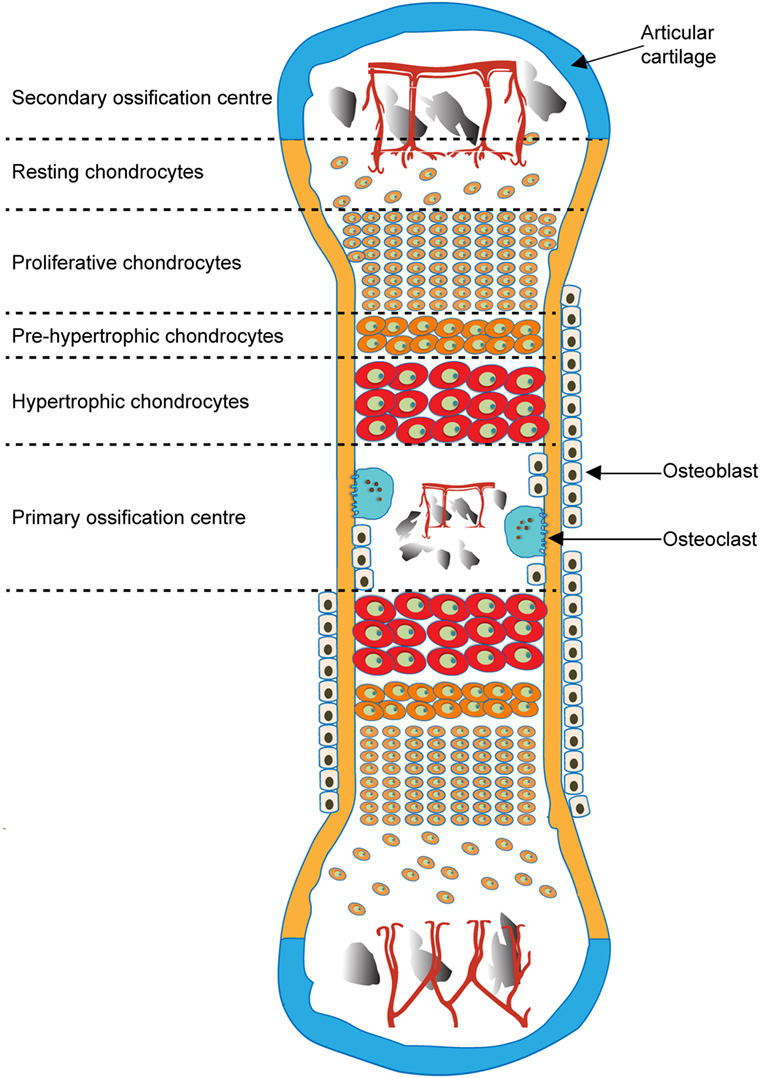
In this type of bone formation, a cartilaginous model is first made by chondrocytes. Osteoclasts and osteoblasts later replace it with woven bone and then remodel to lamellar bone.
What is endochondral ossification?

Osteoblastic activity is measured by osteocalcin, propeptides of type I procollagen, and...
What is bone ALP?
Bone alkaline phosphatase (ALP) is an ectoenzyme attached to the outer surface of the cell membrane of osteoblasts by glycosylphosphatidylinositol. It is partly released into the circulation. Bone ALP and liver ALP constitute about 95% of the total ALP activity in human serum.
Draw and explain 2 complications of OI

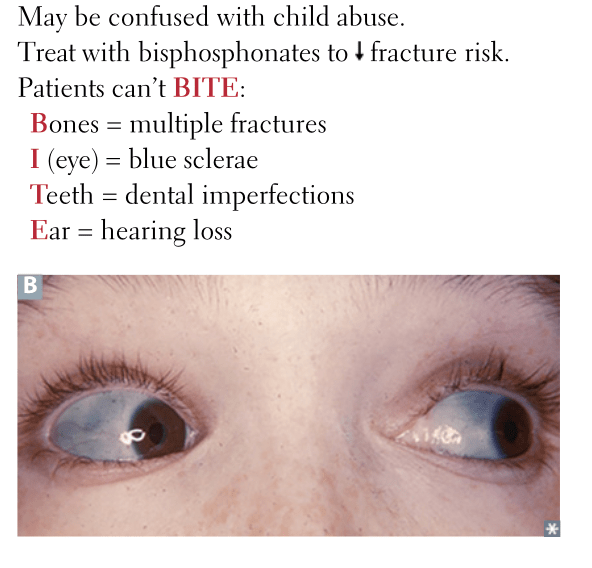
- Frequent Fractures: Individuals with OI experience frequent bone fractures, often with minimal trauma. Fractures can occur in childhood and continue into adulthood.
- Bone Deformities: Repeated fractures and abnormal bone development can lead to deformities such as bowing of long bones, scoliosis, and limb deformities.
- Growth Impairment: Children with OI may experience stunted growth and shorter stature due to frequent fractures and impaired bone development.
- Hearing Loss: Approximately 50-75% of individuals with OI may develop hearing loss due to abnormalities in the bones of the middle ear.
- Dental Problems: Many individuals with OI have dentinogenesis imperfecta, which affects the teeth, causing discoloration, increased fragility, and dental problems.
- Cardiovascular Issues: Some individuals with OI may experience cardiovascular complications, such as aortic aneurysms or valve problems.
- Respiratory Problems: Severe forms of OI can lead to respiratory complications, including restrictive lung disease due to skeletal deformities affecting lung function.
- Increased Risk of Osteosarcoma: Although rare, there is a slightly increased risk of developing osteosarcoma (bone cancer) in individuals with OI.
A T-score of less than or equal to -2.5 is needed to diagnose a patient with this disorder.
What is osteoporosis? 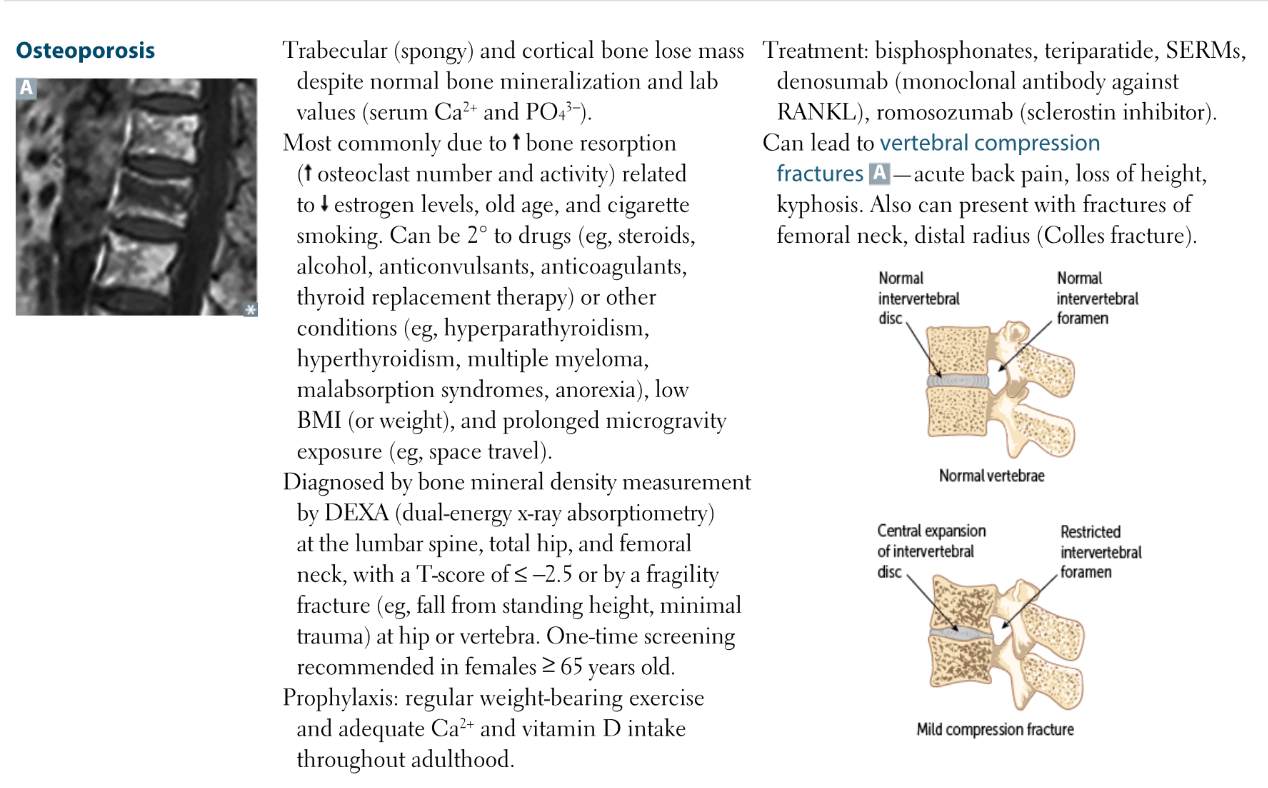
At what stage does the closure of the epiphyseal growth plates typically occur?
A) Infancy
B) Early childhood
C) Puberty
D) Adulthood
C) Puberty
Worksheet time 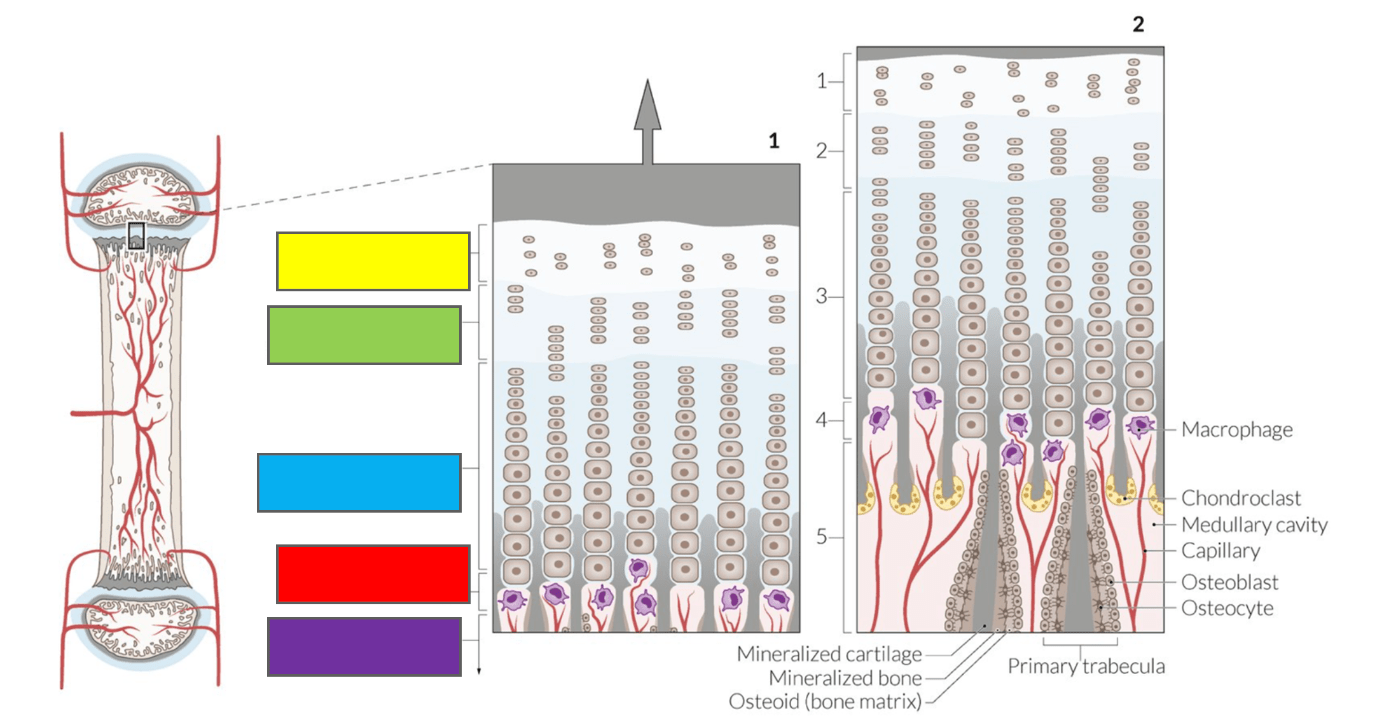
(1) The epiphyseal plate consists of four zones of continued cartilage growth (zone 1-4) and one ossification zone (zone 5).
Zone 1 contains undifferentiated, inactive precursor chondrocytes awaiting proliferation. In zone 2, the chondrocytes undergo mitosis and then enlarge via hypertrophy in zone 3. The chondrocytes are now organized in numerous longitudinal columns with transverse and longitudinal partition. Proliferation and hypertrophy results in the longitudinal growth of the cartilage, and thereby the bone. Following the hypertrophic zone, the longitudinal septa between the columns of chondrocytes are mineralized in the zone of calcified cartilage (zone 4). In zone 5, macrophages (purple) lyse the hypertrophic chondrocytes and unmineralized transverse septa, giving rise to the medullary cavity.
(2) The epiphyseal plate after continued cartilage and bone elongation:
Approx. ⅓ of the longitudinal septa of mineralized cartilage (gray) are degraded by chondroclasts (yellow). The remaining longitudinal septa are colonized by osteoblasts that deposit osteoid (light brown). The osteoid is mineralized to form bone (dark brown); the calcified columns serve as templates for the primary trabeculae of the trabecular bone. Cessation of cartilage growth and complete ossification of epiphyseal plate mark the end of longitudinal growth.
At low, intermittent levels, this hormone exerts anabolic effects on osteoblasts and osteoclasts (indirect). Chronically increased levels of this hormone cause catabolic effects (osteitis fibrosa cystica).
What is PTH?
Family history of OI increases the risk of having the condition. OI has this specific pattern of inheritance.
What is autosomal dominant?
This childhood MSK condition is a common elbow injury in children <5 years. Caused by a sudden pull on the arm, causing the immature annular ligament to slip over the head of the radius. The injured arm is held in a slightly flexed and pronated position. Hint: also called nursemaid's elbow.

What is radial head subluxation? 
Social support plays a crucial role in managing osteogenesis imperfecta (OI) and enhancing the quality of life for individuals with this condition. Describe some of the various forms of social support that could be beneficial for a patient like Matthew and his parents.
1. Emotional support (support groups)
2. Educational support (working with teachers and school administrators to accommodate physical needs, ensure safety, and provide appropriate learning environments)
3. Medical and professional support (multidisciplinary team-PT, genetic counselor, therapists, etc.)
4. Financial support (insurance, financial assistance, charities and foundations - OI Foundation)
5. Social services (counseling, community resources)
6. Peer Support (mentorship and social networks)
7. Advocacy and Awareness
8. Practical Support (assistive devices and home care)
9. Community Integration (foster inclusion and social engagement, making public spaces more accessible)
Which hormone is primarily responsible for regulating bone growth during childhood?
A) Cortisol
B) Thyroxine
C) Parathyroid hormone
D) Growth hormone
D) Growth hormone
Deficiency of this compound can lead to impaired metabolism of calcium and phosphate. Hint: pictured below is the consequence of having this deficiency in children. 
What is Vitamin D?
Which of the following statements about the epidemiology of osteogenesis imperfecta (OI) is correct?
A) Osteogenesis imperfecta affects approximately 1 in 1,000 live births and is more common in females.
B) Osteogenesis imperfecta is a rare genetic disorder occurring in approximately 1 in 15,000 to 1 in 20,000 live births, with an equal prevalence across genders and ethnic groups.
C) The prevalence of osteogenesis imperfecta significantly varies by ethnicity, with higher rates observed in certain ethnic groups.
D) Osteogenesis imperfecta is commonly inherited in an autosomal recessive pattern, making it rare in individuals with no family history of the disorder.
B) Osteogenesis imperfecta is a rare genetic disorder occurring in approximately 1 in 15,000 to 1 in 20,000 live births, with an equal prevalence across genders.

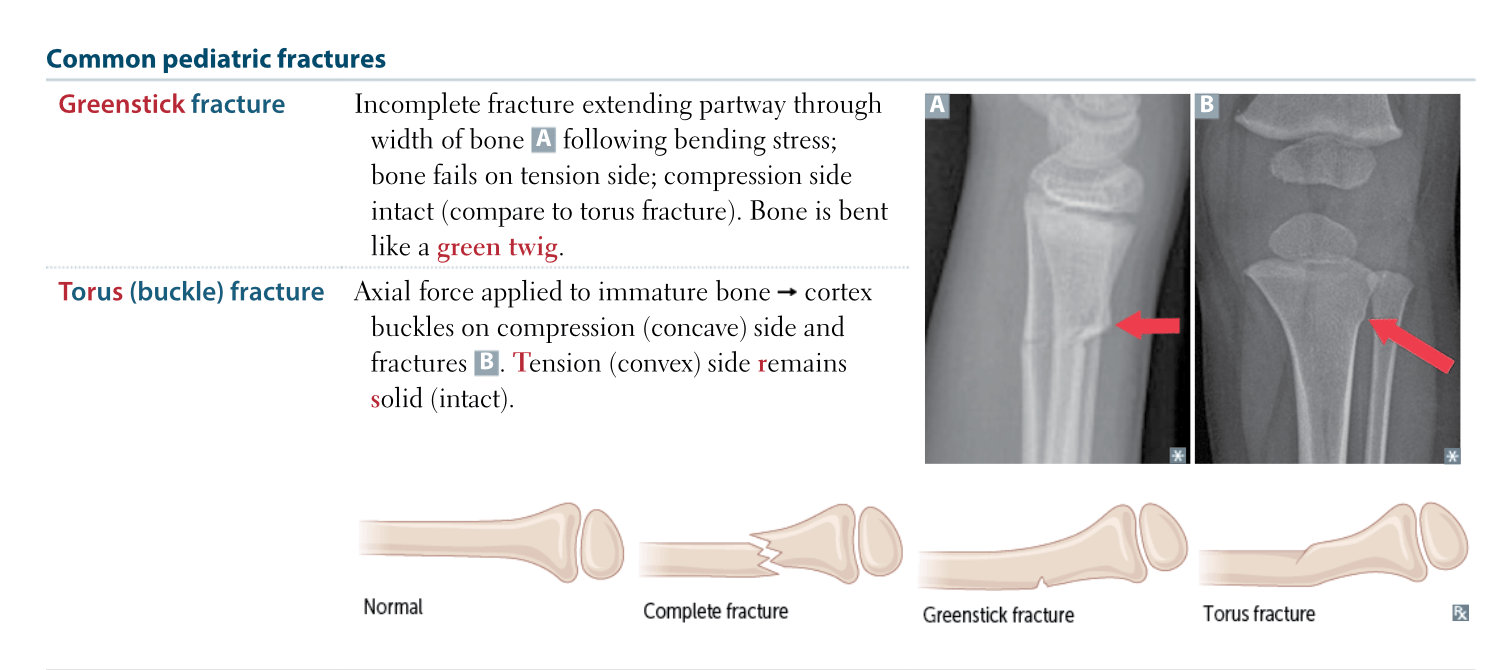
Pick a card labeling a common pediatric fracture. Describe the appearance, cause, and treatment of each fracture.
Complete Fracture
- Description: A complete fracture, also known as a simple or transverse fracture, is a type of bone fracture where the break extends across the entire width of the bone, resulting in two distinct bone fragments.
- Appearance: The bone is completely broken into two or more separate pieces. The fracture line completely traverses the bone, separating it into distinct segments.
- Cause: Typically caused by a significant trauma or force, such as a fall or a car accident. It can also occur from repeated stress or overuse.
- Symptoms: Severe pain, swelling, deformity, and inability to move the affected limb. The ends of the bone may be visible or palpable.
- Treatment: Often requires realignment (reduction) and immobilization with a cast or splint. In some cases, surgical intervention with pins, plates, or screws may be necessary.
2. Greenstick Fracture
- Description: A greenstick fracture is an incomplete fracture where the bone bends and cracks on one side but does not break all the way through. It is similar to bending a green twig until it breaks partially.
- Appearance: The fracture is partial and typically occurs on one side of the bone, causing a bend and a crack on the other side. The bone does not break into separate pieces.
- Cause: Commonly seen in children due to their softer, more pliable bones. It usually results from a fall or trauma.
- Symptoms: Pain, swelling, and tenderness at the fracture site. The bone may appear bent or deformed, but the break is not complete.
- Treatment: Often treated with immobilization in a cast or splint to allow the bone to heal properly. Because the fracture does not completely break through, healing is usually straightforward.
3. Torus Fracture (Buckle Fracture)
- Description: A torus fracture, also known as a buckle fracture, is a type of incomplete fracture where the bone bulges outwards on one side due to compressive forces, creating a “buckle” or “puffed” appearance.
- Appearance: The bone is compressed and bulges outward rather than breaking completely. There is no clear fracture line across the bone; instead, the bone appears to have a localized area of deformation.
- Cause: Common in children and often results from minor trauma or falls, particularly when the bone is soft and still developing.
- Symptoms: Pain, tenderness, and swelling at the site of the bulge. The affected area may appear swollen or deformed without a clear fracture line.
- Treatment: Generally treated with immobilization using a cast or splint. Healing is usually quick, and there is often a good prognosis for complete recovery.
Summary
- Complete Fracture: Bone is broken all the way through, resulting in separate fragments. Requires significant force and often surgical intervention.
- Greenstick Fracture: Partial break with bending, more common in children due to flexible bones. Treated with casting.
- Torus Fracture: Incomplete fracture with bulging or buckling of the bone surface, commonly seen in children. Typically heals with immobilization.
In this histological slide of a finger joint, which zone represents the zone of hypertrophic cartilage?
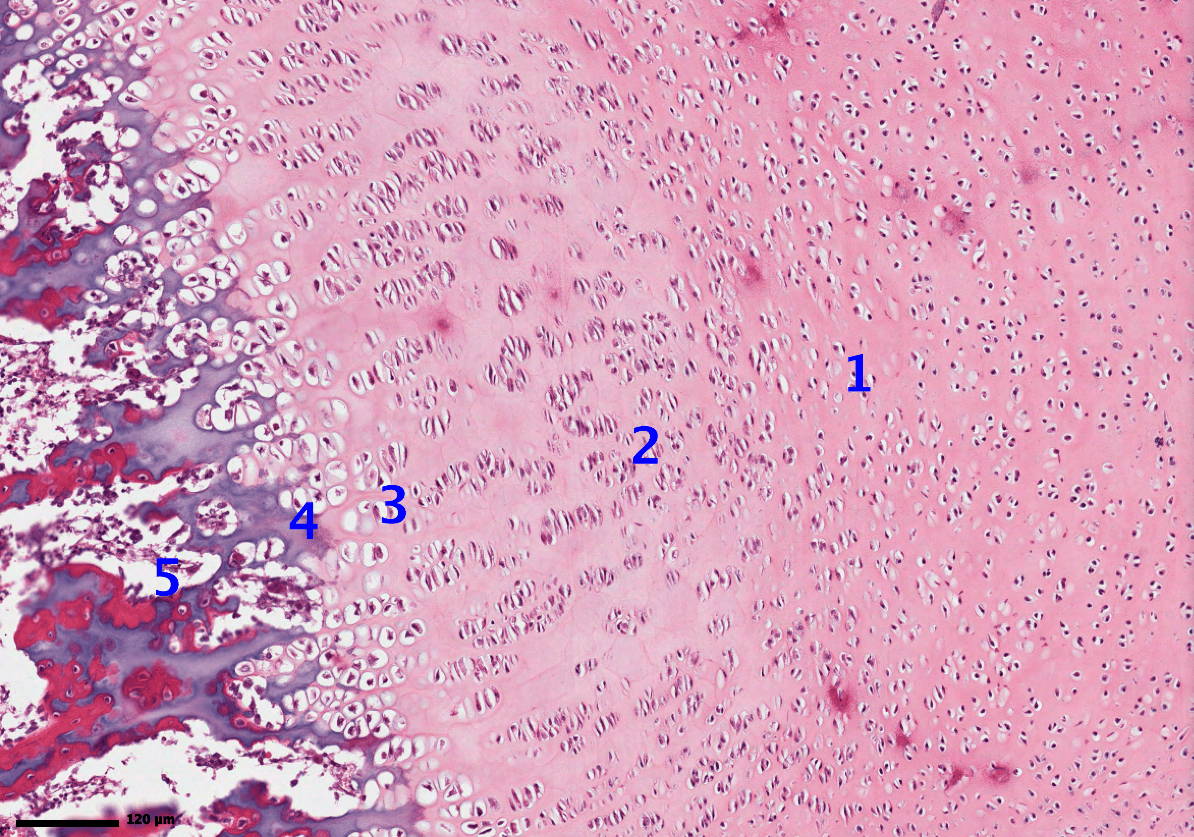
Zone 4

The bones colored in blue are formed by this method of bone formation.
What is membranous ossification?
Bones of the calvarium, facial bones, and clavicle are formed by this method. Woven bone formed directly without cartilage. Later remodeled to lamellar bone.
In weeks 6-7 of fetal development, people with osteogenesis imperfecta have a defect in the formation of this critical component of bone. This makes bones inherently fragile and prone to fracture even before birth.
What is type I collagen?
Name three treatment options/therapeutics for OI

- Therapy
- No definitive treatment available
- Supportive measures: walking aids, wheelchairs, devices to improve patient's mobility and function
- Bisphosphonates: increase cortical thickness and decrease the risk of fractures
- Surgery: to improve mobility and correct the associated skeletal defects
In this most common form of skeletal dysplasia, a mutation in the FGFR3 gene leads to a defective cartiliage-to-bone conversion at growth plates (defective endochondral ossification). The x-ray on the right has a patient with mutation. Hint: Peter Dinklage has this condition.
What is achondroplasia?

A skin biopsy of a rash shows intraepidermal accumulation of edematous fluid with widening of intercellular spaces between keratinocytes. The rash is pruritic and located in the cubital fossa of the upper extremeties. Which of the following is most likely the diagnosis?
A. Psoriasis vulgaris
B. Lichen planus
C. Dermatitis herpetiformis
D. Eczematous dermatitis
D. Eczematous dermatitis

In a long bone, the formation of this particular area involves the cartilage model to slowly become vascularized through penetration of vascular buds. (Hint:this marks the beginning of bone formation during the fetal stage of development).
What is the primary ossification center?
Name the condition that can clinically present as the head CT shown below.
The diploic space of the calvarium is widened and the cortex is thickened. There are numerous ill-defined lucent and sclerotic areas (arrows), which may produce a characteristic cotton-wool appearance.
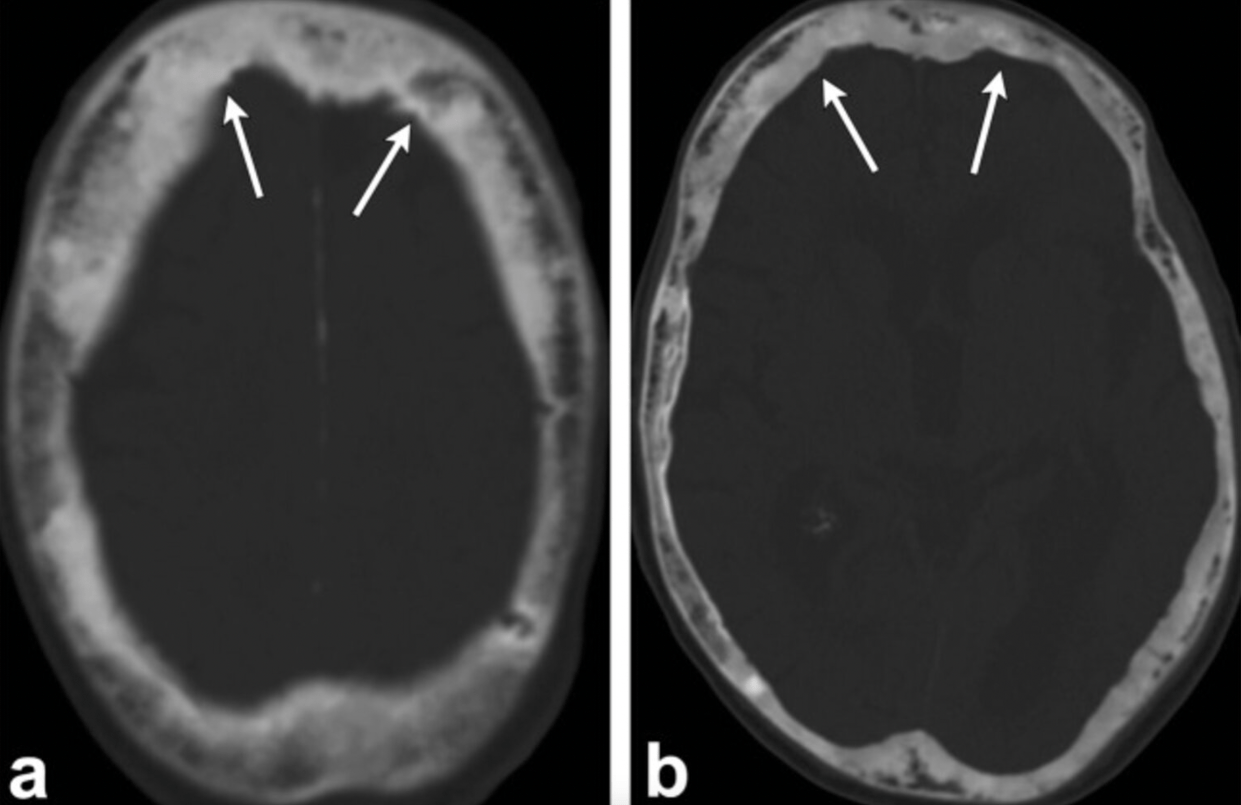
CT head (axial plane; bone window)
What is Paget's disease of bone?
Paget disease of bone (PDB, or osteitis deformans) is a slowly progressive skeletal disease; it can be monostotic or polyostotic. In PDB, increased bone turnover causes normal lamellar bone to be replaced by weak woven bone. PDB is common but underdiagnosed, and its etiology is not known.
Which of the following genes is most commonly associated with osteogenesis imperfecta?
A) COL2A1
B) COL3A1
C) COL1A1
D) COL5A1
C) COL1A1
Osteogenesis imperfecta is primarily associated with mutations in the COL1A1 and COL1A2 genes, which are responsible for the production of type I collagen. The COL2A1 gene is associated with a different type of collagen and other connective tissue disorders, while COL3A1 and COL5A1 are linked to other specific conditions.
This childhood MSK condition classically presents in obese young adolescents with hip/knee pain and altered gait. Increased axial force on the femoral head displaces the epiphysis relative to the femoral neck. Diagnosed via x-ray.
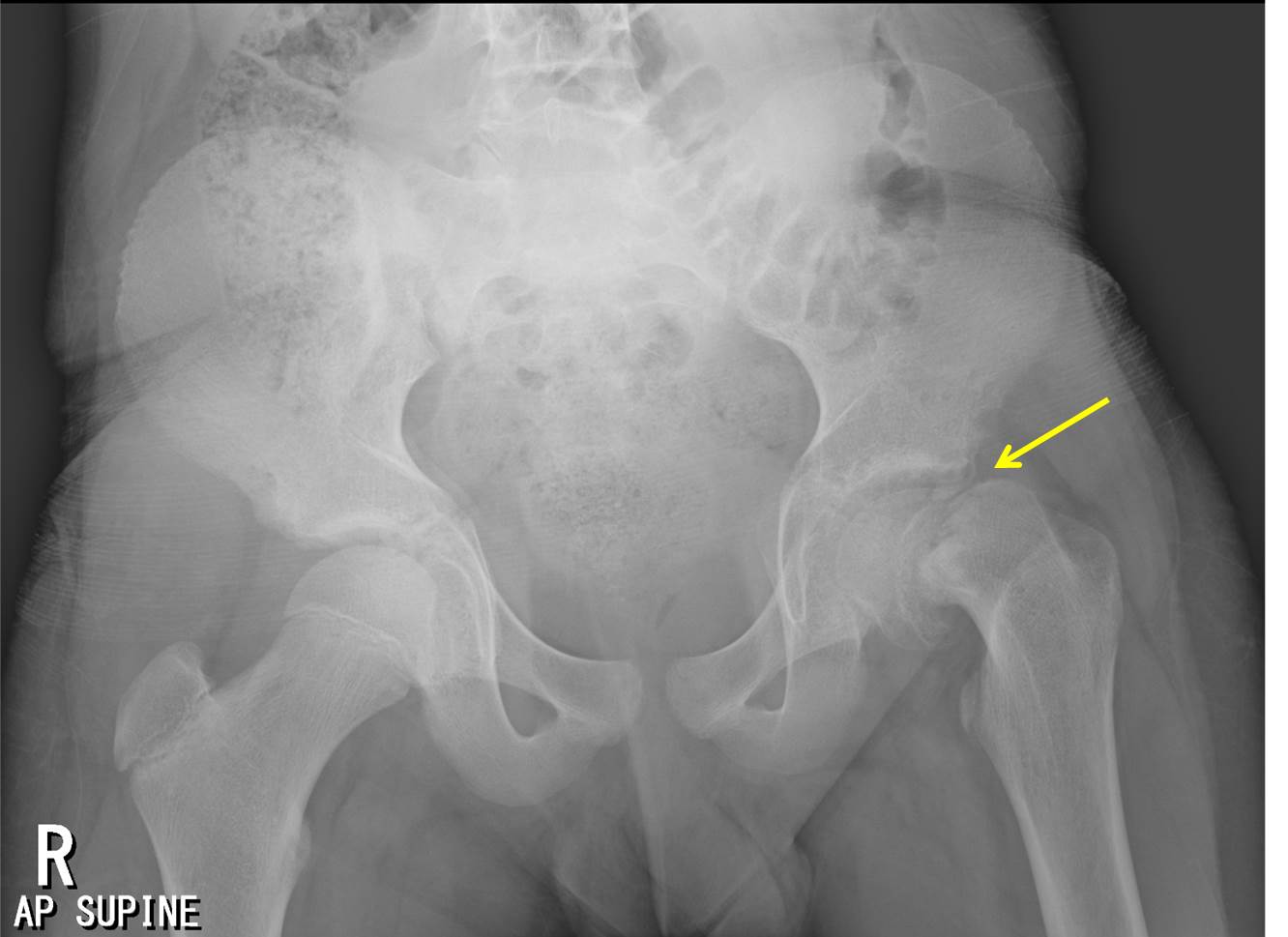
What is slipped capital femoral epiphysis? 
This condition, as seen in the picture below, is associated with several conditions. Name two of the conditions.

Condition: Acanthosis nigricans
1. Insulin resistance and type 2 diabetes
2. Obesity
3. Endocrine disorders (PCOS, Cushing's, hypothyroidism)
4. Genetic syndromes
5. Malignancies (Gastric adenocarcinoma)
6. Medication induced (high-dose niacin, corticosteroids, oral contraceptives, and certain cancer treatments (like nicotinic acid and protease inhibitors))
7. Autoimmune disorders (Lupus)