ECG axis of this patient:
Right axis deviation
Diagnose/Finding?
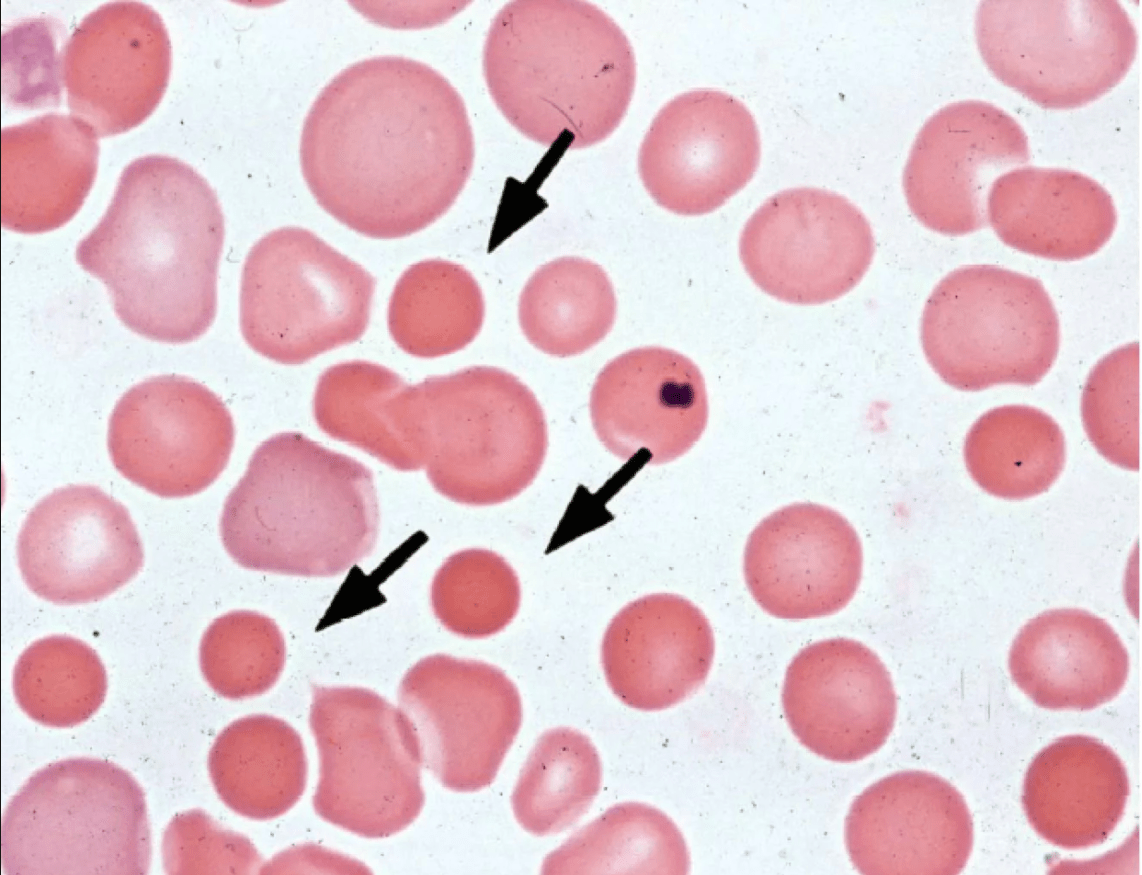
Hereditary Spherocytosis (HS)/Spherocytes
Drug class used before adrenalectomy for pheochromocytoma
α-Receptor blocker
A 66-year-old woman is seen for a preoperative medical evaluation before total right knee arthroplasty. Medical history is significant for atrial fibrillation, hypertension, and peripheral vascular disease. Medications are rivaroxaban, metoprolol, losartan, and atorvastatin.
On physical examination, vital signs are normal. The physical examination documents osteoarthritis of the knee and an irregular heart rhythm.
Laboratory studies show a serum creatinine level of 1.0 mg/dL (88.4 µmol/L) and an estimated glomerular filtration rate greater than 60 mL/min/1.73 m2.
Which of the following is the most appropriate perioperative management of the patient's rivaroxaban?
Withhold rivaroxaban 3 days before surgery
Timing of initiation of enteral nutrition in ICU
24-48 hours after admission
Manifestations:
Hypertension
Diaphoresis
Agitation
Seizures
Mydriasis
Sympathomimetic syndrome
(probable drugs: Cocaine, Amphetamines, Ephedrine, Caffeine)
A 48-year-old man is hospitalized following 4 weeks of cough and fever unresponsive to outpatient antibiotic therapy.
Chest CT scan is shown.
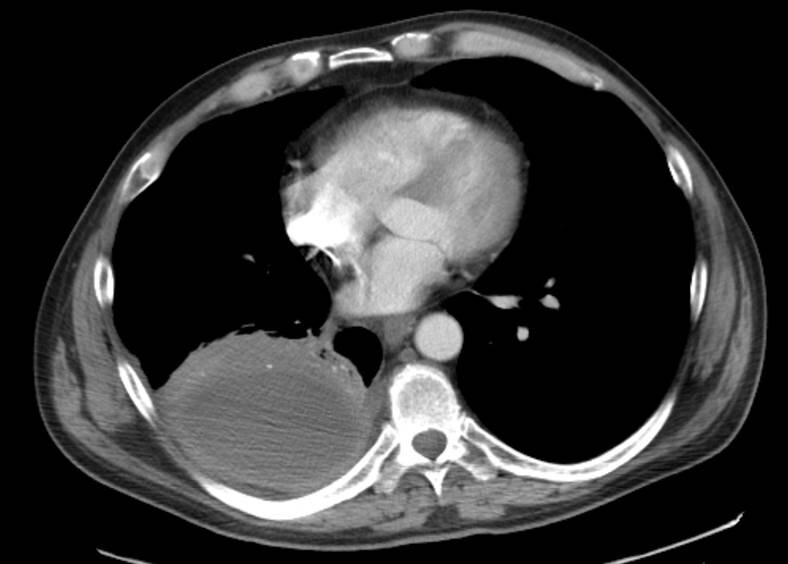
Which of the following is the most likely diagnosis?
Empyema
An 84-year-old man is evaluated during a routine physical examination. His only concern is a gradual loss of stamina and low energy. He can no longer complete his routine 2-mile run without stopping to rest with a prolonged recovery time. He has hypertension, for which he takes lisinopril.
On physical examination, blood pressure is 125/78 mm Hg and pulse rate is 52/min. Heart rate is regular. The remainder of the examination is unremarkable.
Most appropriate management?
Pacemaker implantation
Diagnostic clues, who is 1 and who is 2?
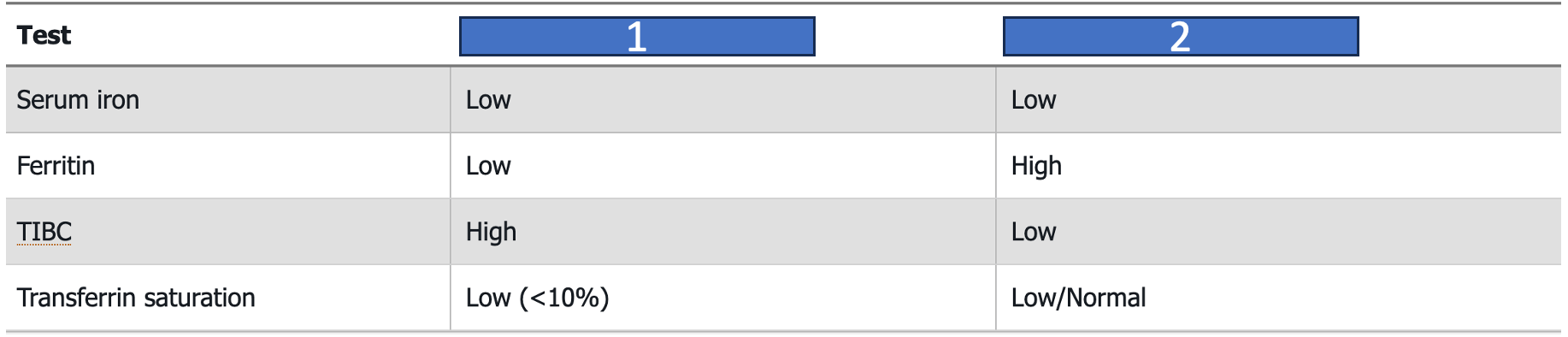
1: Iron deficiency anemia
2: Anemia of chronic disease
A 59-year-old man is evaluated for headaches, pallor, and panic attacks for the past year. His long-term hypertension has also become harder to control. Medications are chlorthalidone, lisinopril, metoprolol, and diltiazem.
On physical examination, blood pressure is 164/98 mm Hg. The remainder of the examination is normal.
Which of the following is the most appropriate diagnostic test?
Plasma free metanephrine measurement
An 82-year-old woman is seen for a preoperative medical evaluation before undergoing cataract surgery. The patient is wheelchair bound. She reports stable shortness of breath with minimal to moderate exertion. Medical history is significant for hypertension, chronic kidney disease, COPD, and degenerative joint disease. Medications are albuterol, ipratropium, and beclomethasone inhalers; lisinopril; metoprolol; and oxygen by nasal cannula, 2 L/min continuously.
On physical examination, blood pressure is 150/85 mm Hg, pulse rate is 97/min, respiration rate is 24/min, and oxygen saturation is 94% on 2 L/min of oxygen by nasal cannula. Breath sounds are distant, with an occasional wheeze.
Which of the following is the most appropriate preoperative testing for this patient?
No further testing
If you would like to Improve respiratory acidosis, the intermediate step is to ↓ Arterial PCO2
Make the ventilator do this by:
Increasing respiratory rate
Increasing tidal volume
Manifestations:
- Hypervigilance
- Agitation (usually easily controlled)
- Hyperactive delirium
- Hallucinations (picking at objects in air)
- Mumbling speech (described as "mouth full of marbles")
- Mydriasis
- Dry mucous membranes
- Decreased bowel sounds
- Urinary retention
- Choreoathetosis
- Seizures (rare)
Anticholinergic syndrome
Agents:
- Diphenhydramine (and other antihistamines)
- Atropine and similar agents (hyoscyamine, dicyclomine, scopolamine, and naturally occurring belladonna alkaloids [eg, jimson weed])
- Tricyclic antidepressants
- Cyclobenzaprine
- Orphenadrine
- Phenothiazines
An 80-year-old man is evaluated for dyspnea following a large-volume gastric aspiration. He was admitted to the hospital 2 days ago with gram-negative sepsis.
Chest radiograph is shown.
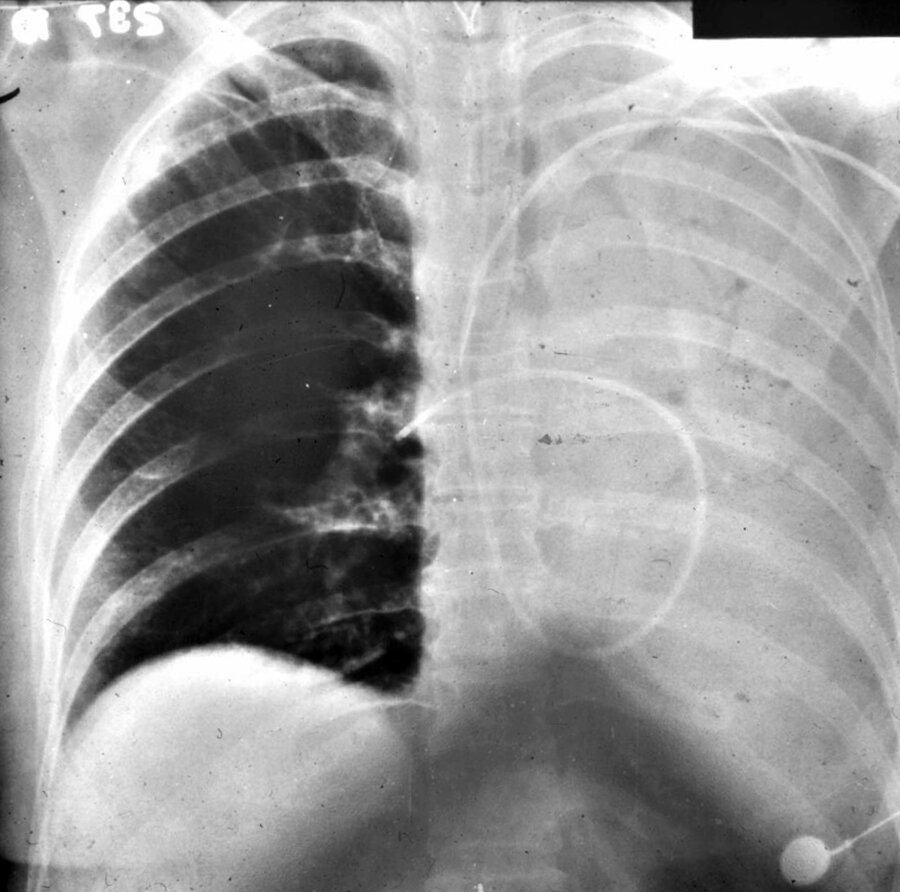
Which of the following is the most likely diagnosis?
Left lung atelectasis
A 57-year-old man is evaluated for a 2-month history of exertional chest pain.
Baseline ECG is normal. Positive treadmill stress testing.
Coronary angiographic findings include a 60% distal left main bifurcation stenosis with extension into the proximal left circumflex artery. There is an additional 80% stenosis involving the bifurcation of the left anterior descending artery and large first diagonal branch. The right coronary artery is large and without significant stenosis.
Left ventriculogram shows global left ventricular dysfunction with a left ventricular ejection fraction of 42%.
Most appropriate management?
CABG
A 42-year-old woman is evaluated for several months of fatigue. She reports a normal diet and no gastrointestinal symptoms. Medical history is notable for hypothyroidism and vitiligo. Her only medication is levothyroxine. CBC remarkable for Hb:8.8; MCV:117fL
Peripheral smear: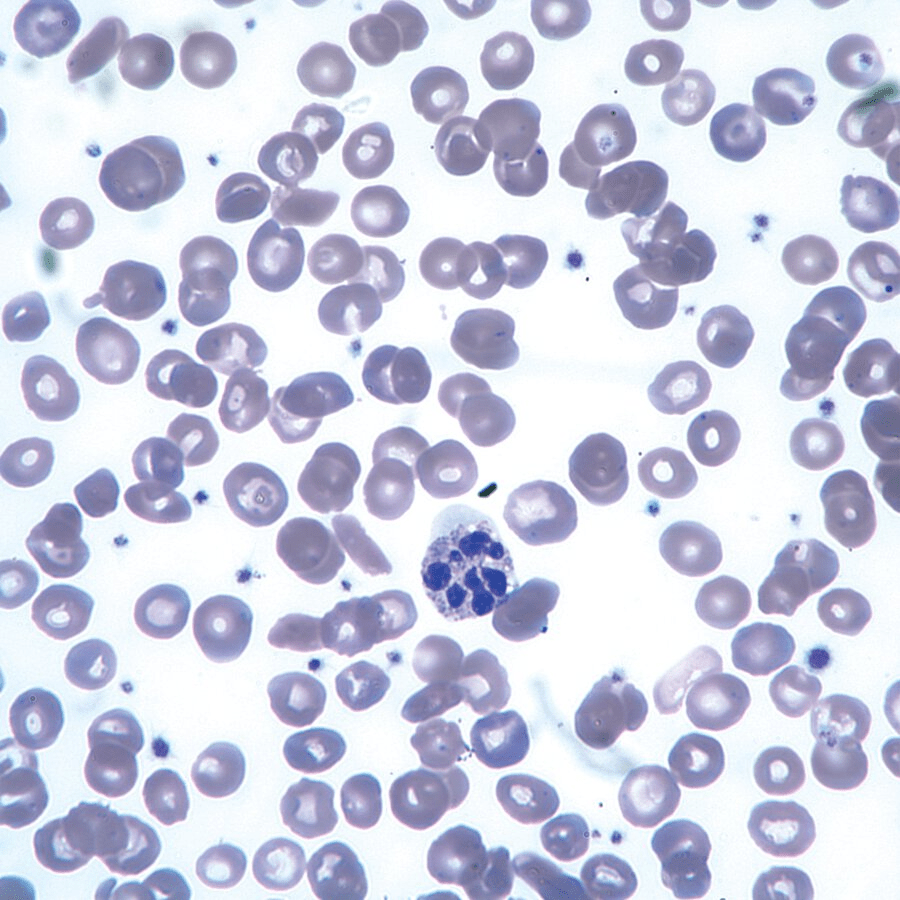
Diagnose + mos appropiate diagnostic testing?
Pernicious anemia/Cobalamine/B12 level
A 30-year-old woman presents with a 4-month history of fatigue and abdominal pain associated with unintentional weight loss of 2.3 kg (5.1 lb). She has no significant past medical history and takes no medications. On examination, her blood pressure is 110/72 mm Hg while sitting and 90/62 mm Hg standing, with a corresponding pulse of 70/min and 88/min, respectively. Her BMI is 19. Notable findings include diffuse hyperpigmentation involving the skin, buccal mucosa, and palmar creases, with otherwise normal vital signs and visual field testing. Laboratory results reveal hyponatremia (132 mEq/L), hyperkalemia (5.4 mEq/L), a markedly reduced morning serum cortisol level (2.1 μg/dL), and a significantly elevated adrenocorticotropic hormone level (580 pg/mL).
Most appropriate next step in management?
Glucocorticoid replacement therapy (hydrocortisone) + Mineralocorticoid replacement (fludrocortisone)
A 68-year-old man undergoes a preoperative medical evaluation before total knee arthroplasty. Medical history is significant for hypertension, hyperlipidemia, degenerative joint disease, and psoriasis. Medications are amlodipine, metoprolol, methotrexate, folic acid, and atorvastatin.
On physical examination, vital signs are normal. Small, scattered psoriatic plaques are noted on the elbows, knees, and sacrum. Examination of the left knee shows limited range of motion. The remainder of the physical examination is normal.
Which of the following is the most appropriate perioperative medication management?
Continue all medications
A 29-year-old man is evaluated in the hospital for hemorrhagic shock. He has osteogenesis imperfecta and was admitted for a right hip fracture repair 2 days ago. He was placed on low-molecular-weight heparin postoperatively.
Blood pressure is 84/44 mm Hg, pulse rate is 132/min, and respiration rate is 31/min. Oxygen saturation is 91% using a nonrebreather mask. Cardiac examination reveals tachycardia but no murmurs or gallops. He has copious amounts of blood coming from his nose, and there is swelling, bruising, and oozing at the surgical site.
He has an 18-gauge peripheral intravenous catheter in his left forearm.
Which of the following is the most appropriate form of additional intravenous access in this patient?
18-Gauge peripheral catheter in the right arm
Manifestations:
- Hallucinations
- Perceptual distortions (typically visual)
- Depersonalization
- Synesthesia
- Mydriasis (usually)
- Occasional agitation (with or without delirium)+
- Nystagmus (phencyclidine, ketamine)
- Tachycardia, hypertension, agitated delirium (designer phenethylamines)
Hallucinogenic syndrome
Agents:
- Designer phenethylamines and tryptamines (eg, MDMA ["ecstasy"], MDEA)
- Ketamine and methoxetamine
- LSD and psilocybin
- Phencyclidine
- Mescaline
A 59-year-old man recently diagnosed with type 2 diabetes mellitus undergoes a comprehensive ophthalmologic examination.
Funduscopic findings are shown.

Which of the following is the most likely diagnosis?
Proliferative diabetic retinopathy
A 50-year-old woman is evaluated for a 3-month history of progressive chest pain. The pain is worse with physical activity, radiates to the left arm, and is associated with diaphoresis. The pain is relieved by rest.
On physical examination, blood pressure is 167/98 mm Hg, and pulse rate is 58/min. Cardiac examination reveals an S4 and no murmurs.
ECG shows sinus rhythm and left ventricular hypertrophy with a strain pattern.
Most appropriate diagnostic test?
Exercise myocardial perfusion imaging
A 46-year-old woman is evaluated after the incidental discovery of an elevated hemoglobin level. She is asymptomatic, has an unremarkable medical history, and is not taking any medications. On examination, her vital signs are normal, but a palpable spleen tip is noted. Laboratory studies reveal an erythropoietin level of 2 mU/mL (2 U/L), a hematocrit of 51%, a hemoglobin level of 17 g/dL (170 g/L), a leukocyte count of 7000/μL (7 × 10⁹/L), and a platelet count of 750,000/μL (750 × 10⁹/L). Genetic testing is positive for the JAK2 V617F mutation. She is started on low-dose aspirin, and therapeutic phlebotomy is scheduled.
Most appropriate additional management?
No further management
A 43-year-old man has developed changes in skin color and is evaluated for weight loss, nausea, and weakness; TB ppd skin test positive. He was found to have hypoglycemia, and borderline low BP.
Skin findings are shown.

Which of the following is the most likely diagnosis?
Primary adrenal insufficiency
A 76-year-old woman is seen for a preoperative medical evaluation before elective total ankle arthroplasty. She has heart failure with reduced ejection fraction and COPD. She has no chest pain, presyncope, or change in weight. Medications are tiotropium, budesonide, and albuterol inhalers; furosemide; metoprolol; lisinopril; and 2 L/min of oxygen via nasal cannula during exertion.
On physical examination, blood pressure is 145/80 mm Hg, pulse rate is 109/min, respiration rate is 24/min, and oxygen saturation is 90% breathing ambient air. Jugular venous pressure is elevated. There is an S4 and a grade 2/6 systolic murmur at the lower left sternal border. Breath sounds are distant without crackles.
A recent transthoracic echocardiogram showed an ejection fraction of 40%, moderate to severe right ventricle dysfunction, pulmonary artery systolic pressure of 65 mm Hg, and tricuspid regurgitation. ECG shows right bundle branch block.
Which of the following is the most appropriate preoperative management of this patient?
Cancel the surgery
Guess the ventilation mode:
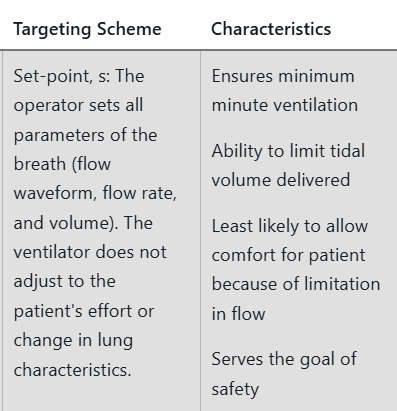
Volume control assist/control
Manifestations:
- Agitation
- Hyperactive delirium
- Confusion
- Mydriasis
- Awake and unresponsive
- Tremor, hyperreflexia, clonus (typically in lower extremities)
- Roving eye movements (ocular clonus)
- Diarrhea
Serotonin syndrome (serotonin toxicity)
Agents:
- MAOIs
- Tricyclic antidepressants
- SSRIs and SNRIs
- Dextromethorphan
- Meperidine
- Refer to UpToDate content on combinations of agents that can cause serotonin syndrome
A 37-year-old man is evaluated for sudden onset of dyspnea without chest pain.
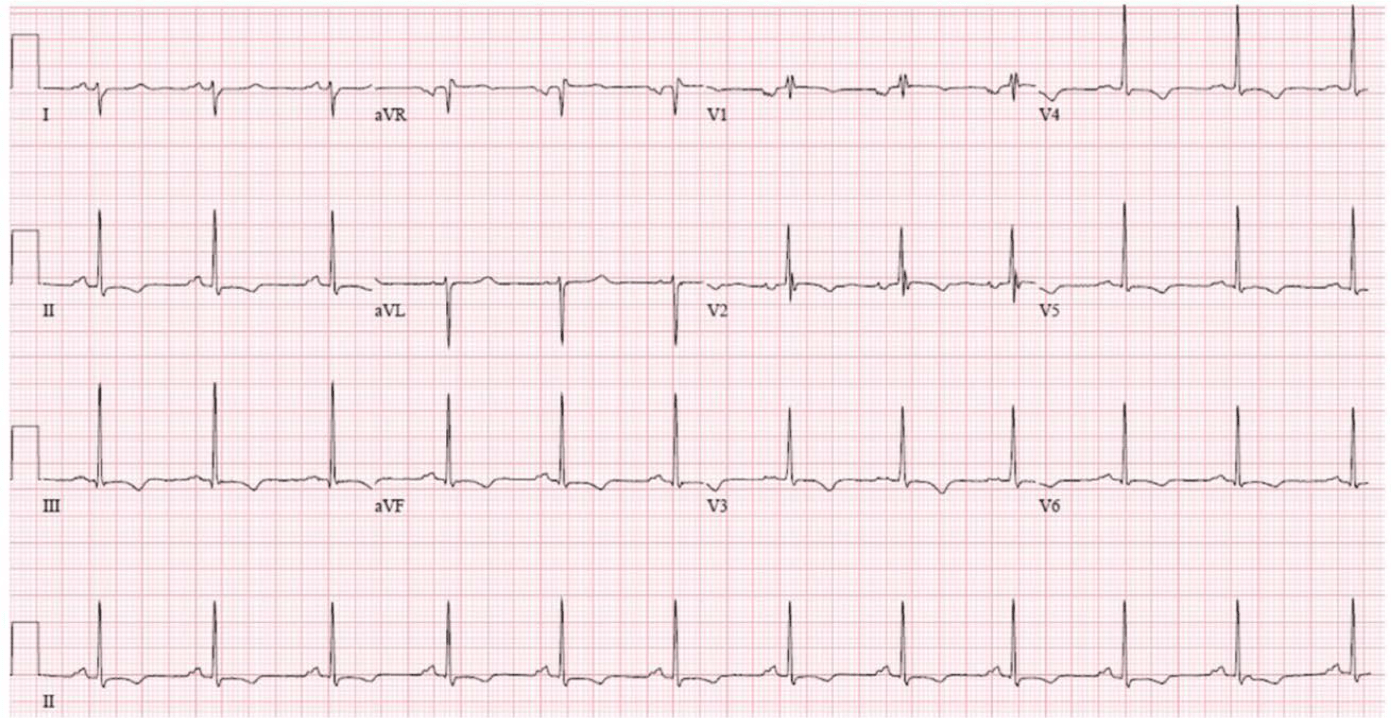
ECG is shown.

Which of the following is the most likely diagnosis?
Pulmonary embolism; S1Q3T3 pattern (prominent S wave in lead I, Q wave in lead III, and inverted T wave in lead III)
A 44-year-old woman is evaluated during a follow-up visit for chronic hypertension. Over the past month, her average blood pressure measured with home blood pressure monitoring was 145/90 mm Hg. There is no family history of hypertension. She has no other medical problems. The patient adheres to a low sodium diet. Medications are maximum doses of amlodipine and lisinopril.
On physical examination, blood pressure is 148/96 mm Hg, and pulse rate is 64/min; other vital signs are normal. BMI is 26. The remainder of the examination is unremarkable.
Laboratory studies show a serum creatinine level of 0.8 mg/dL (70.7 µmol/L) and normal electrolyte levels. Urinalysis shows no blood, protein, or leukocyte esterase.
Most appropriate next step in management?
Add a Thiazide/Add Chlorthalidone
A 21-year-old woman presents with a 4-day history of progressive fatigue, dyspnea on exertion, and dark-colored urine. One week prior, she completed a 5-day course of azithromycin for a cough and fever, which resolved with treatment. On examination, her vital signs are normal, and conjunctival icterus is observed. Laboratory studies reveal a hemoglobin level of 10.7 g/dL (107 g/L), leukocyte count of 8500/μL (8.5 × 10⁹/L), platelet count of 225,000/μL (225 × 10⁹/L), reticulocyte count of 9%, and a haptoglobin level of <10 mg/dL (100 mg/L). A direct antiglobulin test is negative for anti-IgG but strongly positive for anticomplement.
Most probable diagnose?
Cold agglutinin hemolytic anemia/Cold agglutinin disease/Cold autoimmune hemolytic anemia
Invasive test to confirm source of hyperaldosteronism
Adrenal vein sampling
A 76-year-old woman is seen for a preoperative medical evaluation before elective cholecystectomy. Medical history is significant for nonvalvular atrial fibrillation, hypertension, and diabetes mellitus. Medications are warfarin, metoprolol, and metformin.
Which of the following is the most appropriate perioperative management of this patient's warfarin?
Withhold warfarin 5 days prior to surgery; restart 12 hours after surgery
A 73-year-old woman who weighs 56 kg (123 lb) is admitted to the ICU with an exacerbation of severe COPD. Intubation and mechanical ventilation are required: FIO2 of 0.4, tidal volume of 450 mL, and respiration rate of 16/min. Thirty minutes later, her BP has dropped to 82/60 mm Hg. She is restless and has diffuse wheezing with prolonged expiration.
Diagnose?
Auto-PEEP.
Manifestations:
- Sedation
- Confusion
- Stupor
- Coma
- Miosis
- Seizures (typically occur early)
- Salivation
- Urinary and fecal incontinence
- Vomiting, diarrhea, abdominal cramps
- Bronchorrhea and bronchoconstriction
- Muscle fasciculations and paralysis
- Weakness
Cholinergic syndrome
Agents:
- Organophosphate and carbamate insecticides
- Nerve agents (eg, VX, tabun, sarin, soman, and Novichok)
- Nicotine
- Physostigmine
- Rivastigmine
- Bethanechol
- Pilocarpine
- Urecholine
A 23-year-old man is evaluated for anemia, abdominal pain, and arthralgia. He recently renovated an old house, which included scraping and repainting.
Peripheral blood smear is shown.

Which of the following is the most likely diagnosis?
Lead intoxication/basophilic stippling
What is the name of the coffee shop in the sitcom Friends?
Central Perk