A 64-year-old right-handed man presents to the ED after suddenly developing difficulty speaking. He appears frustrated, speaks in short, broken phrases, and struggles to form full sentences. His comprehension appears intact — he follows commands and nods appropriately. Repetition is impaired. He has mild right facial droop and right arm weakness.
❓ Which of the following best describes his type of aphasia?
A) Wernicke aphasia
B) Broca aphasia
C) Conduction aphasia
D) Global aphasia
E) Transcortical motor aphasia
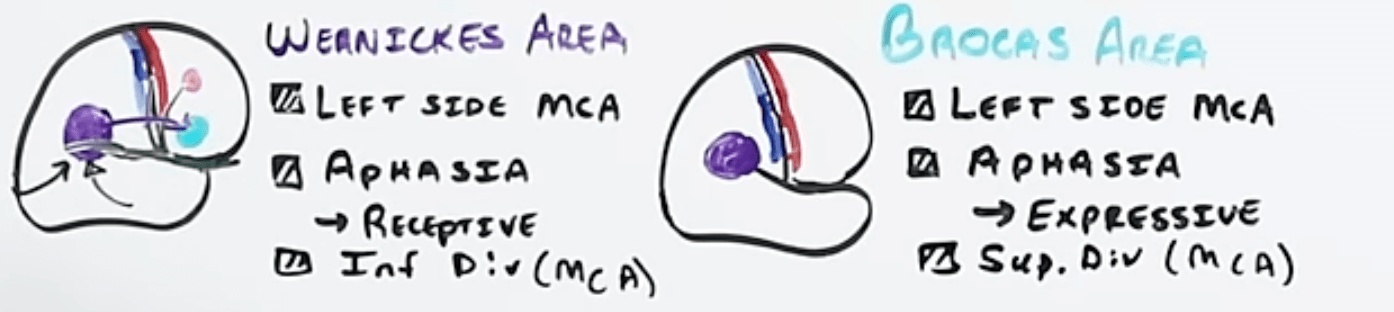
“Broca is broken speech, but they know it. Wernicke is word salad, and they don’t.”
A 40-year-old right-handed man is brought to the ED after a witnessed seizure. According to his coworker, the episode began with rhythmic twitching of his right index finger, which gradually spread to involve his entire hand, then his right arm, and eventually his right leg. He remained conscious during the initial movements but eventually became unresponsive and developed bilateral tonic-clonic activity.
Which of the following best describes the phenomenon observed in the initial phase of this seizure?
A) Myoclonic jerks
B) Todd’s paresis
C) Tonic phase of a generalized seizure
D) Jacksonian march
E) Automatism
D) Jacksonian march
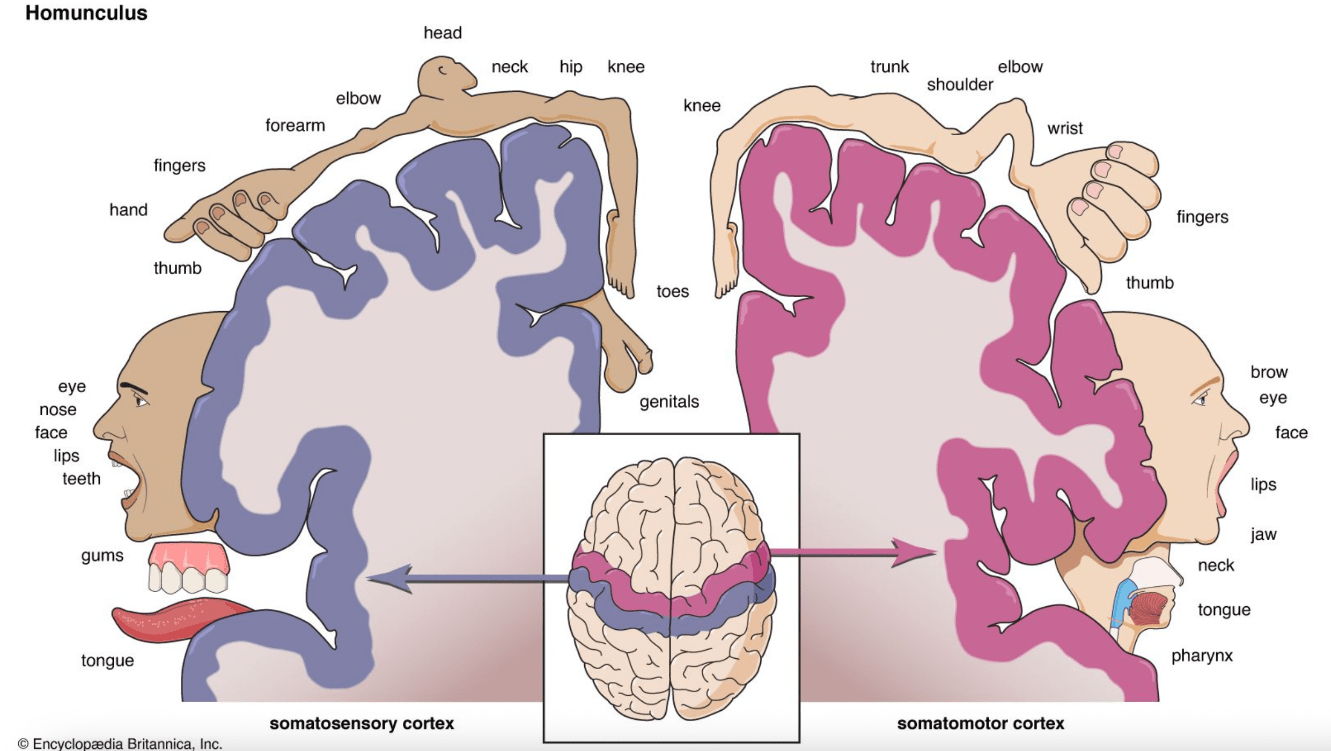
• Jacksonian march refers to the sequential spread of motor activity across body parts in a pattern that reflects the somatotopic organization of the primary motor cortex (precentral gyrus).
• The patient is often conscious during the march, and the seizure may or may not generalize.
• It is a hallmark of focal motor seizures, especially with cortical onset (e.g., frontal lobe).
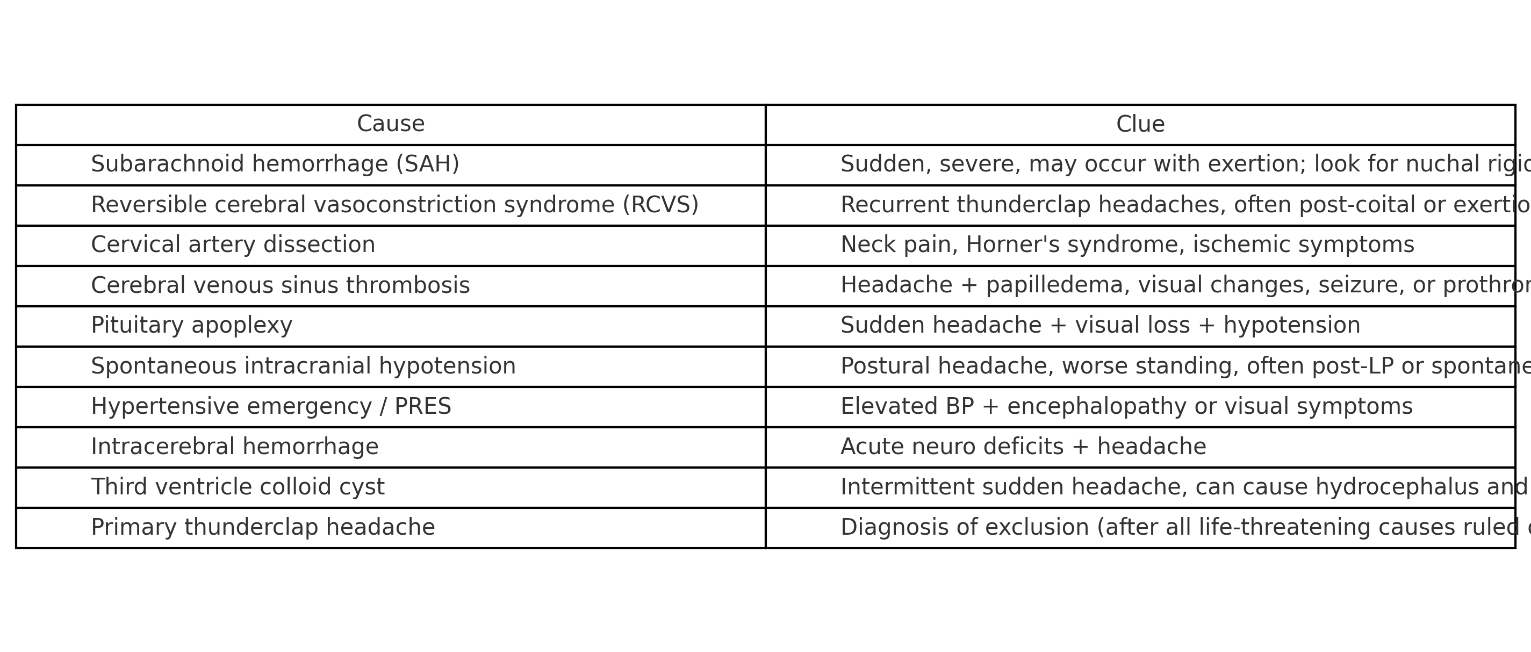
A 35-year-old previously healthy man suddenly clutches his head in the emergency department waiting room and says,
“This is the worst headache of my life!”
He’s grabbing his neck and appears photophobic. His vitals are stable, and there’s no focal neurologic deficit.
While awaiting imaging, you think to yourself:
“Aside from subarachnoid hemorrhage, what else can cause a thunderclap headache?”
🚨 Name at least 6 potential causes of thunderclap headache that should be considered in the ED before attributing it to something benign.
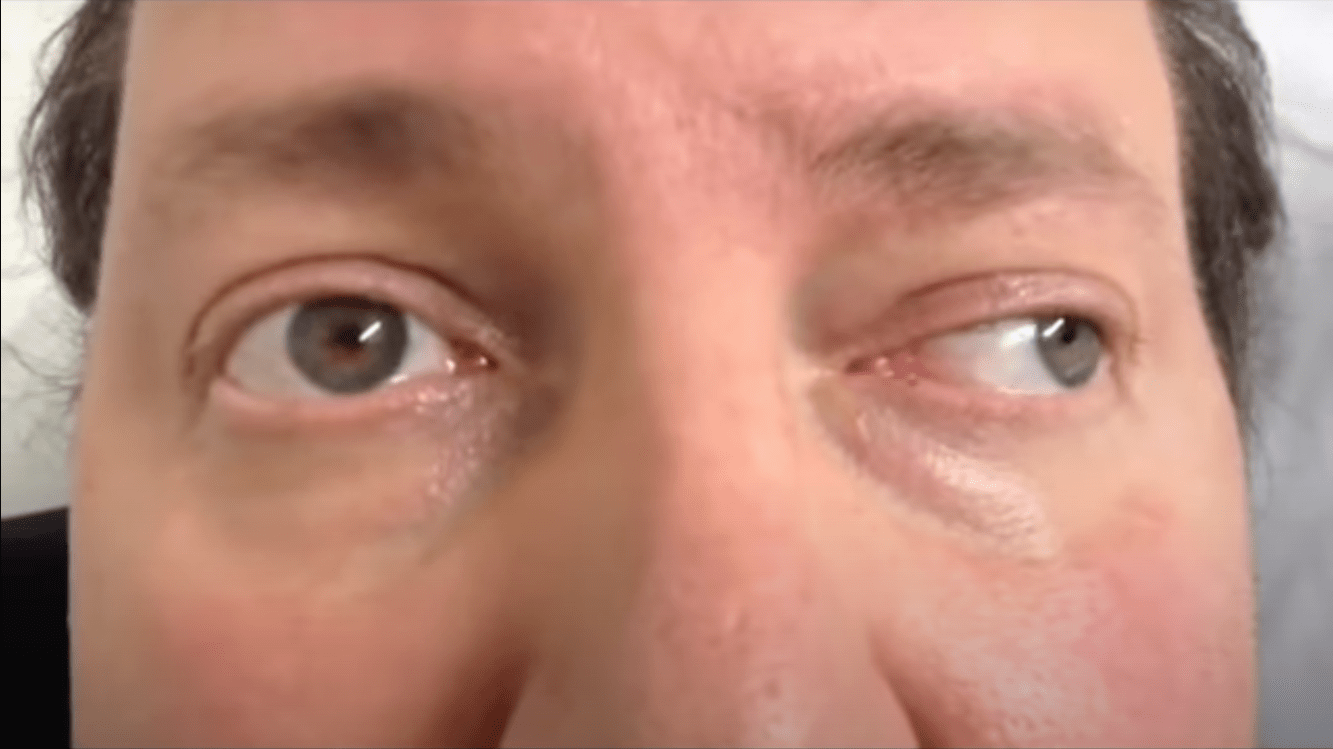

You are evaluating a 45-year-old patient with diplopia. On horizontal gaze testing, you observe the following:
• When attempting to look left, the right eye fails to adduct, while the left eye abducts with nystagmus (see image 1).
• When looking right, both eyes move appropriately (see image 2).
• There is no ptosis or pupil involvement.
❓ Which of the following is the most likely location of the lesion?
A) Right oculomotor nerve
B) Right medial longitudinal fasciculus (MLF)
C) Left abducens nerve
D) Right lateral rectus muscle
E) Left medial longitudinal fasciculus (MLF)
B) Right medial longitudinal fasciculus (MLF)
Internuclear ophthalmoplegia (INO) results from a lesion in the MLF, which connects the contralateral abducens nucleus to the ipsilateral oculomotor nucleus to coordinate conjugate horizontal gaze.
• Classic findings:
• Impaired adduction of the affected eye (on side of lesion)
• Abducting nystagmus of the contralateral eye
Bonus question: What can cause this?
• Multiple sclerosis in young adults
• Brainstem stroke in older patients
• Tumors
• Bleeds
An 84-year-old woman is brought to the ED from a nursing home with acute confusion and lethargy for the past 6 hours. She has a history of hypertension and atrial fibrillation (not on anticoagulation). Her vitals are: T 38.2°C, HR 104, BP 138/78, RR 20, SpO₂ 97% on room air. She is disoriented but opens eyes and follows simple commands. Neurologic exam reveals no focal deficits, pupils are equal and reactive, and there is no gaze preference, weakness, aphasia, or neglect. Urinalysis shows pyuria and leukocyte esterase.
A junior resident wants to send the patient for an urgent non-contrast head CT to rule out stroke.
❓Which of the following is the most appropriate response?
A) Agree — stroke often presents with confusion in the elderly and should be ruled out first
B) Defer CT — this is most likely delirium from infection; imaging is low yield without focal signs
C) Order a CT with perfusion — posterior stroke is common in the elderly and easily missed
D) Recommend MRI instead — CT is not sensitive enough to rule out early ischemia
E) Intubate and sedate the patient for MRI to avoid missing subtle stroke findings
B) Defer CT — this is most likely delirium from infection; imaging is low yield without focal signs
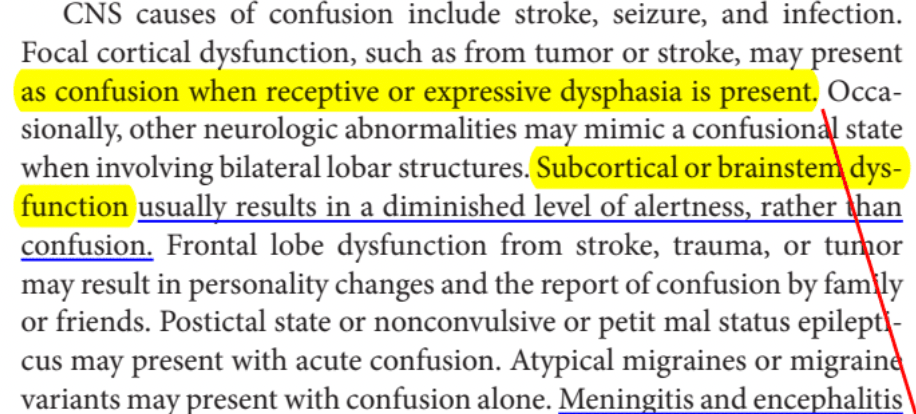
• Stroke rarely causes isolated confusion
• Delirium in the elderly is most often due to infection, drugs, metabolic issues
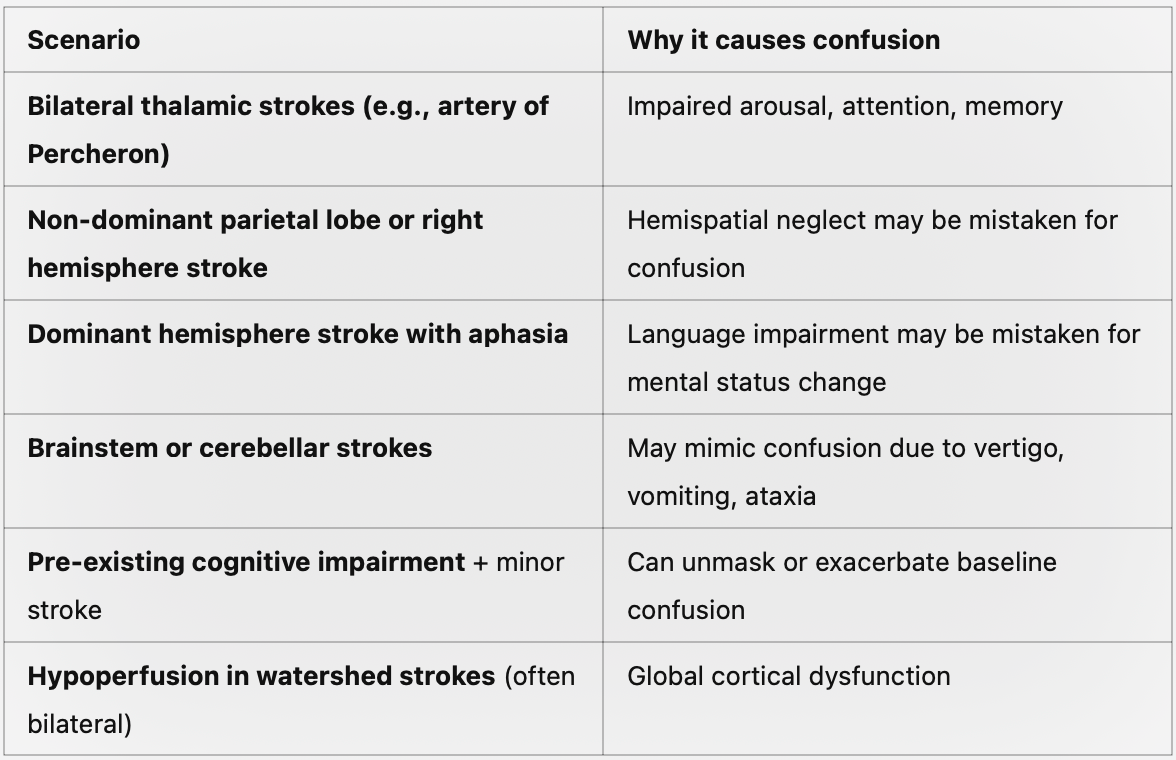
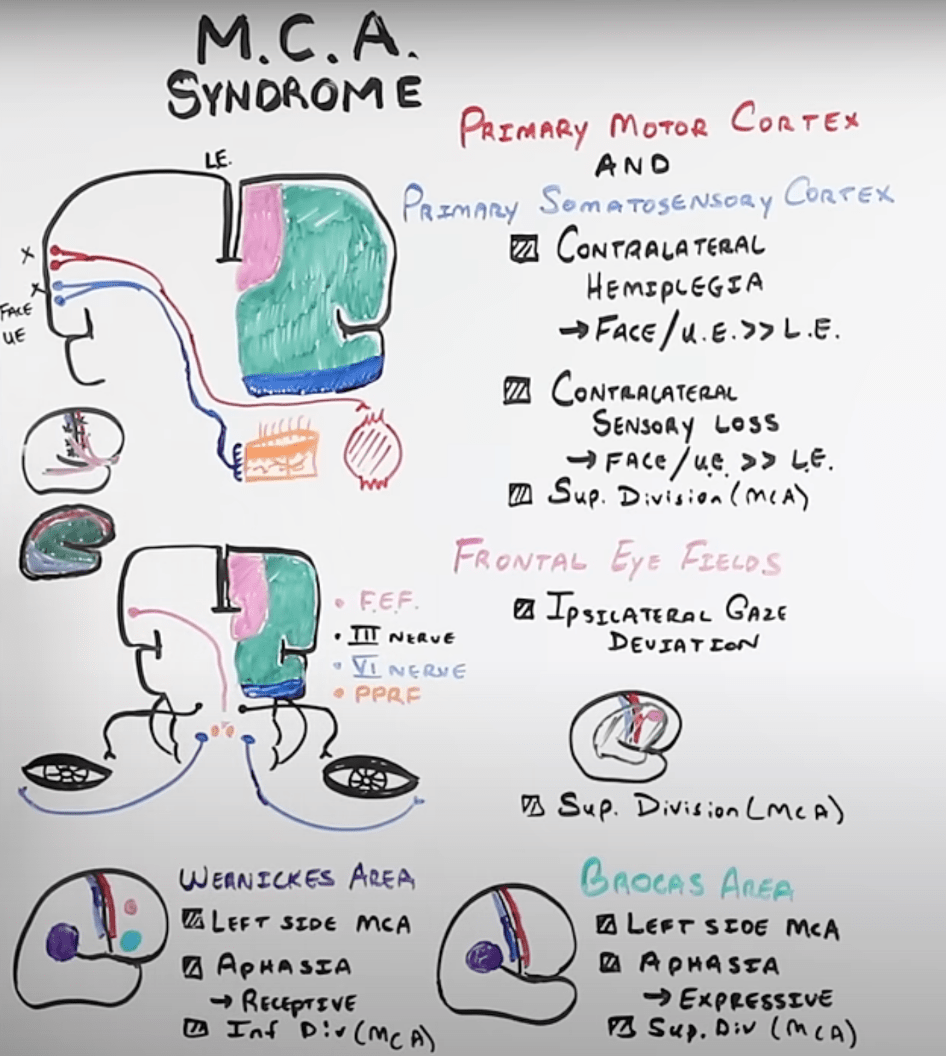
A 67-year-old right-handed man presents with sudden-onset right arm and face weakness, expressive aphasia, and right-sided visual field deficit. He also has mild right leg weakness but is able to move it against resistance. Blood pressure is 170/96 mmHg. CT head is pending.
❓ Which of the following vascular territories is most likely affected?
A) Left anterior cerebral artery (ACA)
B) Left middle cerebral artery (MCA)
C) Left internal carotid artery (ICA)
D) Right middle cerebral artery (MCA)
E) Right anterior cerebral artery (ACA)
B) Left middle cerebral artery (MCA)
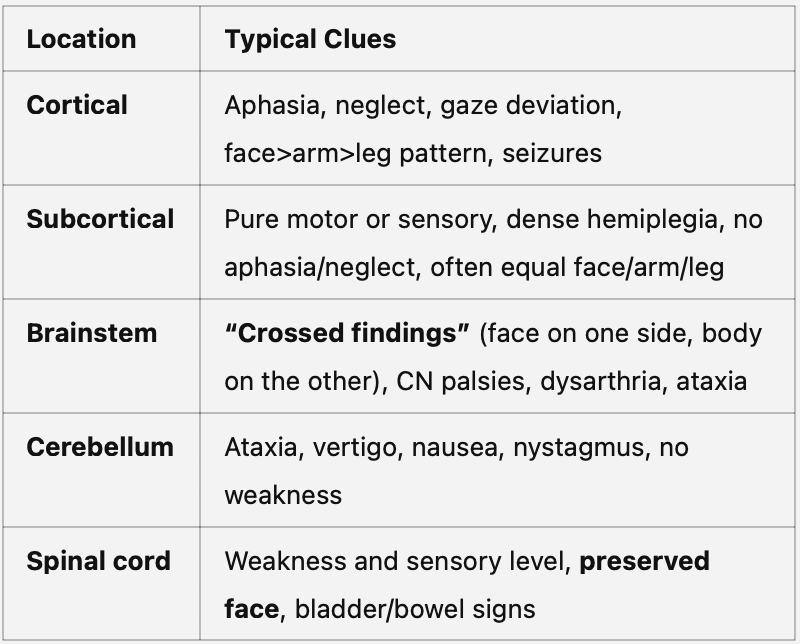
🧠 Why might subcortical strokes cause “pure” deficits?
Because subcortical regions like the internal capsule, thalamus, or corona radiata contain dense bundles of white matter tracts — not the cortical processors themselves, just the “wires” that carry signals.
Which of the following statements regarding patients presenting with first-time seizures is true?
A. All patients should have a basic electrolyte panel.
B. All patients should receive a loading dose of an anti-epileptic drug and a prescription for an oral regimen prior to discharge.
C. Non-diabetic patients do not need to have serum glucose checked if their mental status returns to normal.
D. Persistent altered mental status is an indication for a lumbar puncture
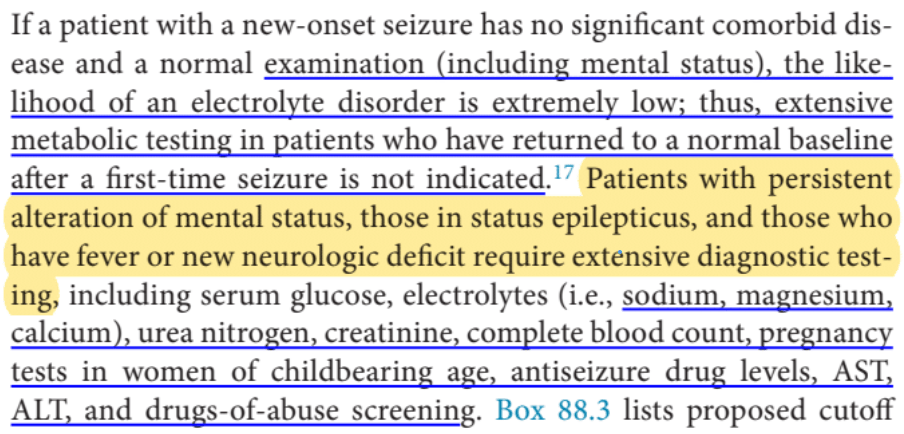
D. Persistent altered mental status is an indication for a lumbar puncture
Persistent altered mental status should trigger consideration of a lumbar puncture, serum glucose, and an electroencephalogram (EEG) among other testing.
Non-contrast CT of the head is relatively high-yield in first-time seizure patients, and most guidelines recommend performing one. Patients with no comorbidities who return to baseline mental status do not need broad-based electrolyte testing, but hypoglycemia is a com-mon cause of seizures even in nondiabetic patients and should be routinely tested for in first-time seizure patients.
A 45-year-old woman with a history of poorly controlled hypertension and lupus presents with new-onset generalized seizures and confusion. Her family reports that she had a severe headache the night before and has been more lethargic over the past 2 days. BP on arrival is 198/110 mmHg. She is disoriented but moves all extremities symmetrically. Fundoscopy reveals mild papilledema.
MRI of the brain shows symmetric T2/FLAIR hyperintensities in the bilateral parieto-occipital lobes without diffusion restriction.
Which of the following is the most likely diagnosis?
A) Acute ischemic stroke
B) Reversible cerebral vasoconstriction syndrome (RCVS)
C) Posterior reversible encephalopathy syndrome (PRES)
D) CNS vasculitis
E) Toxoplasmosis encephalitis
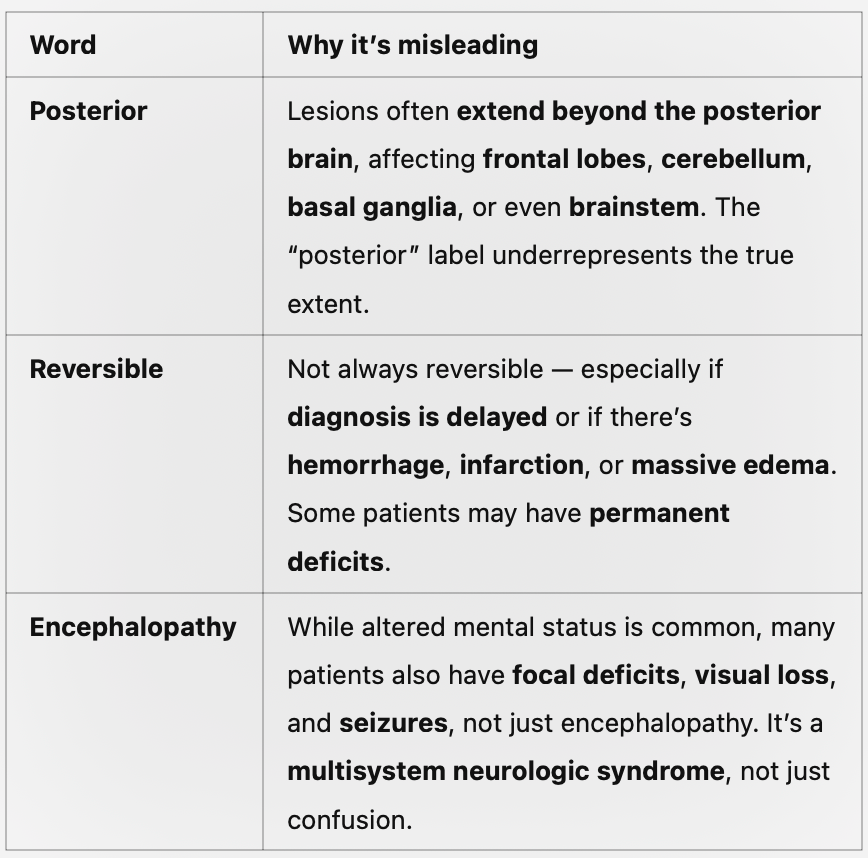
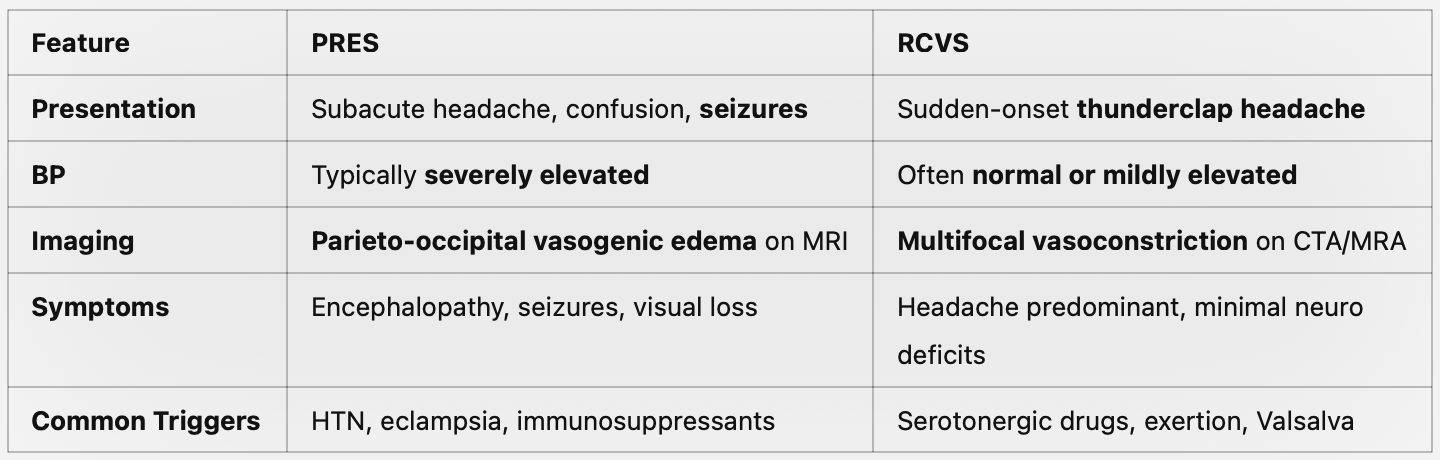
C) Posterior reversible encephalopathy syndrome (PRES)
“PRES is a misnomer — it’s not always posterior, not always reversible, and not limited to encephalopathy. Think of it as a syndrome of vasogenic edema due to failed cerebral autoregulation, often with systemic triggers like hypertension, eclampsia, or cytotoxic drugs.”
A 30-year-old woman with a 3-year history of relapsing-remitting multiple sclerosis presents to the ED with worsening left leg weakness and blurry vision over the past 24 hours. She denies any new trauma. She mentions she recently recovered from a urinary tract infection treated with antibiotics three days ago. On exam, she has mild spasticity in the left leg and decreased visual acuity in the right eye. There is no new sensory deficit and she notes she "had these exact symptoms once before".
Her vital signs are normal, but her temperature is 38.3°C (100.9°F).
What do you think would be the likely course of events?
A. Initiate IV methylprednisolone for presumed MS relapse
B. Obtain emergent MRI of brain and spine with contrast
C. Begin plasmapheresis for acute demyelination
D. Treat the fever and observe for improvement
E. Refer for inpatient rehab due to functional decline
D. Treat the fever and observe for improvement
Pseudoflare: Temporary worsening of MS symptoms triggered by fever, heat, infection, or stress—not true new demyelination.
Bonus: what do we call it when MS symptoms particularly worsen with heat?
(Uhthoff phenomenon)
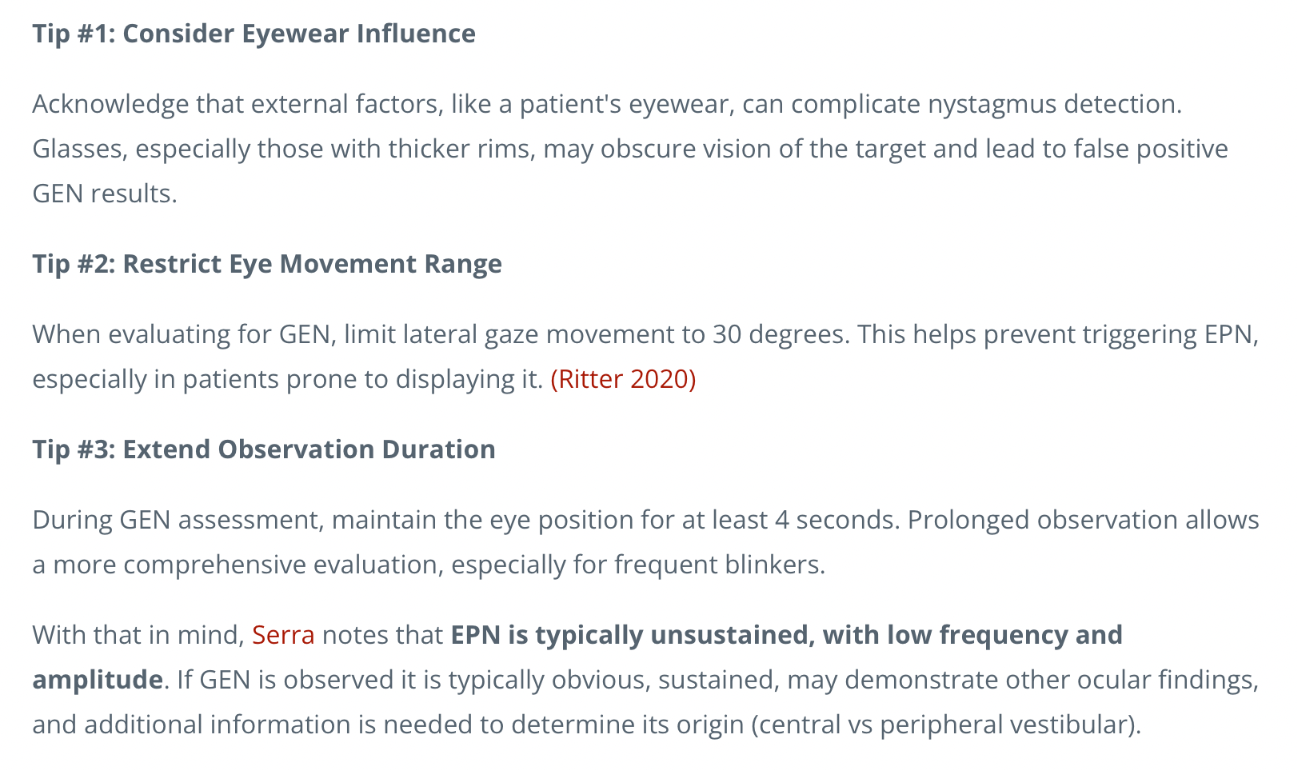
You are examining a patient with dizziness and notice horizontal nystagmus when they look to the left. The resident suggests it may be normal end-point nystagmus.
How would you differentiate between physiologic end-point nystagmus and pathologic gaze-evoked nystagmus? What features help distinguish them clinically?
Physiological nystagmus
This is normal nystagmus, occurring after 6 months of age. It includes end-point and optokinetic nystagmus.
End-point nystagmus is the nystagmus associated with extreme positions of gaze. It is a fine jerk nystagmus with the fast phase being in the direction of the gaze.
Optokinetic nystagmus describes the nystagmus that occurs when following a moving object (such as looking out of a train window). It is a jerk nystagmus - the slow phase follows the target and the fast phase fixates on to the next target:
Gaze evoked nystagmus (Potentially pathological) may be caused by the following:
Structural lesions that involve the neural integrator network, which is dispersed between the vestibulocerebellum, the medulla (region of the nucleus prepositus hypoglossi and adjacent medial vestibular nucleus [NPH/MVN]), and the interstitial nucleus of Cajal (INC)
Recovery from a gaze palsy
Brainstem or cerebellar disease
Side effect of alcohol or the use of oral sedatives, barbiturates or anticonvulsant drugs
Weakness of 1 or more extraocular muscles or the disruption of their innervations
Myasthenia gravis or Guillan Barre syndrome
A 74-year-old woman is brought to the ED by her son after suddenly developing slurred speech and right arm weakness that started one hour ago. On arrival, she is alert and oriented but has expressive aphasia and right-sided hemiparesis. Her blood pressure is 210/100 mmHg. Blood glucose is normal, ECG shows NSR, and she’s being prepared for an emergent non-contrast CT head.
Her son becomes visibly upset and confronts you, saying:
“Why are you just standing around while her blood pressure is sky-high? Why aren’t you treating it right now?!”
You’ve already notified the stroke team and your attending is waiting for imaging before making any further decisions.
❓What is the most appropriate response to the son’s concern?
A) “You’re right, I forgot how to do my job.”
B) “We’re waiting for the CT because we need to lower the blood pressure urgently if it’s a hemorrhagic stroke.”
C) “In suspected strokes, we often allow higher blood pressure temporarily to maintain brain perfusion while we determine the type of stroke.”
D) “We have to wait for a neurologist to decide how to manage her blood pressure.”
E) “We’ll give antihypertensives after her symptoms improve.”
C) “In suspected strokes, we often allow higher blood pressure temporarily to maintain brain perfusion while we determine the type of stroke.”
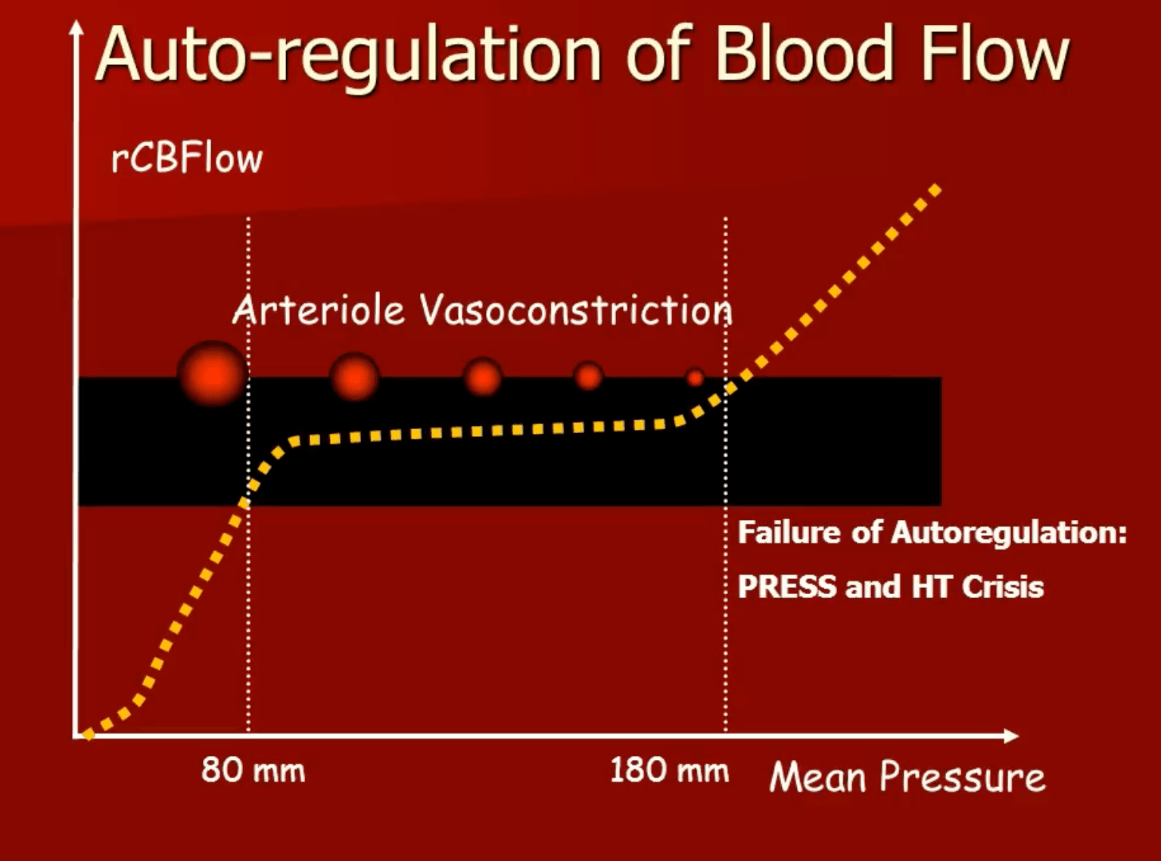
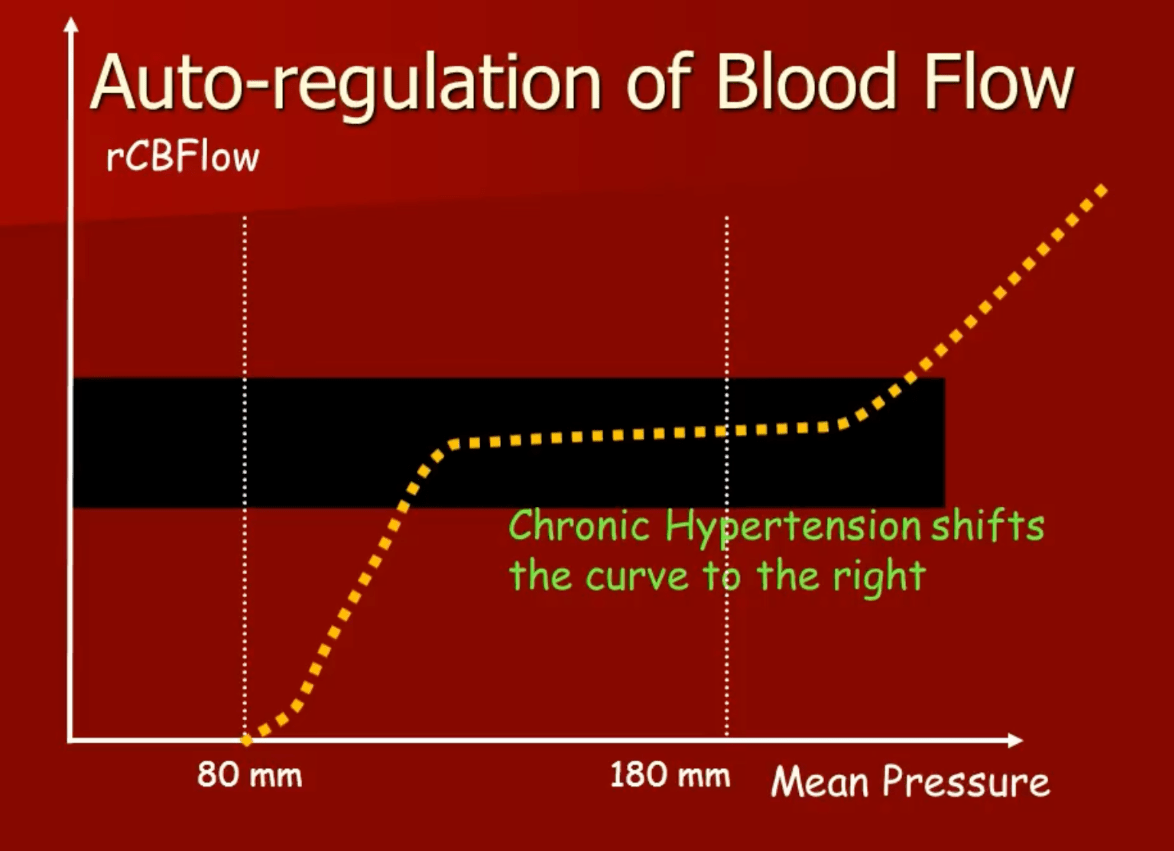
"This arises from an understanding of the cerebral autoregulation curve, which maintains stable blood flow within a range of pressures (MAP of 60–160mmHg) under normal circumstances, but resets in chronic HTN with a shift of the lower limit toward the right"
A 42-year-old woman is brought to the ED by EMS for ongoing generalized tonic-clonic seizures. She was witnessed convulsing continuously for at least 8 minutes before EMS arrival. En route, she received 10 mg of intramuscular midazolam, after which the seizures ceased. On arrival, she is post-ictal but breathing spontaneously with stable vitals.
Which of the following is the most appropriate next step in management?
A. Monitor in ED and reassess in 30 minutes
B. Intubate for airway protection
C. Order a head CT before proceeding with treatment
D. Administer a second-line antiepileptic drug with a loading dose
E. Start long-term oral levetiracetam
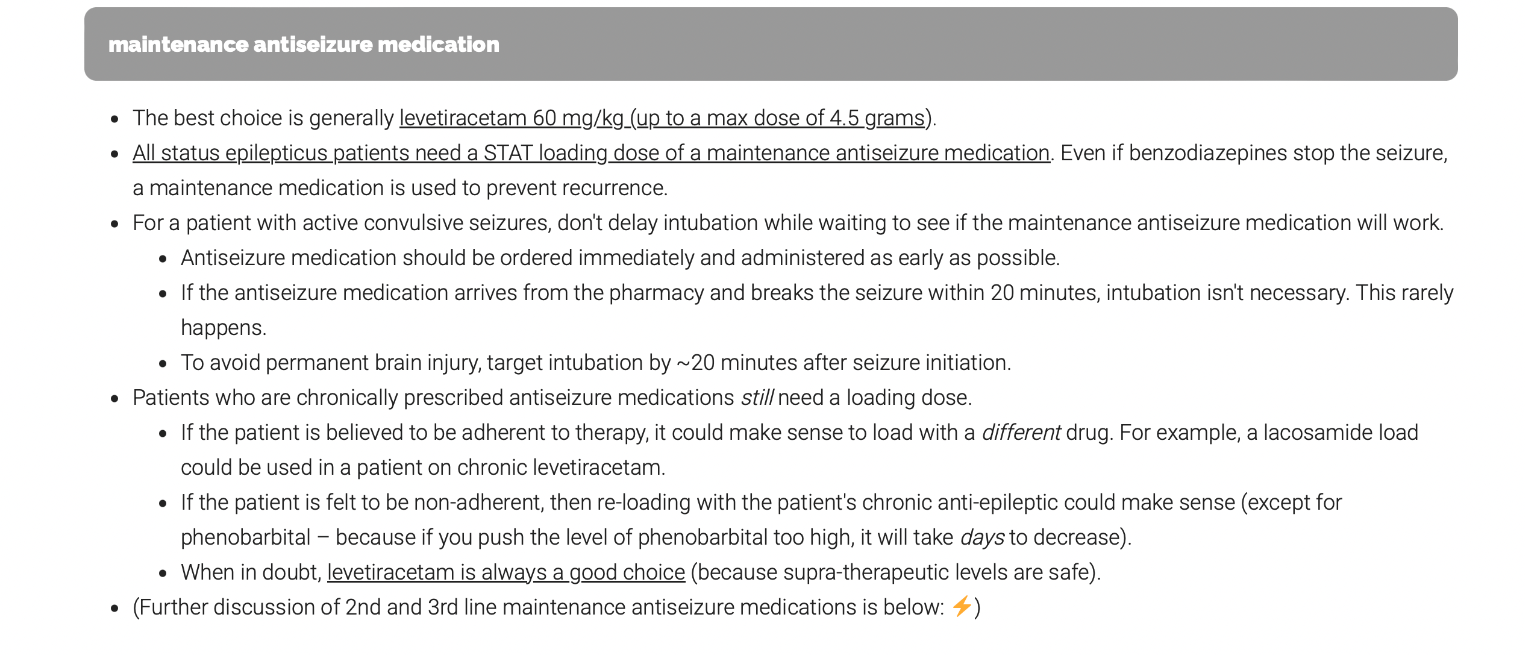
D. Administer a second-line antiepileptic drug with a loading dose
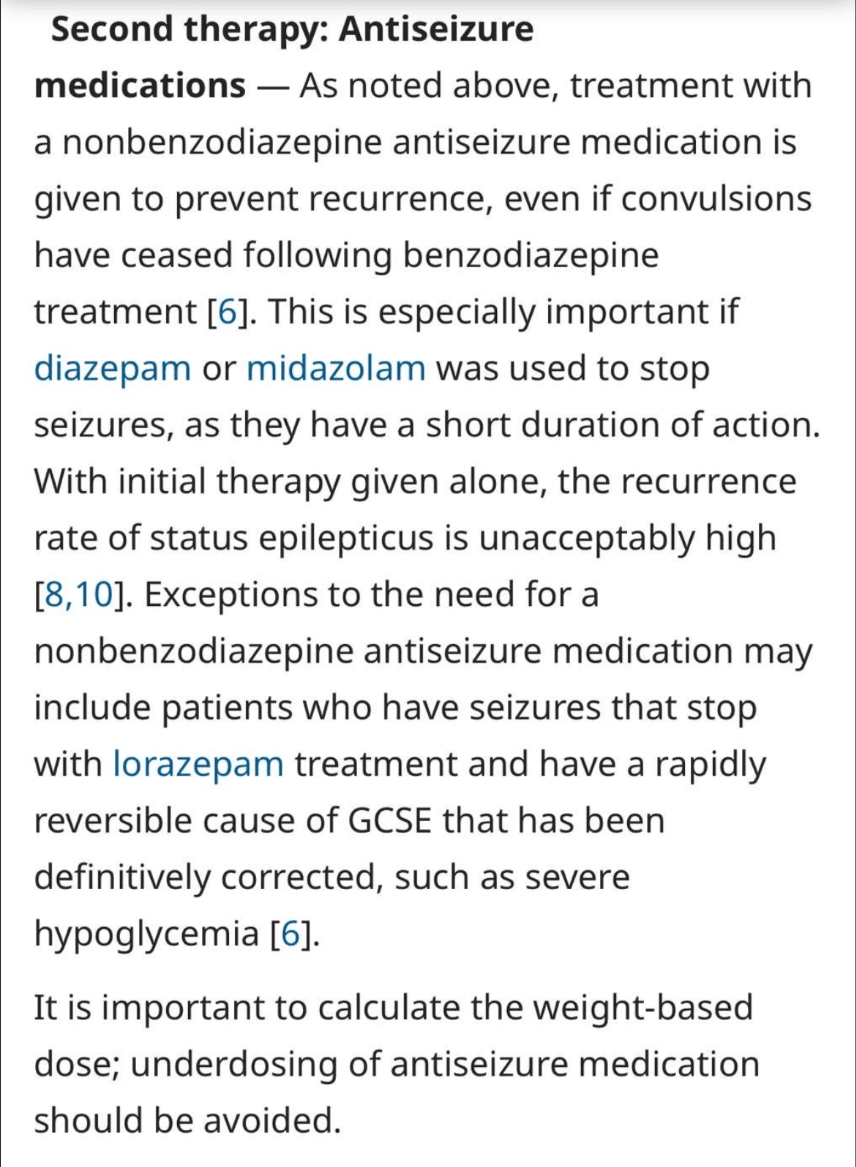
EMCrit*
A 38-year-old woman presents with a sudden, severe thunderclap headache that began during a period of emotional stress. She reports similar headaches over the past week, each triggered by exertion or emotional stress. She denies visual changes, seizures, or confusion. Her BP is 136/82 mmHg. Neurologic exam is normal. She is not on any medications except for sertraline and occasional sumatriptan for migraines.
Non-contrast CT is normal. MRI brain shows no edema or infarct. CTA shows multifocal segmental narrowing of cerebral arteries with a “string of beads” appearance.
Which of the following is the most likely diagnosis?
A) Posterior reversible encephalopathy syndrome (PRES)
B) Subarachnoid hemorrhage from aneurysmal rupture
C) Reversible cerebral vasoconstriction syndrome (RCVS)
D) Migraine with aura
E) Cerebral venous sinus thrombosis (CVST)
C) Reversible cerebral vasoconstriction syndrome (RCVS)
RCVS is often mistaken for PRES or migraine—but it is uniquely associated with recurrent thunderclap headaches, often without initial imaging abnormalities, and classically shows vasoconstriction on vascular imaging.
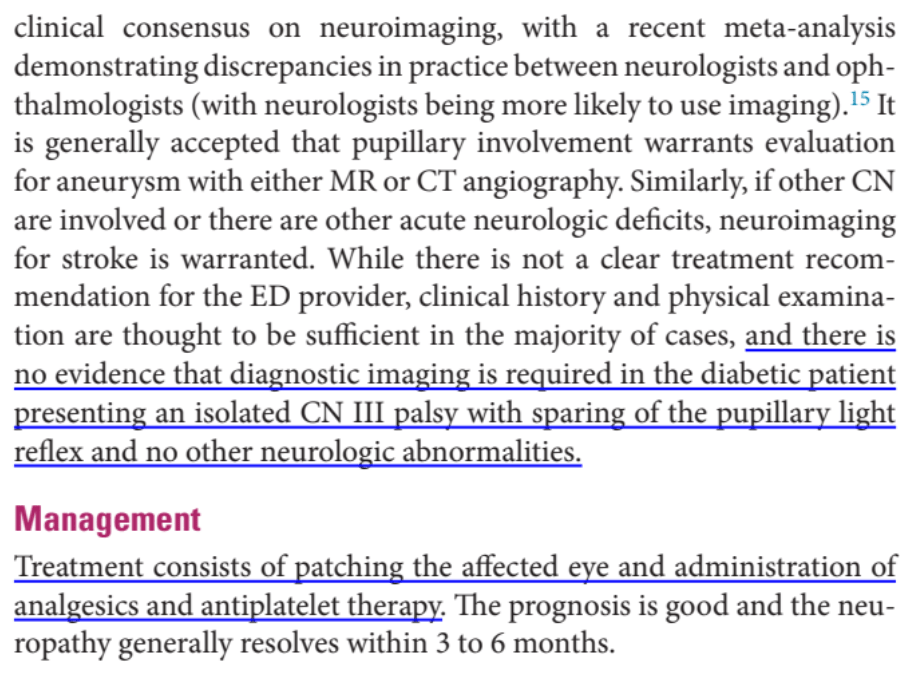
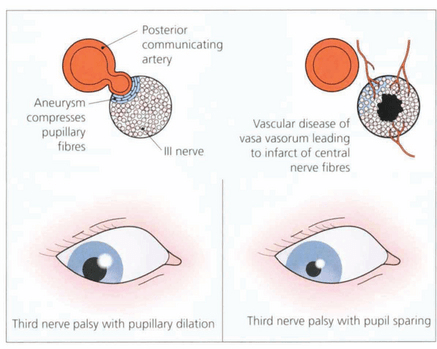
A 62-year-old man with poorly controlled type 2 diabetes presents to the ED with sudden onset of double vision and drooping of his left eyelid. He denies headache, trauma, or other neurologic symptoms. On examination, he has ptosis and his left eye is deviated “down and out.” However, pupillary reflexes are intact bilaterally.
Which of the following is the most likely cause of his presentation?
A. Posterior communicating artery aneurysm
B. Myasthenia gravis
C. Diabetic ischemic mononeuropathy
D. Internuclear ophthalmoplegia
E. Cavernous sinus thrombosis
C. Diabetic ischemic mononeuropathy
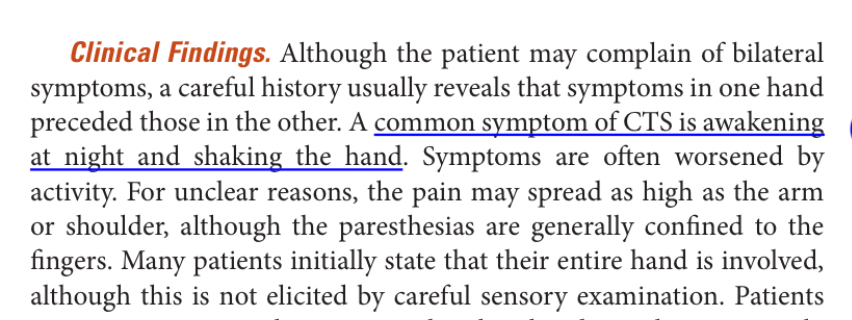
A 58-year-old woman presents with vague discomfort in her right shoulder and upper arm, along with intermittent tingling in her right hand for the past 2 months. She says the pain can be “dull and achy,” and sometimes radiates from her forearm up to her shoulder. The hand symptoms are worse at night and occasionally wake her from sleep. She denies any trauma, neck pain, or recent injury.
On exam:
• Shoulder has full range of motion with mild discomfort on internal rotation
• Spurling’s test is negative
• Pinprick sensation is reduced on the thumb and index finger
• Tinel’s test is inconclusive
• Grip strength is mildly reduced on the right
• Reflexes are intact
Which of the following is the most likely diagnosis?
A) Cervical radiculopathy
B) Rotator cuff tendinopathy
C) Ulnar neuropathy
D) Carpal tunnel syndrome
E) Thoracic outlet syndrome
D) Carpal tunnel syndrome
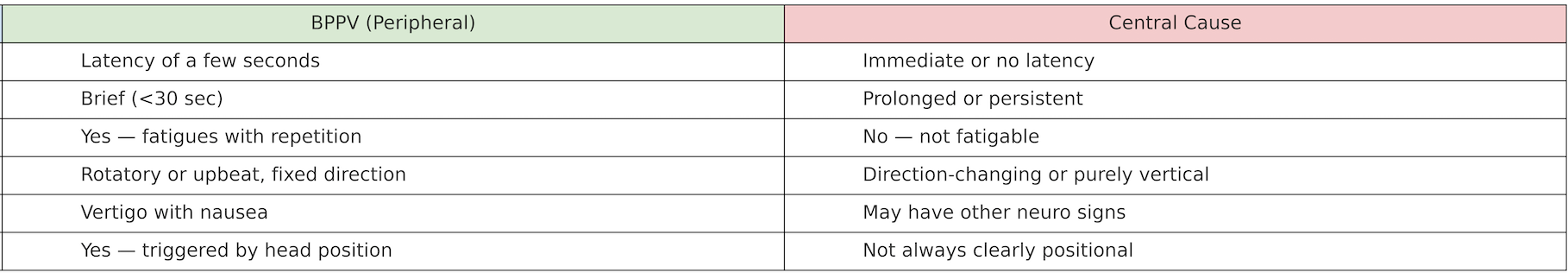
A 68-year-old man with hypertension and diabetes presents with sudden-onset vertigo, nausea, and unsteadiness. He denies hearing loss, tinnitus, or trauma. A bedside Dix-Hallpike maneuver is performed. It provokes immediate onset of down-beating nystagmus without torsional movement, lasting over a minute. The patient reports mild dizziness during the test.
The resident diagnoses BPPV and discharges the patient. He returns 8 hours later with worsening gait imbalance and slurred speech. Neurologic exam now reveals truncal ataxia and mild right-sided dysmetria.
Which of the following best explains the missed diagnosis?
A. Dix-Hallpike is insensitive for BPPV in elderly patients
B. Symptoms evolved too quickly for initial identification
C. Dix-Hallpike was positive, confirming a peripheral cause
D. The pattern of nystagmus was inconsistent with BPPV and should have raised concern for a central lesion
E. CT brain is required to rule out BPPV in elderly patients
D. The pattern of nystagmus was inconsistent with BPPV and should have raised concern for a central lesion
A 34-year-old man with no significant medical history presents in generalized convulsive status epilepticus. He has been seizing for over 45 minutes despite receiving multiple doses of lorazepam, followed by IV loading of levetiracetam and fosphenytoin. He is intubated and sedated but continues to have subtle facial twitching and EEG-confirmed seizure activity. The ICU team considers initiating ketamine infusion.
❓ Which of the following best explains why ketamine may be effective at this stage of status epilepticus?
A) Ketamine enhances GABA-A receptor activity when benzodiazepines fail
B) Ketamine blocks AMPA receptors to suppress excitatory transmission
C) Prolonged seizures lead to GABA-A receptor downregulation and NMDA receptor upregulation
D) Ketamine activates inhibitory glycine receptors in the spinal cord
E) Benzodiazepines inhibit ketamine metabolism, enhancing its efficacy
C) Prolonged seizures lead to GABA-A receptor downregulation and NMDA receptor upregulation
In prolonged status epilepticus, the brain undergoes adaptive receptor trafficking:
• GABA-A receptors are internalized → ↓ responsiveness to benzodiazepines
• NMDA receptors are upregulated → ↑ excitatory glutamate activity
• Ketamine, an NMDA receptor antagonist, works on this glutamatergic pathway that becomes more dominant as seizures progress.
• This makes ketamine especially valuable in refractory or super-refractory SE, where GABAergic drugs (like benzos or barbiturates) may fail.
A 42-year-old man presents with recurrent episodes of excruciating left-sided orbital pain that lasts around 45 minutes. During attacks, he experiences tearing from the left eye, nasal congestion, and ptosis. The headaches occur daily for several weeks and then go into remission. He is restless and paces during attacks.
You suspect a cluster headache.
❓ This headache is best classified under which of the following headache syndromes?
A) Primary stabbing headaches
B) Trigeminal autonomic cephalalgias
C) Chronic migraine variants
D) Tension-type headache
E) Cranial neuralgias
B) Trigeminal autonomic cephalalgias
Not all unilateral “cluster-like” headaches are cluster headaches
• Knowing TACs helps differentiate the rare but treatable mimics (e.g. paroxysmal hemicrania responds dramatically to indomethacin; SUNCT doesn’t).
• If you just call everything “cluster,” you’ll miss the right treatment.
Some TACs are red flag mimics
• Short-lasting, frequent attacks with autonomic signs can be secondary to things like pituitary tumors, aneurysms, or brainstem lesions — especially in atypical presentations.
• Using the TAC framework helps you think systematically and recognize when to image or refer urgently.
A 60-year-old man is admitted for community-acquired pneumonia. He is recovering well on antibiotics. On morning rounds, a resident notes right-sided ptosis and miosis. The patient denies trauma, headache, or eye pain. Extraocular movements and facial strength are intact. Review of the chest X-ray shows a subtle fullness in the right lung apex, attributed to positioning.
❓ What is the most appropriate next step?
A) MRI brain with contrast
B) CT chest with apical views
C) CT angiography of the head and neck
D) Reassure and monitor
E) Lumbar puncture
B) CT chest with apical views
• Subtle apical abnormality + Horner’s = classic Pancoast tumor workup
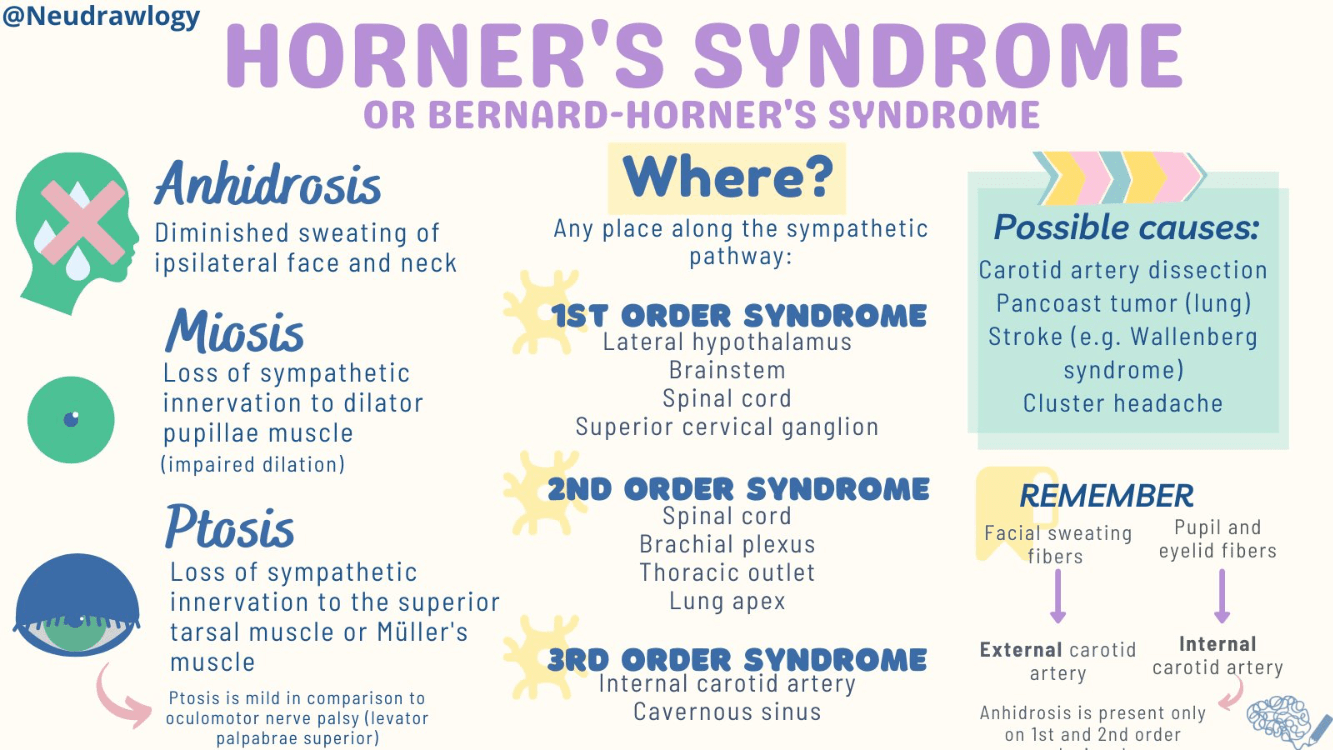
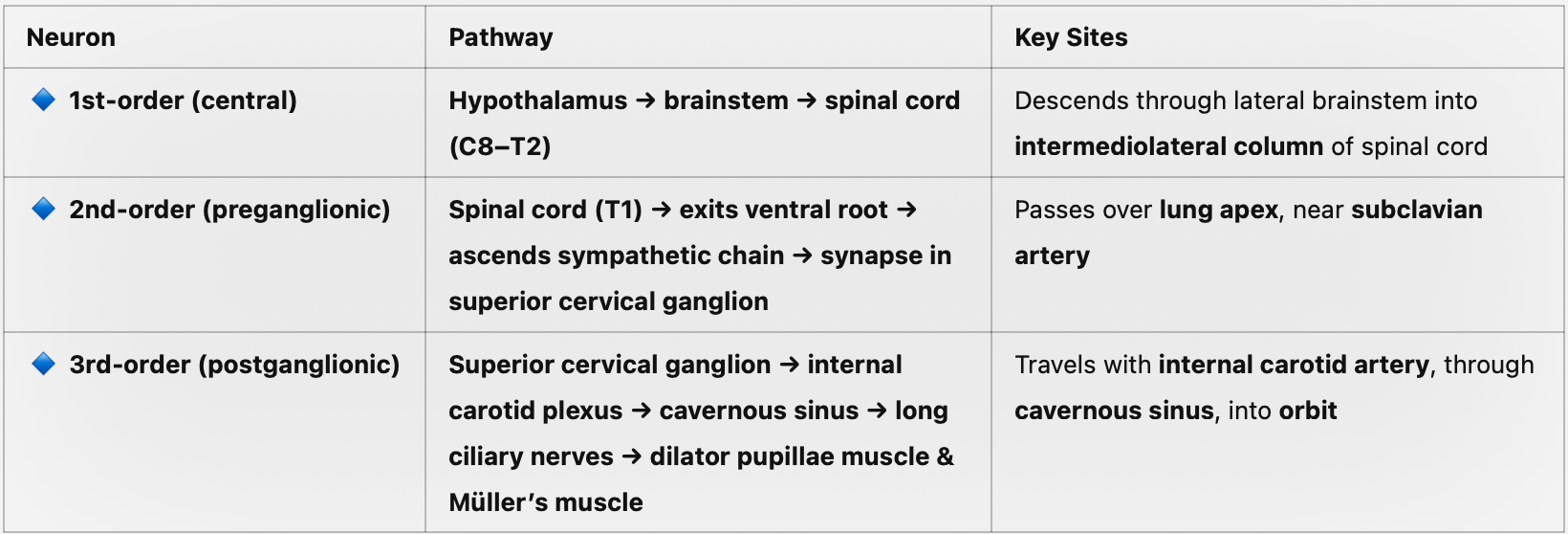
• If sweating is affected, suggests a lesion before the superior cervical ganglion
A 42-year-old man presents with 3 days of progressive bilateral leg weakness and areflexia. He reports mild back pain but denies fever, sensory level, or bowel/bladder dysfunction. Examination reveals symmetric lower extremity weakness and absent ankle reflexes. He is alert, afebrile, and has stable vital signs. You suspect Guillain-Barré Syndrome and are preparing to initiate IVIG.
Before treatment begins, the attending recommends performing a lumbar puncture.
❓ What is the most important reason to perform LP before starting therapy in this patient?
A) Confirm albuminocytologic dissociation to support GBS diagnosis
B) Identify viral meningitis as a potential trigger
C) Rule out spinal cord compression before initiating IVIG
D) Exclude alternative diagnoses that may contraindicate immunotherapy
E) Reduce CSF pressure and relieve back pain
D) Exclude alternative diagnoses that may contraindicate immunotherapy
While albuminocytologic dissociation (high protein, normal WBC) supports GBS, it may not appear until after the first week.
• More importantly, LP helps rule out dangerous mimics:
• Infectious causes (e.g., HIV, Lyme, CMV polyradiculitis)
• Malignant infiltration, leukemia, lymphoma
• Spinal arachnoiditis
• Giving IVIG or plasma exchange in these mimics could delay proper treatment or worsen outcomes.
A 68-year-old man is brought to the ED after being found by his wife at 6:30 AM with slurred speech and right-sided weakness. He was last seen normal when they went to bed at 10:30 PM. Non-contrast CT shows no hemorrhage or early ischemic changes. CTA reveals a left M2 occlusion, and CT perfusion shows a small infarct core with a large penumbra. Your center has the ability to perform MRI and CT perfusion. He arrives at 7:10 AM.
You hear the stroke fellow asking, “Should we consider thrombolysis, or is he out of window?”
❓Which of the following best reflects the current direction in managing wake-up strokes?
A) IV thrombolysis is contraindicated due to unknown time of onset
B) Thrombectomy is appropriate, but IV thrombolysis is not recommended in this case
C) MRI-based DWI/FLAIR mismatch is the only way to determine eligibility for thrombolysis
D) Imaging-based selection with CT perfusion may justify IV thrombolysis in extended or wake-up strokes
E) No intervention is indicated due to time of last known well
D) Imaging-based selection with CT perfusion may justify IV thrombolysis in extended or wake-up strokes
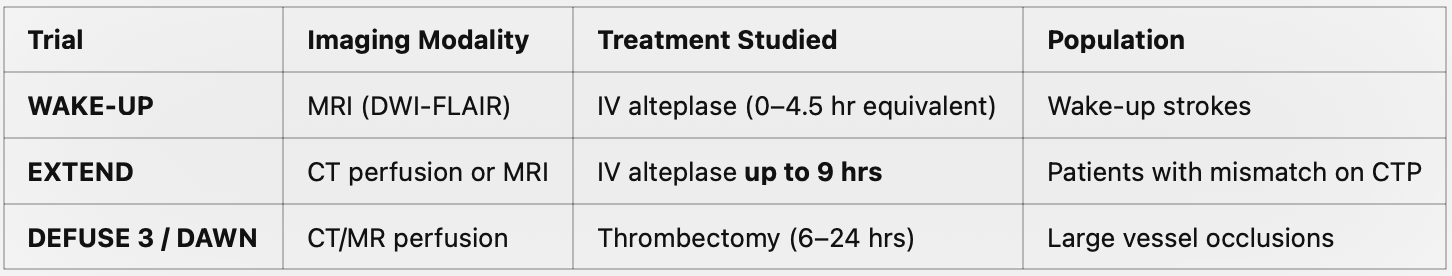
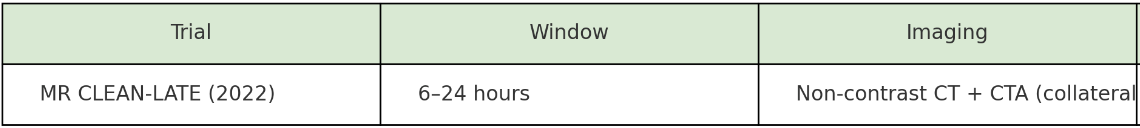
Future-ready clinicians should ask:
• Do we have the imaging tools to see if there’s tissue to save?
• Not “how many hours,” but “how much brain is left to save?”
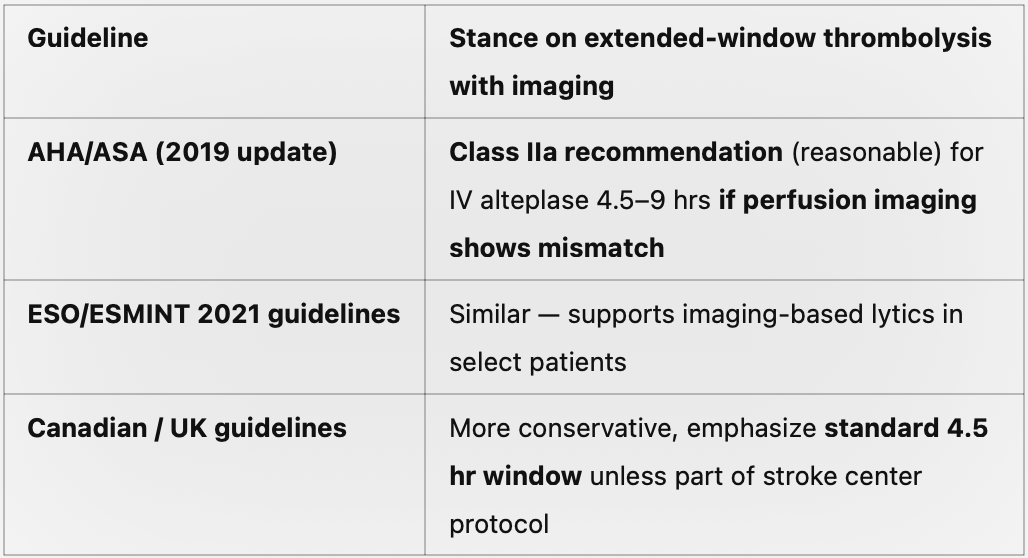
A 74-year-old woman is brought to the emergency department by her daughter due to 2 days of increasing unsteadiness, slurred speech. She has a history of epilepsy, hypertension, atrial fibrillation and depression. Her medications include phenytoin, lisinopril, warfarin and sertraline. The daughter denies any recent trauma or seizures but notes that the patient nearly fell twice today.
On exam:
• Temp: 36.8°C
• HR: 84 bpm
• BP: 138/76 mmHg
• Alert
• Horizontal non-fatigueble nystagmus, dysarthria, and broad-based gait
• No clonus, hyperreflexia, rigidity, or focal deficits
A non-contrast head CT/CTA is unremarkable.
Which of the following is the most appropriate next step in management?
A) Start intravenous acyclovir
B) Administer IV lorazepam and cooling measures
C) Order a phenytoin level
D) Consult neurology for inpatient stroke workup
E) Initiate high-dose corticosteroids for possible encephalitis
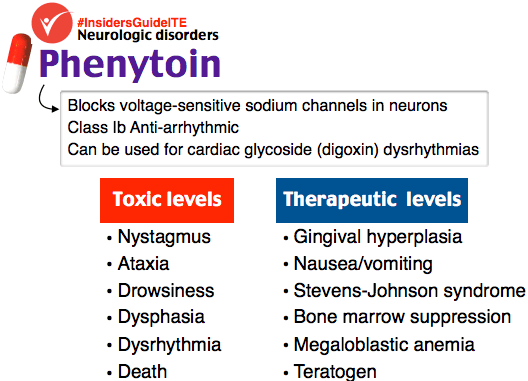
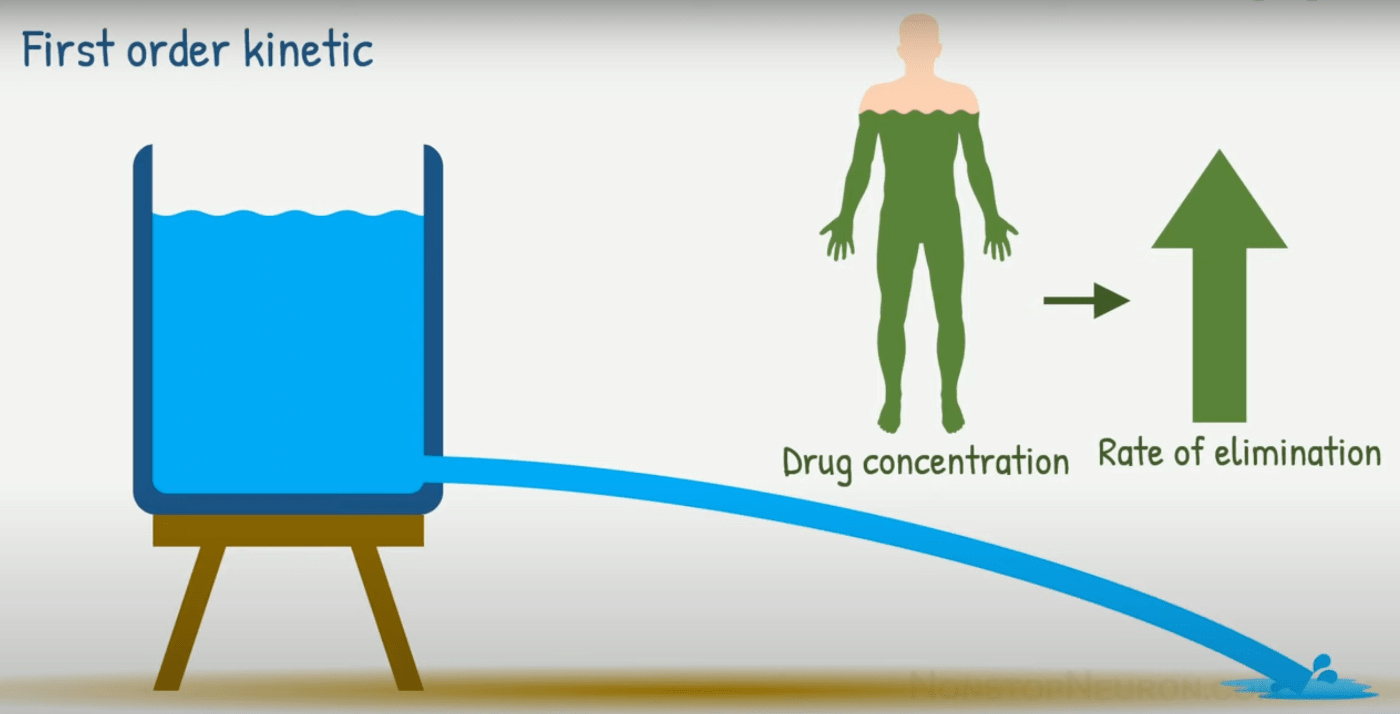
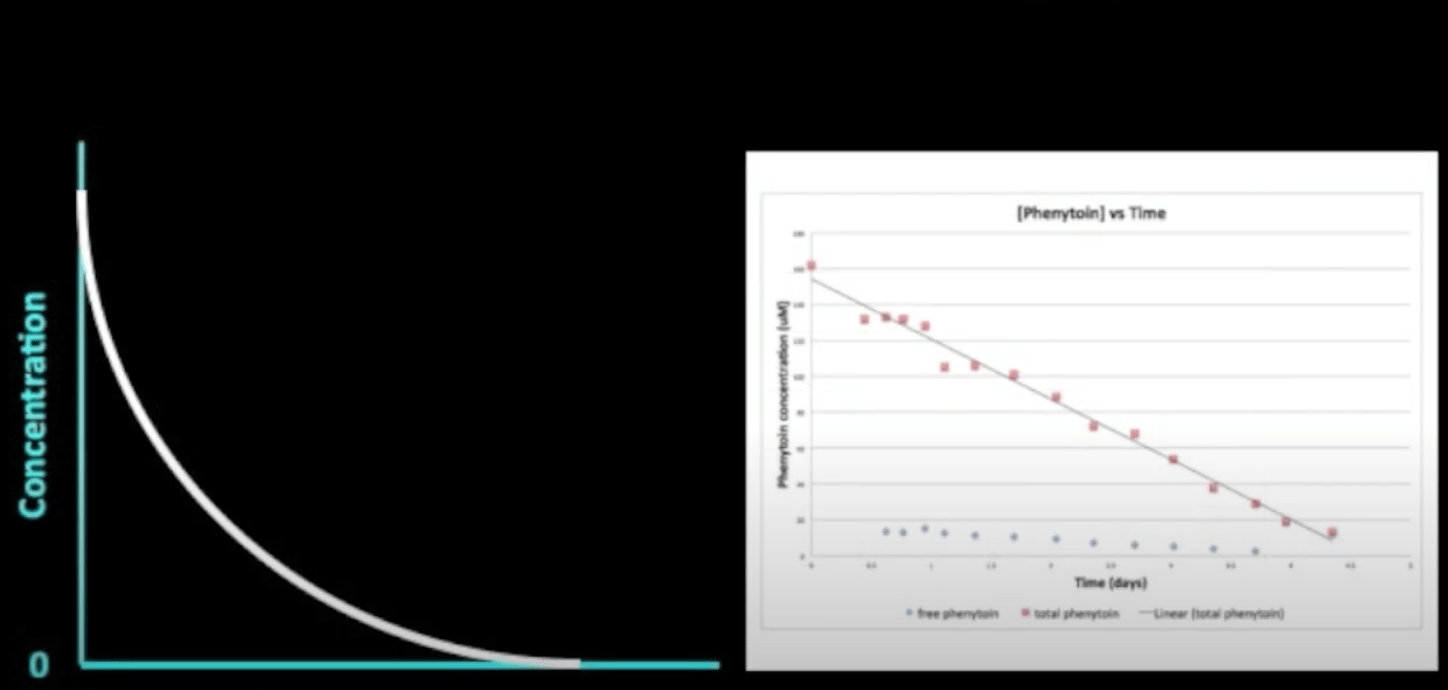
Bonus question: Phenytoin follows _______ Order Kinetics.
Why else suspect phenytoin toxicity?
• Age-related decline in hepatic metabolism
• Drug interactions: warfarin competes for CYP metabolism, increasing free phenytoin levels
• Narrow therapeutic window with zero-order kinetics—small increases in dose can lead to toxicity
A 37-year-old woman presents with a 3-day history of gradual, severe, disabling headache. She describes it as diffuse and pressure-like, with nausea and neck stiffness but no photo-phobia. The pain is significantly worse when upright and improves after lying flat. She denies recent trauma, LP, or known illness. Vitals are normal, and neurologic exam is non-focal. Fundoscopy reveals subtle optic disc blurring.
A non-contrast head CT/ CTA is normal.
❓ Which of the following is the most likely diagnosis?
A) Subarachnoid hemorrhage
B) Spontaneous intracranial hypotension
C) Idiopathic intracranial hypertension
D) Cervical artery dissection
E) Viral meningitis
B) Spontaneous intracranial hypotension
Some SIH cases follow subtle Valsalva (retching, coughing, minor trauma), many have no clear inciting event.
• Congenital dural weakness (often related to connective tissue disorders like Marfan or Ehlers-Danlos) can predispose to spontaneous spinal CSF leaks.
• Leak sites are often found in the thoracic spine, sometimes due to meningeal diverticula or calcified disc spurs eroding the dura.
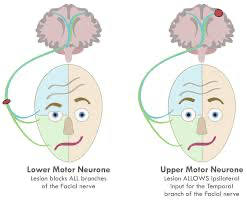
A 52-year-old man presents to the emergency department with sudden onset right-sided facial weakness. He reports that it started this morning when he noticed difficulty blinking and drooling from the right side of his mouth. He denies headache, limb weakness, vertigo, or hearing loss. Examination reveals:
• Inability to raise the right eyebrow
• Loss of nasolabial fold
• Incomplete eye closure on the right
• Normal speech, gait, and limb strength
• No rash or vesicles
He has a history of a resected cerebellopontine angle tumor (vestibular schwannoma) 8 years ago with no recurrence since, and he has been neurologically intact until now.
What is the most appropriate next step in management?
A) Initiate prednisone and valacyclovir without imaging
B) Order MRI of the brain with attention to the internal auditory canal
C) Discharge with eye care instructions and follow-up in 72 hours
D) Begin corticosteroids and schedule outpatient neurology evaluation
E) Perform lumbar puncture to rule out infectious or inflammatory causes
B) Order MRI of the brain with attention to the internal auditory canal
Any LMN facial palsy with risk atypical features—gradual onset, recurrent, bilateral, or associated systemic/neurologic signs—should not be assumed to be Bell’s palsy. These cases warrant further workup, often including imaging, serologies, or lumbar puncture depending on the differential.
Bonus question: name a few other conditions that presents with a LMN distribution which are not idiopathic bells.
1. Infectious:
• Herpes zoster oticus (Ramsay Hunt syndrome)
– LMN palsy + ear pain + vesicles in the ear canal
• Lyme disease
– Often bilateral; consider in endemic areas or with tick exposure
– Systemic signs (fever, target rash, arthralgia)
2. Neoplastic:
• Cerebellopontine angle tumors (e.g. acoustic neuroma/vestibular schwannoma)
– Gradual onset, hearing loss often present
– History of prior tumor resection = high risk for recurrence
• Parotid gland tumors
– Facial weakness with firm mass near the angle of the jaw
3. Trauma:
• Temporal bone fractures
– Immediate or delayed facial paralysis
– Often associated with hemotympanum or hearing loss
4. Neurologic/Autoimmune:
• Guillain-Barré syndrome (Miller Fisher variant)
– Often bilateral facial weakness
– Look for areflexia and ataxia
• Sarcoidosis (Heerfordt syndrome)
– Facial nerve palsy + uveitis + parotid swelling
– More common in African descent; consider with other systemic symptoms
5. Iatrogenic:
• Post-surgical injury (e.g. parotidectomy, mastoid surgery, CPA tumor resection.
A 56-year-old man presents with 3 months of progressive numbness and tingling in his feet, unsteady gait, and recent difficulty with buttoning his shirt. He is diabetic and on Metformin for the past year, he denies alcohol use. His exam reveals decreased vibration and proprioception in the lower limbs, positive Romberg sign, and Brisk reflexes. No weakness or spasticity is noted. CBC shows mild macrocytosis (MCV 103), but his serum B12 level is 180 pg/mL (normal: 200–900).
Which of the following is the most appropriate next step going forward?
A) Start empiric folic acid and reassess in 1 month
B) Order MRI of the cervical/ thoracic spine.
C) Order EMG/NCS to evaluate for large fiber neuropathy
D) Repeat B12 level in 6 weeks
E) Start high-dose vitamin B1 (thiamine) therapy
B) Order MRI of the cervical/ thoracic spine.
Subacute combined degeneration is a progressive demyelinating disease of the posterior columns and lateral Cortico-Spinal tracts of the spinal cord, caused by vitamin B12 deficiency.
🧠 Why is the cervical spine most affected in subacute combined degeneration (SCD)?
Because the posterior columns and corticospinal tracts are largest and most myelinated in the cervical region, making them more vulnerable to B12 deficiency-induced demyelination.
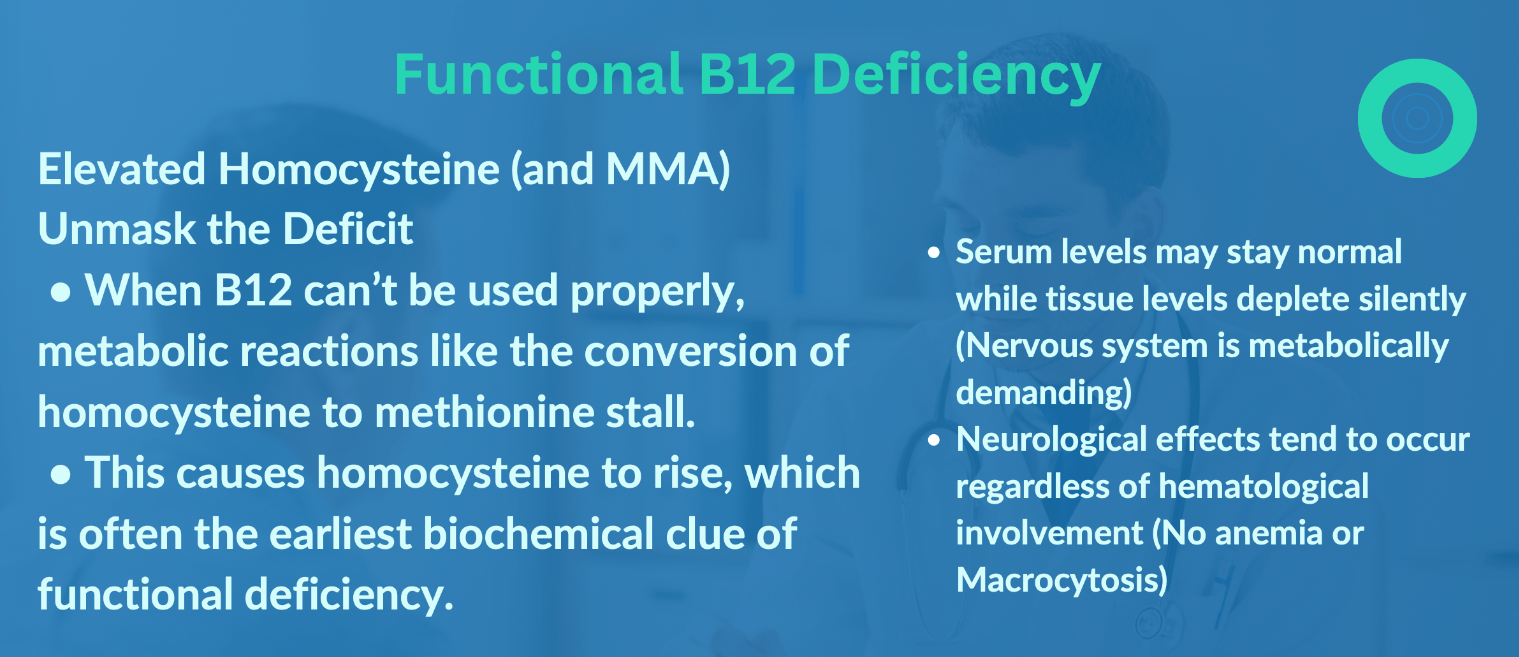
Bonus question: If B12 levels were normal and patient present with otherwise a clear picture of B12 neuropathy, which test supports your diagnosis?