal ligation.
An asymptomatic patient with cirrhosis who has never bled has a screening EGD showing the above findings in his esophagus.
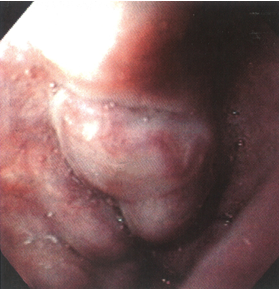
The next best step in management is:
a) Perform endoscopic variceal ligation (EVL)
b) Perform EBL or start non-selective beta blockers
c) Do nothing
d) Refer for transjugular porto-systemic shunt (TIPS)
Answer: B
The patient has large esophageal varices with red markings and is at increased risk of variceal rupture (60% over the next 2 years). The mortality of a variceal bleed is about 20%. Primary prophylaxis (before a bleed) with either a non- selective beta blockers ( propranolol, nadolol or carvedilol) or endoscopic variceal ligation are recommended by the AASLD
A 54 yo woman had colonoscopy for colorectal cancer screening and had a 0.5 cm tubulovillous adenoma removed. When should the patient have the next colonoscopy?
a) 7-10 years
b) 3-5 years
c) 3 years
d) 1 year
Answer: C
The patient has an advanced adenoma. An advanced adenoma is defined as an adenoma >10mm; or with tubulovillous/villous histology, or with high grade dysplasia or with cancer. The US Multi-Society Task Force guidelines from 2020 recommend repeating colonoscopy for an advanced adenoma (tubulovillous adenoma) in 3 years.
A 52-year-old man with history of liver transplantation 5 years ago for alcohol-related cirrhosis comes to see you in follow-up.
He has a history of hypertension, hyperlipidemia, and recent diagnosis of type 2 diabetes.
His body mass index is 31 kg/m2. He takes tacrolimus 4 mg twice daily for immunosuppression.
Other medications are amlodipine 5 mg daily, metformin 500 mg twice daily, and multivitamin.
Laboratory test results that were completed before the office visit are shown below in Figure 1.

What would be your approach to his elevated creatinine?
a) decrease amlodipine to 2.5 mg daily
b) decrease tacrolimus to 3 mg twice daily
c) stop amlodipine and switch to furosemide
d) stop metformin and switch to insulin
e) stop tacrolimus and switch to cyclosporine
Decreasing tacrolimus to 3 mg twice daily is correct as the first step to possible calcineurin inhibitors renal toxicity is to lower the dose of tacrolimus while following the transaminase levels.
His current tacrolimus level is on the higher range of normal and lower levels should be targeted if transaminase levels remain normal.
He has metformin for his diabetes which should be safe for his renal function while not worsening his obesity risk (as insulin does).
His amlodipine is likely not contributing to renal injury and furosemide would not be indicated as a substitute for amlodipine in this setting.
Cyclosporine would potentially worsen his hypertension and could still contribute to renal injury so should not be tried.
A 39-year-old woman who is in the 28th week of her fourth pregnancy is referred to you for evaluation of elevated liver enzymes.
She initially presented to her obstetrician with pruritis and was found to have the following laboratory test results are shown below.
Liver biochemistries before pregnancy were all within normal limits, and recent viral hepatitis panel and autoimmune serologies are all negative.
What finding on further diagnostic testing would confirm the diagnosis of intrahepatic cholestasis of pregnancy (ICP)?
a) mild intrahepatic biliary ductal dilation on US
b) serum total bile acids of 8 umol/L
c) serum total bile acids of 18 umol/L
d) normal heat-stable alkaline phosphatase
e) normal 5'-nucleotidase
Answer: C
In the absence of other causes, a serum total bile acid level higher than 10 µmol/L in a pregnant patient with pruritis is consistent with ICP.
ICP is not associated with biliary ductal dilation.
Laboratory tests aimed at determining whether alkaline phosphatase is elevated due to a liver problem (heat-fractionated alkaline phosphatase and 5'-nucleotidase) do not play a role in the diagnosis of ICP.
A 61-year-old woman with compensated hepatitis C-related cirrhosis is found to have a 2.1 cm mass on a right upper quadrant ultrasound.
She has had multiple images of her abdomen in the last 2 months related to abdominal pain, including a computed tomography (CT) scan of her abdomen with oral and intravenous contrast 7 weeks before and a noncontrast CT of her abdomen diagnosing her with kidney stones just last week.
Neither of these images had any concerns for a liver mass. Her liver disease is compensated (Child-Pugh class A) and her liver tests all remain at baseline with a low Model for End-Stage Liver Disease (MELD) score.
An alpha fetoprotein level is checked and normal at 2.3 ng/mL.
Which of the following should be recommended as a next best step in evaluation?
a) No further testing is needed at this time, as she has had recent cross-sectional imaging. She should have an ultrasound in 6 months for ongoing HCC screening
b) She should undergo MRI without contrast given the discrepancy between teh US and CT scans. If a mass is seen she should undergo biopsy.
c) She should undergo a multiphasic CT of her liver with IV contrast
d) She should be scheduled for an US-guided biopsy of this liver lesion with interventional radiology to rule out malignancy
Answer: C
This patient was found to have a liver mass on ultrasound, which is highly concerning for HCC given her baseline cirrhosis. Diagnosis can often be made without biopsy, when dynamic imaging of the liver (either CT or MRI) reveals the typical features of HCC (arterial hypervascularity and early washout in the portal venous phase). Her recent CT imaging is not adequate to evaluate for HCC. HCC would not be evident on noncontrast CT imaging of the liver and could easily be missed on a single-phase CT of her abdomen with contrast (which would have only obtained a venous phase). A biopsy would not be necessary if the lesion can be accurately diagnosed with typical imaging features.
A 47-year-old woman with mild asthma and seasonal allergies is seen for evaluation of dysphagia for the past 3 years. She notes food moving down her esophagus slowly, especially when she eats chicken and rice. She denies history of food impactions. She reports heartburn and takes calcium carbonate antacids as needed, typically several times weekly.
She denies weight loss.
On endoscopy, the esophagus has mucosal edema in the proximal esophagus and mucosal edema and longitudinal furrows in the distal esophagus. A 4 cm hiatal hernia is noted. Biopsies demonstrate 35 eosinophils per high-power field in the distalesophagus and 15 eosinophils per high-power field in the mid esophagus.
Esophagus as below:

What is the best initial treatment for her condition?
a) antihistamine
b) esophageal dilation
c) food elimination diet
d) PPI
e) swallowed topical steroids
Answer: D
This is a case of eosinophilic esophagitis (EoE) based on esophageal dysfunction and esophageal eosinophilia greater than 15 eosinophils per high-power field, particularly in the setting of a person with asthma and seasonal allergies.
The treatment of inflammation in EoE includes proton pump inhibitors (PPIs), swallowed topical steroids, food elimination, and, potentially, biologics. In this case, the best initial treatment is a PPI, which has a response rate of 30% to 50% in adults. For this case, modest esophageal eosinophilia is noted, with more eosinophilia in the distal esophagus, which may be more likely to respond to PPI therapy.
Additionally, with the hiatal hernia and reflux symptoms, she likely has both gastroesophageal reflux disease and EoE; thus, a PPI is the best first choice. Given the overall availability, low cost, and few side effects, PPIs are often the first choice in treatment of EoE, especially in individuals with heartburn symptoms.
Antihistamine therapy does not reduce esophageal eosinophilia significantly. Esophageal dilation can be used to treat strictures and rings; however, it does not improve esophageal inflammation. A food elimination diet and swallowed topical steroids may be considered for some patients; therefore, individualized treatment of EoE with PPI, swallowed topical steroids, or food elimination diet based on patient preference and discussion of benefits/risks is reasonable.
A 72-year-old man is admitted with hematemesis and melena. He has a history of coronary artery disease and had a coronary stent placed 2 months ago. He is currently taking dual antiplatelet therapy (DAPT) with aspirin 81 mg qd and clopidogrel 75 mg qd. He reports a past history of peptic ulcer but has had no gastrointestinal symptoms recently and has not been taking a PPI or H2-antagonist. He denies NSAID and anticoagulant use. He was hemodynamically stable and physical examination was otherwise unremarkable. At EGD on the following morning, he had a 1 cm clean-based prepyloric ulcer and there was no fresh or altered blood in the gastric lumen. Gastric biopsies taken at sites separate from the ulcer were negative for H. pylori. What do you recommend?
a) IV PPI therapy for 72 hours, then transition to oral PPI therapy, continue oral PPI therapy for at least the duration of DAPT
b) IV PPI therapy for 72 hours, then transition to oral PPI therapy, recommend discontinuation of clopidrogel, continue low-dose aspirin with oral PPI
c) Start oral PPI therapy, and continuie this at least for the duration of DAPT
d) Start oral PPI therapy, and continue this while on DAPT, stop oral PPI therapy when clopidrogel stopped, then continue patient on low-dose aspirin without oral PPI
Correct answer: C
The patient has had a bleed from a prepyloric ulcer and appears to be H. pylori-negative (multiple biopsies from different areas of the stomach; no blood in gastric lumen; no recent PPI treatment – so low probability of a false-negative test for H. pylori). He is at high risk of recurrent ulcer bleeding because of his dual antiplatelet therapy. He will require continued PPI treatment at least for the duration of dual antiplatelet therapy – and this should be continued even if the clopidogrel is stopped and the low-dose aspirin is continued. At the time of endoscopy, he only had a clean-based ulcer with no endoscopic evidence of current or recent bleeding. Therefore, he does not need IV PPI therapy and should have been started on oral PPI therapy.
A 43-year-old woman with history of liver transplantation for hepatitis B virus/hepatocellular carcinoma cirrhosis presents to your office for follow-up.
Her transplantation was 3 months ago, and she has been feeling well.
She is adherent to her medications.
Her transaminase levels were elevated for the past few weeks at 2 to 3 times the upper limit of normal, and you arranged for an outpatient liver biopsy last week.
She is here to review the pathology.
Which biopsy findings listed below would support your decision to bolus with high-dose steroids?
a) Central edotheliitis
b) Councilman bodies
c) Ground glass hepatocytes
d) Hepatic foam cell arteriopathy
e) Noncaseating biliary granulomas
Answer: A
Central endotheliitis is correct because it represents 1 of the 3 major histologic features associated with acute cellular rejection, which requires boluses of high-dose steroids.
The other 2 features are a mixed inflammatory infiltrate in the portal triad (primary lymphocytic) and destructive or nondestructive nonsuppurative cholangitis involving interlobular bile duct epithelium.
Ground glass hepatocytes is incorrect as that describe features seen in hepatitis B virus.
Noncaseating biliary granulomas is incorrect as that describes findings seen in primary biliary cholangitis.
Councilman bodies is noted in viral-related liver injury.
Hepatic foam cell arteriopathy is seen in chronic rejection, which is not treated with boluses of high-dose steroids.
A 31 year old woman is currently hospitalized for complications of her pregnancy. She was in the 35th week of her pregnancy when she developed edema, and was hospitalized with a blood pressure of 165/95, proteinuria, headaches and nausea and vomiting. She had a vaginal delivery 8 hours ago, and shortly after her vaginal delivery developed abdominal pain in the right upper quadrant and a fever of 101. She currently has a blood pressure of 130/90, pulse rate 95, temperature 100.9, RR 22, and pulse oximetry 98%. On exam she is completely oriented but in significant pain. Her abdomen is tender mainly in the upper regions, with a palpable uterus but no other palpable organs. Her current labs show AST 2255, ALT 2198, total bilirubin 2.2, albumin 2.0, alkaline phosphatase 344, INR 1.9, platelet count 32,000, Hgb 8.7, Hct 26.4, WBC 19.7. Basic metabolic panel is normal. Her fibrinogen is low at 98 (normal >150). A stat CT of the abdomen shows a very large subcapsular hematoma in the right lobe of the liver, with mass effect on the liver. There is no free blood seen in the peritoneum. What do you recommend?
a) Urgent surgical exploration with packing
b) Urgent angiography with hepatic artery embolization
c) Watchful waiting with close monitoring of labs and vitals
d) Correction of coagulopathy and close monitoring
e) Transfer to a liver transplant center for urgent evaluation for liver transplant
Answer: D
This patient has HELLP ( hemolysis, elevated liver enzymes, low platelets) syndrome, which occurs in 10-20% of women with pre-eclampsia. Life-threatening complications of the HELLP syndrome with hepatic hemorrhage, rupture, or infarction can occur in up to 45% of women with HELLP. This has a very high mortality, and often times requires surgical or angiographic intervention.
However, this patient has a contained hematoma under the capsule of the liver and has stable vital signs at this time. In these patients it is recommended to correct their coagulopathy aggressively, give prophylactic antibiotics, and transfuse as required.
If there is any evidence of hemodynamic instability, then urgent angiography or surgical intervention is warranted.
Occasionally these patients may develop liver failure and and require consideration for liver transplant.
A 63 year old Caucasian male is referred to you for chronic HCV which was identified during birth cohort screening. His physical examination is normal. He has HCV genotype 1A, HCV RNA Log 6.1 IU/ml. HB surface antigen negative, anti-HB core positive, anti-HB surface positive. A liver ultrasound suggests the liver is echogenic and nodular. AST 92, ALT 89, TBILI 0.5 mg/dl, Albumin 4.1 mg/dl and platelet count 125. A Fibrosure is 0.95. You have ordered a direct acting antiviral (DAA) to treat the HCV.How would you monitor this patient for HBV reactivation?
a) no monitoring for HBV needed
b) initiate HBV treatment and continue this life long
c) initiate HBV treatment and stop this 3 months after HCV treatment is completed
d) check HBV DNA 3 months after HCV treatment is completed
Answer: A
Patients who are co-infected with HBV and HCV have a risk of HBV reactivation when HCV is treated with anti-viral therapy. As a result, the FDA has recommended that all patients with HCV have HBV serology assessed prior to initiating HCV treatment with a DAA. This should include not just HB surface antigen but also anti-HB core and anti-HB surface. Patients who are HB surface antigen positive should then be assessed with E-antigen and HBV DNA to determine if they have active HBV and require treatment or have inactive HBV and require prophylaxis during HCV treatment.
The risk of HBV flare in patients with isolated anti-HB core is very low and these can just be monitored monthly during HCV treatment and for several months after treatment has been completed to make sure HBV does not flare. Patients with protective anti-HB surface antibody have resolved HBV infection and are not at risk for HBV flare. These patients do not require any monitoring.
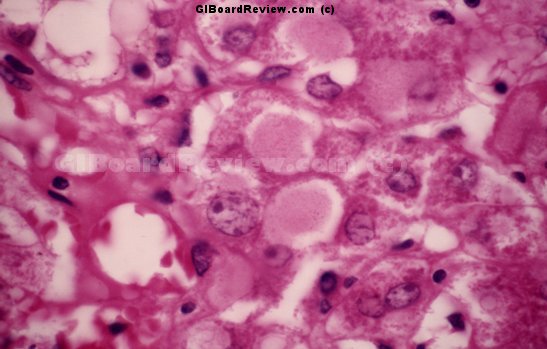
This patient was endoscoped for epigastric discomfort. He is taking daily omeprazole 20 mg. Biopsies were obtained of the distal esophagus and are shown:
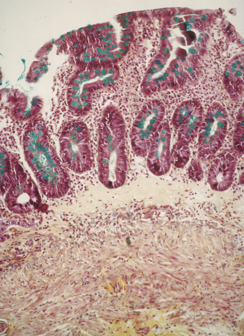
The next best step is:
a) assure the patient that there is nothing to worry about and continue current therapy
b) recommend regular endoscopic surveillance
c) refer for radiofrequency ablation (RFA)
d) increase the dose of omeprazole to 40 mg BID
Answer: B
The biopsy show's Barrett's esophagus with mucus cells (stained with Alcian Blue). All GI societies recommend continued endoscopic surveillance. RFA is not recommended for Barrett's without dysplasia and there is no agreed upon dose of PPI's for continued therapy.
A 38-year-old woman undergoes resection of the entire ileum and all but 50 cm of her jejunum after penetrating trauma causes severe damage to the superior mesenteric artery with resulting mesenteric ischemia and necrosis.
She remains total parenteral nutrition (TPN) and enteral hydration-dependent despite all medical therapies available, including teduglutide.
She has been admitted to the hospital 3 times in the past year with sepsis, twice related to bacteremia and once related to fungemia.
On examination, she is thin with body mass index (BMI) of 18 kg/m2.
She is mildly jaundiced.
Her abdomen is scaphoid, soft, and nontender to palpation.
Laboratory analysis reveals anemia as demonstrated below in Figure 1.
The patient asks whether she should be referred to a transplantation center to consider intestinal transplantation.

What is your answer?
a) Yes, because she experienced severe complications of TPN
b) Yes, because of her elevated bilirubin
c) Yes, because of her low BMI
d) No, because she has a contraindication to intestinal transplantation
e) No, because she does not have an indication for intestinal transplantation
This patient meets criteria for placement on waitlist for intestinal transplantation because she is TPN-dependent and has experienced severe complications of TPN in the form of multiple episodes of sepsis, including fungal.
Her BMI is low but not extremely so, and her bilirubin is elevated but is below the 4.5 mg/dL cutoff recommended in a 2019 consensus statement.
She does not currently have a contraindication to transplantation.
A 63 year old female with cirrhosis has developed refractory ascites requiring weekly large volume paracentesis. Her labs show a serum creatinine of 1.8, INR 1.7, and total bilirubin 3.7 (MELD 23). Your next recommendation should be:
a) Liver transplant evaluation (OLT)
b) TIPS
c) midodrine + octreotide
d) Peritoneovenous (PV) shunt placement
The patient has refractory ascites, azotemia, and high MELD. Clearly, she needs to be evaluated for OLT urgently. A TIPS must be used with caution if MELD is > 18 due to the risk of liver failure and death. Diuretics must be stopped when the serum sodium drops to < roughly 125 mEq/L, or in the setting of significant azotemia. Midodrine and octreotide might improve the azotemia transiently, but are not likely to improve this patient's prognosis without a liver transplant. PV shunts are only used for palliative care, not in those who will come to OLT in the near future.
You are referred a 28 year old Syrian female who is in the 30th week of her first pregnancy. She recently arrived in the USA and has no pre-natal care until 1 week ago. Testing by her OB demonstrated that she is HB surface antigen positive, anti-HCV positive and anti-HIV negative. The liver transaminases are normal. The ALP is 250 IU/ml. You obtain the following tests: anti-HB core positive, anti-HB surface negative, HB E antigen negative, anti-HBE positive. HBV DNA 8,420 IU/ml. HCV RNA Log 6.1 IU/ml. Genotype 4. Which of the following would you recommend?
a) initiate HBV treatment with tenofovir or entecavir now
b) obtain an MRCP
c) treat HCV now with a direct acting antiviral (DAA)
d) treat HCV 3 months after the baby is born
Answer: D
Transmission of HBV to the baby at or after birth is directly related to the serum level of HBV DNA in the mother. An HBV DNA level of greater than 200,000 IU/ml is associated with an increased risk of infection despite vaccination of the newborn at birth. Several studies have now demonstrated that treatment of HBV DNA during the third trimester of pregnancy and through the first month after birth will essentially eliminate the risk of HBV vertical transmission to the newborn. In women with an HBV DNA level under 200,000 IU/ml the rate of vertical transmission is exceedingly low with just administration of HBIG and vaccine within 12 hours of birth. In this case, the level of HBV DNA is far below 200,000 IU and so it is not necessary to treat with an antiviral agent.
The risk of HCV vertical transmission is very low especially in the absence of HIV-coinfection. Anti-viral therapy against HCV is not indicated in women with HCV infection during pregnancy. It would be recommended to treat the mother for HCV after delivery of the baby.
An ultrasound to screen the liver for HCV demonstrated no dilated bile ducts and no liver mass. There is no reason to perform an MRI in this situation.
A 46 year old man is admitted to the hospital after being found unconscious by his family. He is known to consume more than a fifth of vodka in addition to 6-12 cans of beer for at least two decades. Physical examination reveals no fever. Tender hepatomegaly and splenomegaly are present. Laboratory tests reveal a serum bilirubin of 3 mg/dl, albumin 3 gm/dl. AST 5,550 IU/L, ALT 1210 IU/L, Alk phos 155 IU/L, INR 1.5, and serum creatinine 2.1 mg/dl. There is no leukocytosis. The next appropriate test for this patient is:
a) doppler ultrasound of the liver
b) liver biopsy
c) acetaminophen level
d) blood cultures
The patient is likely to have acetaminophen toxicity. The isolated very high AST and AST:ALT ratio is out of proportion to that seen in patients with alcoholic hepatitis where levels are typically < 250-300. If transaminase elevations are greater than 250-300 in the setting of alcohol, a second source of liver injury should be sought. Ultrasound and liver biopsy would not provide diagnostic certainty. In the absence of fever and leukocytosis blood cultures are unlikely to be helpful.
This patient presented with dysphagia. Which one of the high resolution manometries pictured below would best predict a good response to a Heller myotomy?
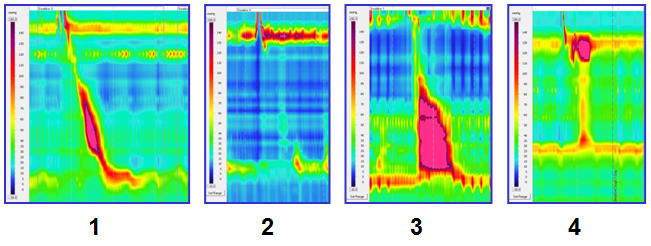
a) figure 1
b) figure 2
c) figure 3
d) figure 4
Answer: D
A Heller myotomy is a surgical treatment for achalasia. Figure 1 shows normal peristalsis and normal LES relaxation. Figure 2 shows complete aperistalsis, with a swallow followed by no esophageal activity except for LES relaxation. Figure 3 shows type III achalasia with absent LES relaxation and esophageal spasm. Figure 4 shows type II achalasia with absent LES relaxation and panesophageal pressurization with swallowing. Among the three types of achalasia that can be recognized by high-resolution esophageal manometry, type II is the one with the most consistent good response to treatment.
This 22 year old HIV infected man has severe diarrhea and weight loss. He has had problems with herpes simplex virus infections in the past. He recently returned from a trip to Egypt. Colonic biopsy shows this finding. He should be treated with which drug:
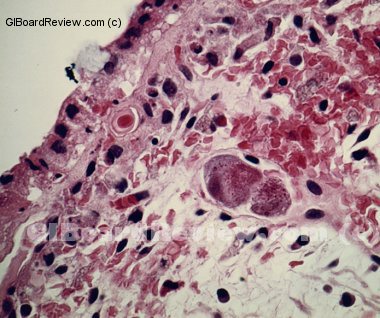
a) acyclovir
b) praziquantel
c) gancyclovir
d) ivermectin
Answer: C
The patient has CMV colitis. Hallmark histological feature is a large intranuclear inclusion which is densely eosinophilic.
The treatment for this gancyclovir. Acyclovir treats herpes, praziquantel treats schistomiasis and ivermectin treats strongyloidiasis.
A 45-year-old woman with alcohol-related cirrhosis received a living donor transplant from her sister.
Her surgery was without immediate complication.
She remains intubated in the intensive care unit and laboratory test results are trended after the surgery.
They are shown below in Figure 1.

What is the best next step in treatment of these abnormal liver enzymes?
a) abdominal US to assess biliary anastomosis stricture
b) doppler US to assess hepatic artery
c) liver biopsy to rule out CMV hepatitis
d) nuclear medicine study to assess for biliary leak
e) pulse steroids to treat acute cellular rejection
Hepatic artery thrombosis is a complication that can present acutely and early after transplantation and requires detection with doppler ultrasound when suspected. There are some patients who require surgical repair when this is discovered. Liver biopsy may be appropriate but assessing for hepatic artery thrombosis should be done first.
The possibility of acute cellular rejection is possible; however, a biopsy would be indicated before starting pulse steroids.
A biliary leak is possible after an operation, but her laboratory test results would likely be more cholestatic in nature.
Biliary strictures do not occur after transplantation so acutely so abdominal ultrasound to assess biliary anastomosis stricture is incorrect.
A 36-year-old woman who is 32 weeks pregnant presents to the community hospital emergency department with jaundice and confusion.
She has no significant past medical history, and her husband reports that she was in her usual state of health until the day before, when she noticed that she was unusually thirsty and urinating more than usual.
She was disoriented when she woke up on the day of admission, and her husband noticed that her eyes looked a little yellow.
Laboratory evaluation in the emergency department is shown below. Liver ultrasound shows a bright liver with no signs of hemorrhage.
After the infant is emergently delivered, the woman is noted to remain lethargic and confused and international normalized ratio is now 2.1.
What is the next step?
a) administer lactulose orally
b) administer lactulose rectally
c) transfer to a liver transplant center
d) transfuse fresh frozen plasma
e) transfuse cryoprecipitate
Her presentation is consistent with acute fatty liver of pregnancy, and she meets criteria for acute liver failure.
Therefore, in addition to delivery of the fetus, evaluation for liver transplantation should be pursued.
Lactulose, whether given orally or rectally, may help to reduce ammonia levels but is not definitive treatment for acute liver failure.
Fresh frozen plasma should be given in acute liver failure only in the setting of active bleeding or a planned invasive procedure.
Cryoprecipitate helps to improve fibrinogen levels but is not definitive treatment for acute liver failure.
The patient with this liver biopsy showing "ground glass" hepatocytes should be treated with:
a) Sofosbuvir/ledipasvir
b) ursodiol
c) entecavir
d) prednisone and azathioprine
Ground glass hepatocytes are liver cells with a significantly increased smooth endoplasmic reticulum producing large quantities of hepatitis B surface antigen. This is typically seen with very active hepatitis B and is not typically seen with hepatitis C. This biopsy is strongly suggestive of chronic hepatitis B and therefore entecavir is the correct answer. Ursodiol would be used for primary biliary cholangitis and prednisone and azathioprine for autoimmune hepatitis neither of which are present on biopsy.
A 48 year-old woman with a history of 4 years of dysphagia and frequent episodes of squeezing substernal chest pain that have resulted in numerous visits to emergency rooms has a normal coronary angiogram. Past medical history is unremarkable, and she takes no medications. Her high-resolution esophageal manometry tracing is shown below ( IRP= integrated relaxation pressure). Which of the following is the best therapeutic option:
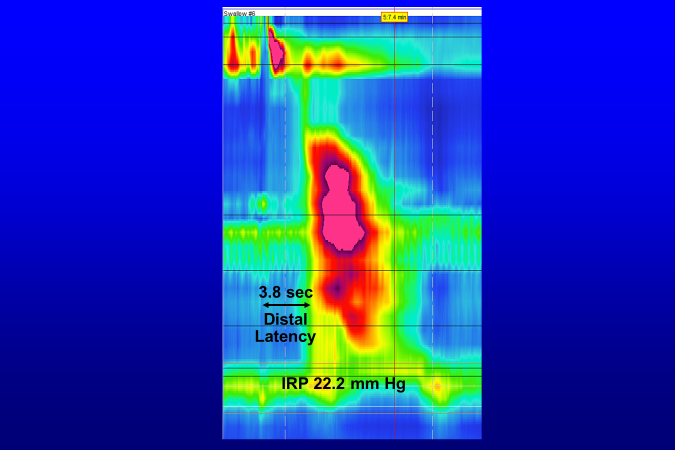 a) Botulinum toxin injectin of the LES
a) Botulinum toxin injectin of the LES
b) Laparoscopic Heller myotomy
c) Pneumatic dilation
d) Per-oral endoscopic myotomy (POEM)
Answer: D
The high-resolution esophageal motility study shows findings of Type III (spastic) achalasia with an elevated IRP (>15 mm Hg) and a short distal latency (<4.5 seconds). Her symptoms of dysphagia and chest pain are entirely consistent with the diagnosis of Type III achalasia. Botulinum toxin injection is used primarily to treat patients who are not candidates for more definitive therapy. Type III achalasia often does not respond well to pneumatic dilation or laparoscopic Heller myotomy. Furthermore, the manometry shows evidence of a long segment of hypercontractile esophagus, suggesting that a longer myotomy than that provided by pneumatic dilation or laparoscopic Heller myotomy might be preferable. POEM is now regarded as the treatment of choice for Type III achalasia.
A 70 year old woman is referred from the emergency room after a CT scan performed for possible renal stone identifies a pancreatic cyst. The patient has no current GI complaints, no weight loss, and feels otherwise well. Her physical examination is normal. Laboratory testing, including liver chemistries, amylase, and CA 19-9 are normal. You review the CT scan which notes a 5 cm cyst in the body of the pancreas. The cyst has multiple small microcystic components, and a central scar. The pancreas appears otherwise normal. What is the best management for this lesion?
a) Surgical removal
b) Evaluate yearly with EUS
c) Observation. No interventions are needed
d) MRCP yearly and if enlarging send for surgery
Correct answer: C
The appearance of a cyst with many small microcysts and a central scar is pathognomonic for a serous cystadenoma. These have minimal malignant potential, and do not require ongoing surveillance or surgery.
You are asked to see a 22 year old female from Nepal who immigrated to the USA 1 year ago. She had a persistent cough, was found to have a pulmonary lesion on CXR, had a positive Quantiferon TB Gold and started on INH 6 weeks ago. For the past 2 days she has been nauseated and vomits whenever she eats. She came to the ED and was noted to be jaundiced and mildly encephalopathic ( Grade 1). Labs: AST 322, ALT 450, TBILI 8.5 mg/dl, Albumin 3.4 mg/dl, INR 2.0, Sodium 148, Serum creatinine 1.8 mg/dl, platelets 225,000. Acute hepatitis panel was negative. A liver ultrasound was normal. What would you recommend?
a) start IV steroids
b) start IV N-acetylcysteine
c) Recommend liver transplant
d) monitor patient, no treatment necessary
The patient may be going into acute liver failure from drug induced liver injury. She has a coagulopathy and is encephalopathic and thus fulfills the definition of acute liver failure ( ALF). A randomized, placebo-controlled trial has demonstrated that N-Acetylcysteine is effective in reducing liver failure and the need for liver transplantation in patients with non-acetaminophen induced acute liver failure when started when patients have grade 1-2 encephalopathy (as opposed to grade 3-4 where the benefit was not seen).
A retrospective evaluation of corticosteroids for treatment of acute liver failure did not demonstrate any benefit. IV steroids simply increase the risk of infection and should therefore not be used for this indication.
With a normal liver ultrasound a dynamic MRI, which is highly effective in assessing liver mass lesions, would not be expected to add any new information which would help in the management of this patient.

