You receive a call from your night nurse that a patient admitted for a kidney stone that you are cross-covering, has a BP of 190/80. What should you do (3)?
Check the prior BPs
Ask or evaluate yourself for HTN emergency/EOD
If no symptoms - gently educate your nursing colleagues on recent changes to the guidelines.
Spontaneous falls in BP without any antihypertensive agents occur commonly, at a rate of 40% to 50%. Tx associated with increased risk of in-hospital mortality, AKI, and prolonged hospital stay.
What is the most common cause of hospital-aquireed AKI?
ATN - 45%
up to 40% of in hospital pre-renal (including depletion, CRS etc)
Community-aquired 70% pre-renal
How do you define a relaspe of COP?
Worsening of symptoms
OR
New opacities/imaging changes suggestive of worsening disease
Patient presents with 6 months of weight loss and the rapid development of these skin lesions. What is this sign, and what are you concerned about?
Leser-Trelat sign - seborrheic keratoses, underlying internal cancer
Most commonly colon, breast, or stomach adenocarcinomas but has also been associated with renal, hepatic, and pancreatic malignancies.
This intern enjoys baking goods and doing puzzles
Natasha Harpalani
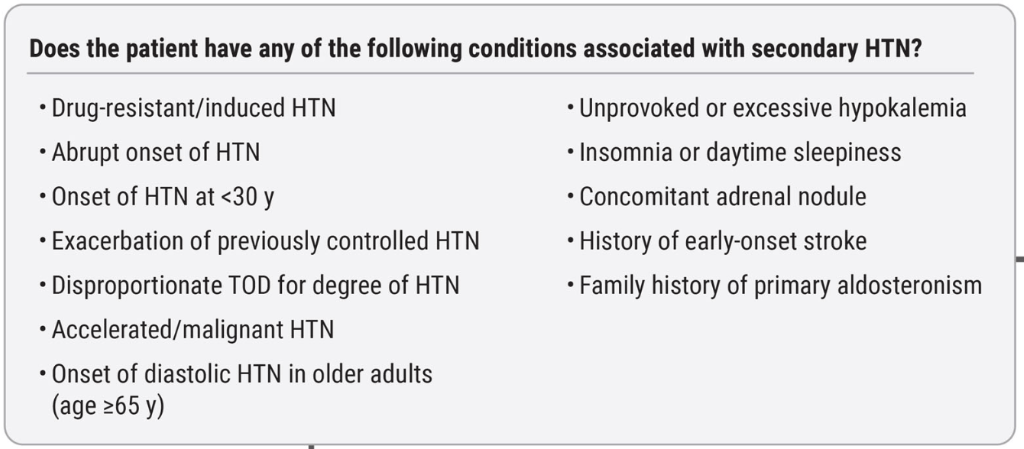
What is the lab test that should be sent on ALL patients with newly diagnosed HTN that is new in the 2025 guidelines
U Alb:Cr ratio
What antibody is associated with primary membranous nephropathy?
Anti-PLA2R - important, because if Anti-PLA2 is positive, you do not need a biopsy, and you can confidently not dig for secondary causes outside of age-appropriate cancer screenin (malignancy, autoimmune etc)
In a patient presenting with moderate or advanced idiopathic pulmonary fibrosis, what might you expect their % predicted values be for:
FEV1
FVC
TLC
DLCO
FEV1: Normal, slightly decreased
FVC: Decreased
TLC: Decreased
DLCO: Decreased
What is the empiric treatment for bacterial meningitis in a 55-year-old immunocompetent man?
Dexamethasone followed by vanc + ceftriaxone + ampicillin
Ampicillin for age > 50, immunocompromised
NNT for mortality 10 for dexamethasone, on subgroup analysis efficacy only seen in strep pneumo
This intern likes to crochet
Olivia Howland
Name 2/3 of the parameters that are in the PREVENT score, which are absent from ASCVD
eGFR
Statin use
BMI
ACE/ARB
Statin
Loop diuretic +/- thiazide
What are the three most common causes of secondary organizaning pneumonia
Infections
Drugs
Connective tissue disorders
Less common: malignancy, radiation, inhalation, transplant complication, other ILD (eosinophillic pneumonia, hypersens pneumonitis, UIP)
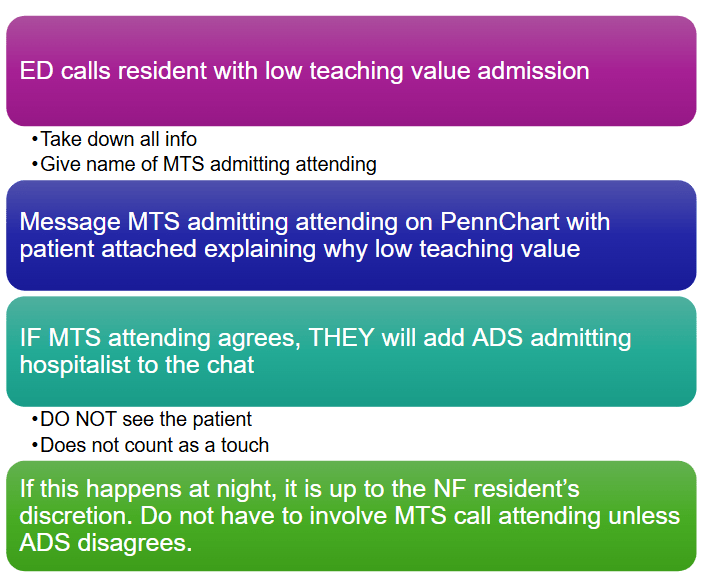
What is the process for passing admissions to ADS?
This intern does Jiu Jitsu
Daniel Youssef
In patients with newly diagnosed Stage 1 HTN, which patient populations (name 3/4) should be empirically started on anti-HTN and which patient population should be offered 3-6 months of lifestyle changes, then started on anti-HTN (if still elevated)
Primary prevention: Pre-existing CVD (CHF, CVA or CAD)
Secondary Prevention: DM, CKD or 10-yr PREVENT >7.5%
Lifestyle changes first if NONE of the above
What can you do to reduce the risk of CIN when a patient is to receive intra-arterial contrast?
Hold diuretics and NSAIDs for 24-48 hours prior to procedure
Give 6 cc/kg/hr for 6-12 hours pre AND post-procedure
Which ILD is indistinguishable from ARDS?
Acute interstitial pneumonia is clinically, radiographically, and pathologically indistinguishable from acute respiratory distress syndrome (ARDS), but patients lack risk factors for ARDS.
50% mortality, high-dose steroids used empirically, no strong evidence for or against.
What are the 3 lab cutoffs used to define empyema?
How does detection of an empyema change your management?
pH <7.2, Gluc < 60 or positive gram stain/culture
Any of three makes an empyema
NEED anaerobic coverage and likely chest tube (over serial thoras)
This intern will make you the best espresso you have ever had
Kevin Kim
What are first, second and third line pharmacological treatments for established hepatorenal syndrome?
Terlipressin + albumin
Norepi + albumin
Octreotide + midodrine + albumin (low efficacy)
What are the standard of care anti-fibrotic therapies used in idiopathic pulmonary fibrosis (2)?
Nintedenib - CAPACITY 2011, ASCEND 2014
Pirfenidone - INPULSIS 2014 + TOMORROW 2011
Decrease rate of decline of FVC. May reduce acute exacerbations. Pooled data show *may* reduce mortality.
What three things make a pulmonary embolus intermediate-high risk?
Who should you involve with most pulmonary emboli when at PMPMC?
Elevated PESI/high risk comorbidities
Signs of RHS on echo/CTA
Elevated troponin
PERT - Pulm embolus response team - no hard mortality data, but observational data show increased speed to decision and access to advanced therapies
This intern is a calisthenics guru
Farooq Sheikh