A 47-year-old woman with sarcoidosis is evaluated for an irregular pulse, a sensation of pounding in the neck, and an episode of syncope.
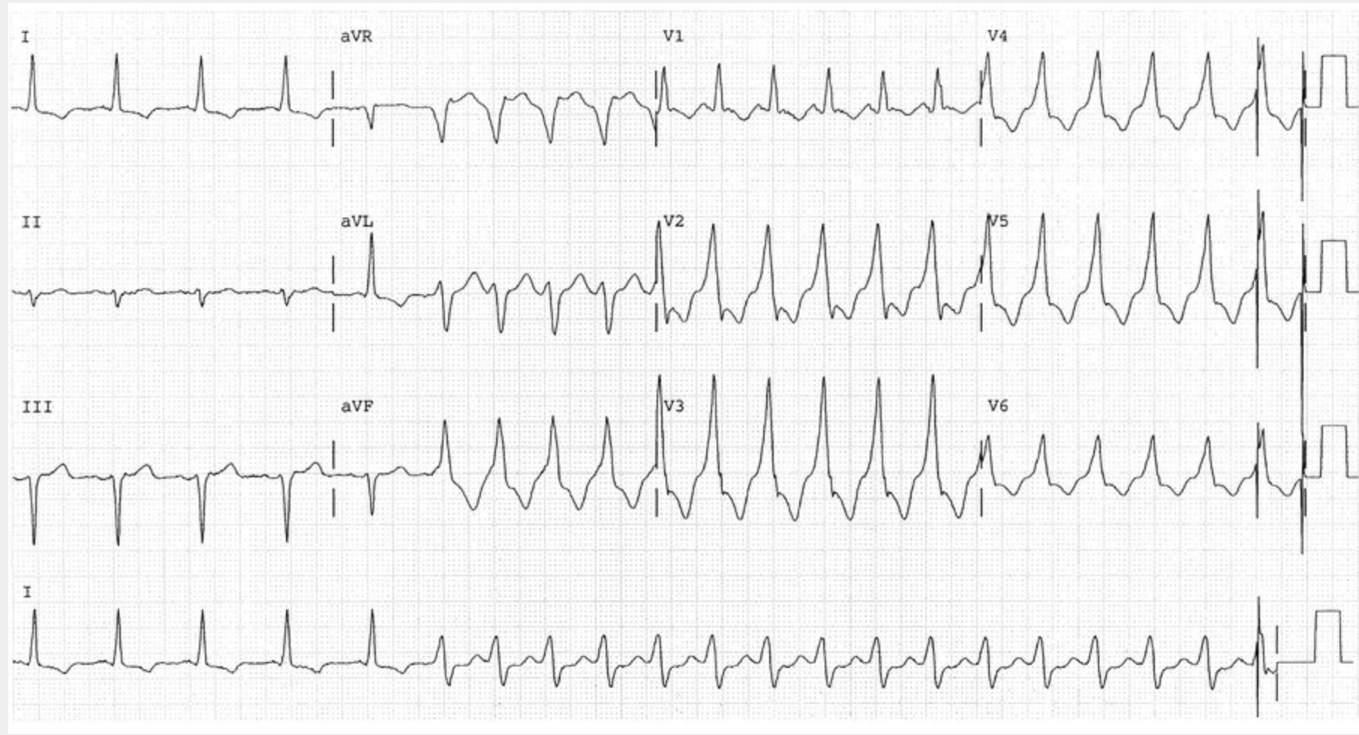
ECG is shown.
What is the diagnosis?
A. Junctional rhythm
B. Monomorphic VT
C. Polymorphic VT
D. Vfib
B. Monomorphic VT
This ECG shows ventricular tachycardia, which is typically caused by organic heart disease. It begins approximately one third of the way into the tracing and is marked by an abrupt change in axis and widening of the QRS complex. Ventricular tachycardia is characterized by fairly regular wide QRS complexes, a pulse rate of more than 120/min, and atrioventricular dissociation. Ventricular tachycardia can be characterized as either sustained (lasting >30 seconds) or nonsustained, and as monomorphic, if all of the QRS complexes have the same morphology, or as polymorphic, if the QRS pattern twists across the baseline (e.g., torsades de pointes). Ventricular tachycardia can degenerate into ventricular fibrillation.
A 20-year-old transgender male (genetic female, identifies as male) is evaluated 3 months after starting intramuscular testosterone injections. He was previously diagnosed with gender dysphoria by a psychiatrist and requested masculinizing hormone therapy. At the start of therapy, laboratory results, including complete blood count, electrolytes, and lipid panel, were normal.
Which of the following is the most appropriate test to monitor for therapy-related complications?
A. Hematocrit
B. Prolactin
C. PSA
D. Serum electrolytes
A. Hematocrit
In this transgender male undergoing masculinizing testosterone therapy, a hematocrit test (Option A) is needed to screen for erythrocytosis. Erythrocytosis (hematocrit >50%) is a known risk of testosterone therapy, and current guidelines for transgender males taking testosterone recommend hematocrit or hemoglobin measurement before starting therapy, every 3 months for the first year, then annually or semiannually. Testosterone levels should be maintained in the physiologic normal male range (320-800 ng/dL [11-28 nmol/L]) to reduce the risk for adverse events such as erythrocytosis, sleep apnea, hypertension, excessive weight gain, sodium retention, lipid changes, and cystic acne. Testosterone therapy should be reduced or the method of delivery changed if erythrocytosis occurs. In cases of severe and refractory erythrocytosis, therapy may need to be discontinued.
Hyperprolactinemia and hyperkalemia are known complications of feminizing hormone therapy (estrogen and spironolactone therapy, respectively), not testosterone. Estrogen can increase the growth of pituitary lactotroph cells, and prolactinomas have been reported in transgender females on long-term, high-dose estrogen therapy. Current guidelines recommend periodically monitoring prolactin levels (Option B) in transgender females treated with estrogen. Spironolactone competes with aldosterone for receptor sites in the distal renal tubules leading to increased sodium and water excretion while retaining potassium.
Prostate-specific antigen (Option C) should be monitored in genetic males taking testosterone therapy to treat hypogonadism because testosterone therapy can accelerate prostate cancer cell growth. Transgender males do not have a prostate; therefore, PSA monitoring is not needed in this population. Current practice guidelines recommend that cancer screening for transgender persons be based on the person's anatomy and risk factors. If cervical tissue is present, screening should be performed as recommended by current guidelines. If mastectomy is performed, annual sub- and peri-areolar breast examinations should be performed. If the patient has not had a mastectomy, screening mammography should be performed as recommended by current guidelines.
Current guidelines recommend monitoring serum electrolytes (Option D), particularly potassium, every 3 months in the first year and annually thereafter for transgender females taking spironolactone.
A 68-year-old woman is seen in consultation regarding recently diagnosed JAK2 V617F mutation–positive essential thrombocythemia. She is asymptomatic, has no other medical problems, and takes no medications.
On physical examination, vital signs are normal. The spleen is palpable 2 cm below the left costal margin.
Laboratory studies show a hemoglobin level of 13.5 g/dL (135 g/L), leukocyte count of 6000/μL (6 × 109/L), and platelet count of 685,000/μL (685 × 109/L).
Which of the following is the most appropriate treatment?
A. Aspirin
B. Hydroxyurea plus aspirin
C. Ruxolitinib
D. Stem cell transplantation
B. Hydroxyurea plus aspirin
Hydroxyurea plus aspirin is the most appropriate treatment for this patient (Option B). Her diagnosis of essential thrombocythemia (ET) is based on the presence of the JAK2 V617F mutation and elevated platelet count with normal leukocyte count and hemoglobin level. ET is a chronic myeloproliferative neoplasm, with the JAK2 mutation being the most common, occurring in approximately 50% to 60% of patients; the CAL-R mutation is seen in 25% to 35% of patients, and 5% have the MPL mutation. Patients with ET and an underlying JAK2 mutation are at higher risk for developing thrombotic complications than those with the CAL-R or MPL mutations, and aspirin is recommended in this population. Aspirin is also recommended for those older than 60 years regardless of mutation status. Cytoreductive therapy, which is aimed at decreasing the platelet count, is accepted care in those older than 60 years, as well as those with a history of thrombosis regardless of age. Cytoreductive medications include hydroxyurea, interferon, and anagrelide. Hydroxyurea is often used initially because of its tolerability and efficacy. Because the myelosuppressive effects are not specific to platelets, it is necessary to monitor for leukopenia and anemia.
Because this patient is older than 60 years, hydroxyurea should be included in the treatment plan. Aspirin alone would be insufficient (Option A).
Ruxolitinib is an oral JAK1/JAK2 inhibitor approved for use in polycythemia vera and myelofibrosis (Option C). It has been shown to be effective at reducing spleen volume and symptom burden in these diseases, but it is not approved for use in ET.
Stem cell transplantation is the only curative option in BCR-ABL–negative myeloproliferative neoplasms (Option D). However, stem cell transplantation has an associated mortality risk and significant potential morbidity. Therefore, it is not considered in patients with ET or polycythemia vera because prognosis in these diseases is generally excellent with other therapies. Stem cell transplantation is typically reserved for those with higher risk myelofibrosis whose prognosis is otherwise estimated to be poor.
In Mean Girls, Lindsay Lohan’s character wears what type of costume to the Halloween party?
She’s the bride of Frankenstein
Who wrote the 1818 classic book "Frankenstein?"
Mary Shelley
A 40-year-old woman is evaluated for hypotension. Blood pressure is 100/70 mm Hg, and pulse rate is 110/min. Heart sounds are distant. Jugular venous pressure is elevated.
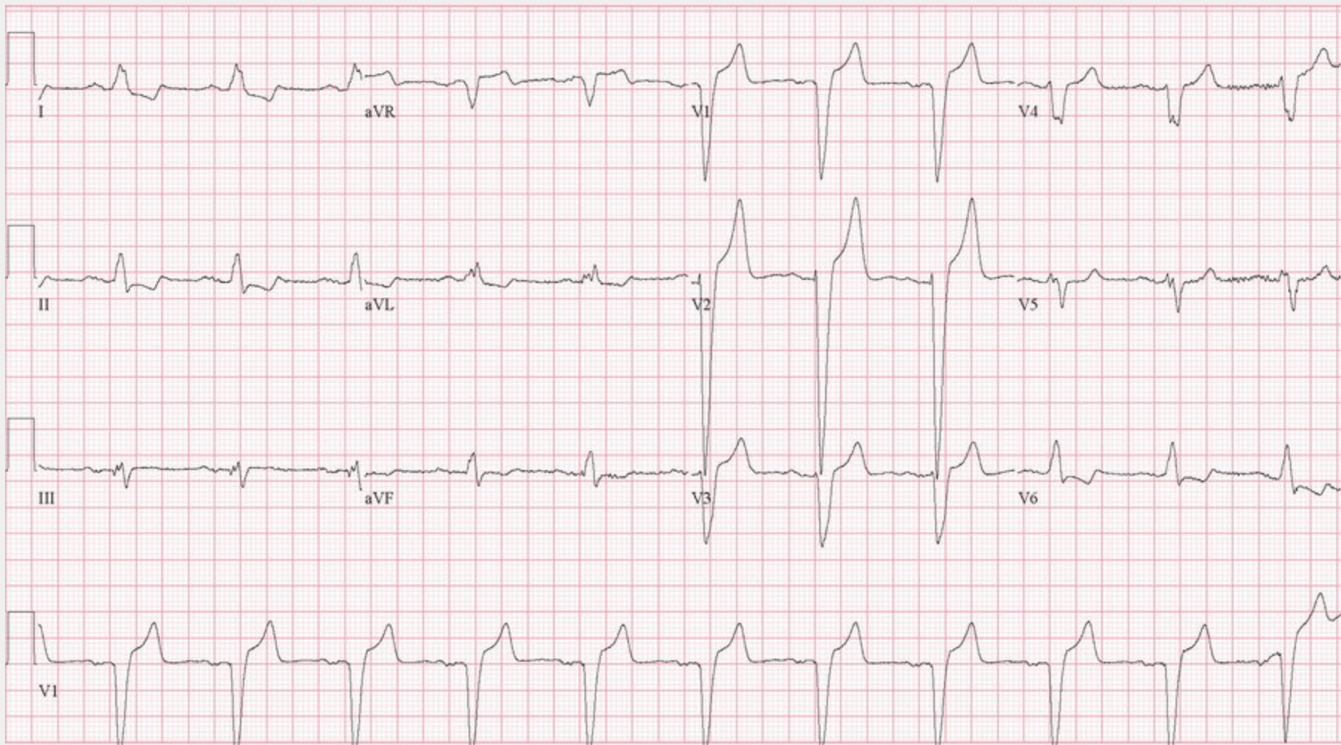
ECG is shown.
What is the most likely diagnosis?
A. Acute coronary syndrome
B. Cardiac tamponade
C. Hypertrophic cardiomyopathy
D. Pulmonary embolism
B. Cardiac tamponade
The most likely diagnosis is cardiac tamponade. This ECG demonstrates electrical alternans, a shifting of the QRS axis with each beat related to a swinging motion of the heart within the pericardial fluid. It is most clearly seen in this tracing in lead I and the precordial leads. Electrical alternans and low voltage (not seen on this ECG) are suggestive of cardiac tamponade. Clinical signs of tamponade include tachycardia, hypotension, muffled heart sounds, and elevation of the jugular venous pulse. The y descent of the jugular venous pulse may be absent because passive filling of the ventricles is impeded by the intrapericardial pressure. The cardiac silhouette is also typically enlarged on chest radiograph if the accumulation of fluid has occurred slowly.
A 75-year-old woman is evaluated in follow-up for abnormal thyroid function test results. The test was obtained to evaluate unexplained weight gain over the previous 6 months. She reports no additional symptoms such as fatigue, cold intolerance, or constipation. She has no other medical concerns.
On physical examination, pulse rate is 82/min. BMI is 26. The thyroid is normal size and without nodules.
Laboratory studies show a thyroid-stimulating hormone level of 9 μU/mL (9 mU/L) and a free thyroxine level of 1.0 ng/dL (12.9 pmol/L).
Which of the following is the most appropriate management?
A. Initiate levothyroxine
B. Measure triiodothyronine level
C. Repeat thyroid function studies in 6 to 8 weeks
D. No additional management
C. Repeat thyroid function studies in 6 to 8 weeks
The most appropriate management is to repeat the thyroid function studies in 6 to 8 weeks (Option C). This patient has subclinical hypothyroidism. Subclinical hypothyroidism is typically asymptomatic and diagnosed by a serum thyroid-stimulating hormone (TSH) level above the upper limit of the reference range and a normal free thyroxine (T4) level. It affects 5% to 10% of the general population. Transient elevation of serum TSH should be ruled out by repeating the measurement in 6 to 8 weeks. The rate of progression from subclinical to overt hypothyroidism is 2% to 4% per year, whereas normal thyroid function will spontaneously return in one third of patients. The normal range for TSH increases with age; a TSH level of up to 10 μU/mL (10 mU/L) is within the normal range for persons 80 years and older.
Initiating levothyroxine (Option A) for subclinical hypothyroidism with TSH less than 10 μU/mL (10 mU/L) should be considered in younger patients, those attempting to become pregnant, or if severe symptoms are present. This patient fulfills none of these criteria. Subclinical hypothyroidism with TSH greater than 10 μU/mL (10 mU/L) may be a risk factor for coronary artery disease and heart failure. There is no evidence that treating subclinical hypothyroidism improves quality of life, cognitive function, blood pressure, or weight; however, in patients with elevated LDL cholesterol, normalizing the TSH will lower LDL cholesterol. Overtreatment, however, is seen in more than one third of patients older than 65 years, which may increase risk for dysrhythmia and bone loss.
Measuring the triiodothyronine level (Option B) in the setting of hypothyroidism is not necessary or recommended; normal levels are maintained unless hypothyroidism is severe. TSH will become elevated in hypothyroidism first, followed by abnormalities in the T4 level.
This patient should have thyroid function tests repeated in 6 to 8 weeks to confirm the diagnosis of subclinical hypothyroidism and the need for ongoing monitoring. In this context, no additional management (Option D) is incorrect.
A 40-year-old woman is hospitalized with acute shortness of breath. Medical history is significant for two pregnancy losses in the second trimester. Laboratory testing 3 months ago after her second pregnancy loss was positive for lupus anticoagulant, high titer IgG anticardiolipin antibodies, and high titer IgG anti–β2-glycoprotein antibodies. She is otherwise well and takes no medications.
On physical examination, pulse rate is 120/min and respiration rate is 20/min; oxygen saturation is 92% breathing ambient air.
Laboratory studies show a positive lupus anticoagulant, high-titer IgG anticardiolipin antibodies, and high-titer IgG anti–β2-glycoprotein antibodies.
CT angiography shows a pulmonary embolism in the right main pulmonary artery.
Low-molecular-weight heparin is initiated.
Which of the following is the most appropriate long-term treatment?
A. Dabigatran plus aspirin
B. Rivaroxaban
C. Warfarin
D. Warfarin plus inferior vena cava filter
C. Warfarin
The most appropriate long-term treatment for this patient is anticoagulation with warfarin (Option C). She meets the criteria for antiphospholipid antibody syndrome (APLAS) based on her vascular thrombosis (acute pulmonary embolism), history of pregnancy morbidity, and laboratory criteria. Pregnancy morbidity that meets the criteria for APLAS includes at least one pregnancy loss after 10 weeks' gestation; at least one premature birth before 34 weeks' gestation because of eclampsia, preeclampsia, or placental insufficiency; or three or more unexplained consecutive spontaneous abortions before the 10th week of gestation. APLAS evaluation includes the anticardiolipin antibodies, anti–β2-glycoprotein antibodies, and lupus anticoagulant; for APLAS diagnosis, laboratory findings must include medium- or high-titer antiphospholipid antibodies on two or more occasions at least 12 weeks apart. This patient has high-risk APLAS based on triple positivity for the lupus anticoagulant, anticardiolipin antibodies, and anti–β2-glycoprotein antibodies on two occasions measured 12 weeks apart.
Emerging data from systematic reviews indicate that the use of direct oral anticoagulants, such as dabigatran, are not as effective as warfarin in the prevention of recurrent thrombotic events in patients with high-risk APLAS. Aspirin is often added to anticoagulation in patients with arterial thrombosis and in patients with a pre-existing indication for aspirin therapy such as cardiovascular or cerebrovascular disease. This patient should be treated with warfarin, not dabigatran, and has no indication for the addition of aspirin therapy (Option A).
Warfarin is the preferred anticoagulant in patients with high-risk APLAS because clinical trials have demonstrated an increased risk of thromboembolic events with rivaroxaban compared with warfarin (Option B).
Guidelines do not recommend dual therapy with an inferior vena cava filter and anticoagulation for patients with deep venous thrombosis (DVT), even for patients with proximal DVT and significant preexisting cardiopulmonary disease, as well as for patients with pulmonary embolism and hemodynamic compromise (Option D).
What do the Halloween colors black and orange symbolize?
Orange stands for harvest and warmth, and black signifies death and darkness.
A 72-year-old man is evaluated for exertional dyspnea of 1 year's duration and recent onset of orthopnea. He has diabetes mellitus, hypertension, and coronary artery disease. Medications are atorvastatin, aspirin, lisinopril, metoprolol, and metformin.
On physical examination, blood pressure is 150/82 mm Hg; the remaining vital signs are normal. Jugular venous pressure is elevated. An S3 is present. Pulmonary examination reveals occasional crackles. There is 2+ pitting edema to the knees.
A chest radiograph shows an enlarged cardiac silhouette and pulmonary vascular congestion.
An echocardiogram reveals a left ventricular ejection fraction of 20% and a right ventricular systolic pressure of 50 mm Hg.
Which of the following is the most likely cause of the patient's pulmonary hypertension?
A. Chronic thromboembolic pulm. HTN
B. Idiopathic pulmonary arterial HTN
C. Interstitial lung disease
D. Left ventricular failure
D. Left ventricular failure
The most likely diagnosis is left-sided heart failure (Option D) leading to pulmonary hypertension (PH). PH occurs when a patient's pulmonary artery pressure is elevated. Normal mean pulmonary artery pressure in adults is rarely greater than 20 mm Hg. Accordingly, the Sixth World Symposium on Pulmonary Hypertension (WSPH) has defined PH as mean pulmonary pressure greater than 20 mm Hg. The WSPH has further classified PH into five groups based on the clinical, epidemiologic, and histologic profiles. PH related to left-sided heart disease (group 2) accounts for 65% to 80% of all PH diagnoses. This patient has several risk factors that support underlying left-sided heart disease, including advanced age, history of hypertension, diabetes, and coronary artery disease. The presence of orthopnea, elevated jugular venous pressure, an S3, pulmonary congestion on chest radiography, and echocardiographic evidence of reduced ejection fraction support the diagnosis of PH related to left-sided heart disease.
Chronic thromboembolic pulmonary hypertension (CTEPH) (group 4) (Option A) is uncommon, even in patients with a history of venous thromboembolism. Approximately 20% of patients with CTEPH report no previous deep venous thrombosis or pulmonary embolism. This patient's history, physical examination, and echocardiographic findings support left-sided heart failure as the cause of PH.
In patients with pulmonary arterial hypertension (group 1) (Option B), the lung parenchyma usually appears normal on chest imaging. This patient has pulmonary vascular congestion on chest imaging.
This patient has findings of left-sided heart failure and no clinical or radiographic findings to suggest interstitial lung disease (Option C).
A 77-year-old man is evaluated following an episode of syncope. He was sitting at the breakfast table and suddenly, without prodromal symptoms, lost consciousness. He spontaneously revived after 2 minutes. There was no evidence of seizure activity. He has no chest pain or palpations.
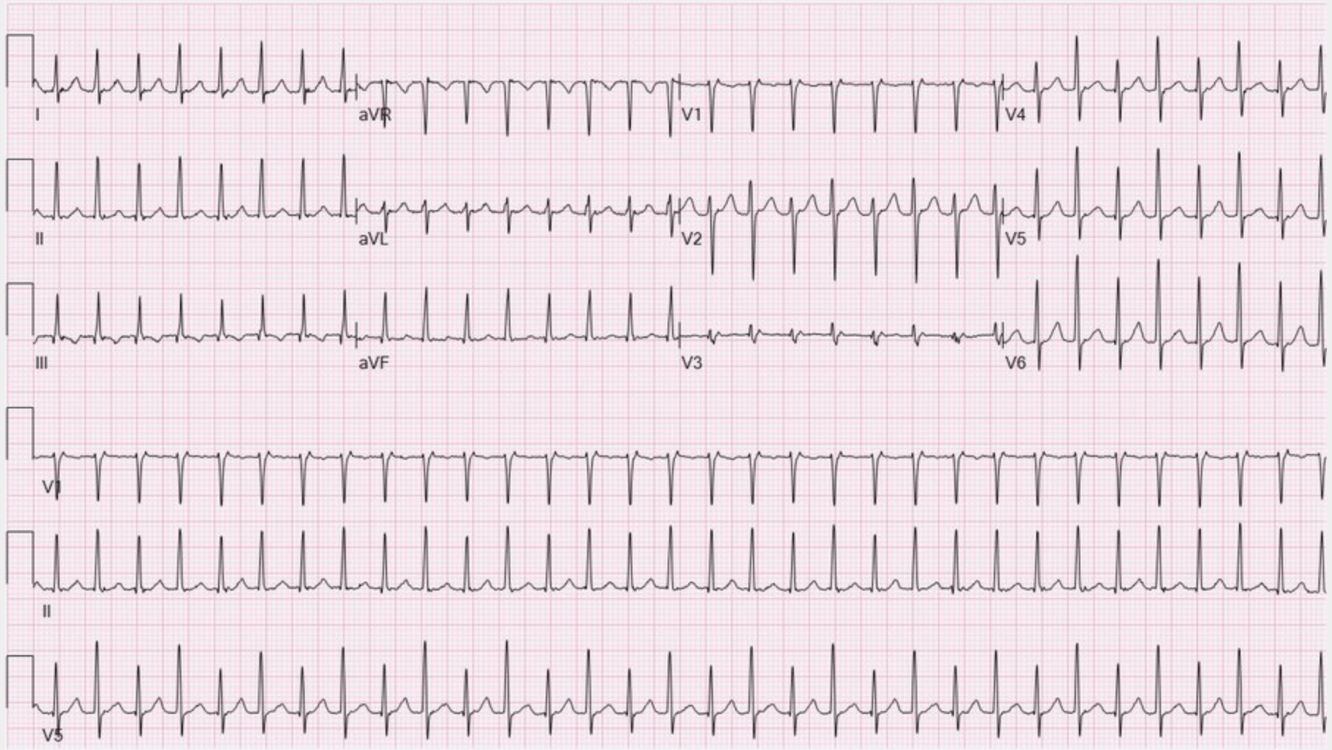
Physical examination is normal without orthostatic blood pressure changes. ECG is shown.
Which of the following is the diagnosis?
A. Afib
B. 2nd degree Mobitz Type I AV block
C. 2nd degree Mobitz Type II AV block
D. Third degree heart block
C. 2nd degree Mobitz Type II AV block
The diagnosis is second-degree Mobitz type 2 atrioventricular (AV) block (Option C). In second-degree AV block, only some P waves conduct to the ventricles. In this ECG, two nonconducted P waves are seen after the third QRS complex in the bottom rhythm strip. Mobitz type 2 second-degree AV block is typified by intermittent nonconducted P waves with unchanging PR intervals. Dizziness and syncope are major symptoms. Mobitz type 2 AV block usually occurs below the AV node and has a higher risk for progression to third-degree (complete) heart block. Regardless of symptoms, permanent pacing is indicated for second-degree Mobitz type 2 AV block, high-grade AV block, and third-degree AV block not attributable to reversible causes.
Atrial fibrillation (Option A) is defined by the presence of disorganized atrial activity with an irregularly irregular ventricular response on ECG without preceding P waves. Although this patient does have an irregularly irregular rhythm, P waves are present before all QRS complexes but not all P waves are conducted.
Mobitz type 1 second-degree (Wenckebach) AV block is characterized electrocardiographically by a PR interval that progressively prolongs until a beat is dropped, resulting in grouped beating (Option B). When 2:1 block is present, Mobitz type 2 AV block cannot be distinguished from Mobitz type 1 AV block. Most patients are asymptomatic, but if the sinus rate is slow enough, it may result in lightheadedness, syncope, presyncope, angina, or heart failure. In the absence of bradycardia, Mobitz type 1 AV block may be suggested by an irregular pulse. There are few other physical examination findings.
In third-degree AV block, no P waves conduct to the ventricles (Option D). AV dissociation is observed on the ECG; P waves bear no relationship to the QRS complexes. Most patients with complete heart block are symptomatic. Symptoms may include fatigue, dyspnea, chest pain, presyncope or syncope, and cardiac arrest.
A 70-year-old woman is evaluated for follow-up of osteoporosis, diagnosed 5 years ago. At that time, her left femur neck dual-energy x-ray absorptiometry (DEXA) T-score was -2.5. Treatment was initiated with denosumab. She has had no fractures. The most recent dose of denosumab was given 6 months ago.
Today, the left femur neck DEXA T-score is -1.8.
Discontinuation of denosumab is planned.
Which of the following is the most appropriate management?
A. Alendronate
B. Drug holiday
C. Raloxifene
D. Romosozumab
E. Teriparatide
A. Alendronate
The most appropriate choice is to start alendronate (Option A). Denosumab decreases bone turnover and increases bone mineral density (BMD), yielding robust antifracture efficacy. Optimal duration of use is unknown, but current recommendations suggest reassessing fracture risk and need for ongoing therapy after 5 to 10 years of use. This patient's fracture risk is no longer high; thus, discontinuation of denosumab is appropriate. The effects of denosumab on BMD, however, are transient, and alternative antiresorptive therapy to prevent loss of accrued BMD should be initiated on discontinuation of denosumab.
Because the efficacy of denosumab is transient, a drug holiday (Option B) strategy is not advisable, and antiresorptive therapy should be initiated after discontinuation of denosumab.
The oral bisphosphonate alendronate, initiated 6 months after the last denosumab treatment, effectively prevents bone loss during denosumab withdrawal. Although intravenous bisphosphonates may be used beginning 6 months after the last denosumab treatment, intermittent oral bisphosphonate administration throughout the period of denosumab withdrawal is advantageous. Bisphosphonates are preferentially taken up into bone at sites of active bone remodeling, making optimal timing of intravenous bisphosphonate dosing unclear.
Given its antiresorptive effects, raloxifene (Option C) could be used following denosumab withdrawal. However, it suppresses bone resorption less than bisphosphonates, and its effectiveness in this setting is unproven. Raloxifene should be avoided in patients at risk for cardiovascular disease but may be useful in women at high risk for breast cancer because it reduces the risk for invasive breast cancer.
Although romosozumab (Option D) has both bone-formative and antiresorptive effects, its bone formative effect is blunted when used subsequent to antiresorptive therapy, including denosumab. As a net anabolic drug, romosozumab would not be indicated in a patient whose bone density and fracture risk no longer justify highly potent pharmacotherapy.
Teriparatide (Option E) is effective in improving BMD and reducing fracture risk by increasing bone formation. Teriparatide combined with denosumab therapy yields greater improvement in BMD than either alone. However, teriparatide accentuates the increased bone resorption and rapid loss of BMD associated with denosumab withdrawal; thus, it should not be substituted for denosumab.
A 65-year-old woman is hospitalized with a diagnosis of multiple segmental pulmonary emboli in the right and left lungs. Medical history is otherwise unremarkable. Her only medication is estrogen-medroxyprogesterone hormone replacement, which has been discontinued.
On physical examination, blood pressure is 124/64 mm Hg, pulse rate is 124/min, and respiration rate is 24/min. Oxygen saturation is 93% breathing ambient air. Examination findings are otherwise noncontributory.
Complete blood count and metabolic profile are normal. Estimated glomerular filtration rate is greater than 60 mL/min/1.73 m2.
Which of the following is the most appropriate treatment?
A. Apixaban
B. Inferior vena cava filter placement
C. Thrombolytic therapy
D. Unfractionated heparin
A. Apixaban
The most appropriate treatment for this patient is apixaban (Option A). Furthermore, she has a score of 1 (pulse rate ≥110/min) on the simplified Pulmonary Embolism Severity Index (PESI), which places her at high risk for adverse outcomes and necessitates treatment in the hospital. Apixaban is a direct factor Xa inhibitor that is approved to treat acute venous thromboembolism (VTE) without concomitant parenteral therapy on initiation; it can be used in patients with kidney injury and does not require dose adjustment for VTE treatment, even in patients undergoing dialysis. Rivaroxaban, another direct factor Xa inhibitor, would also be a treatment option for this patient. For patients with VTE, the American Society of Hematology (ASH) suggests using direct oral anticoagulants (DOACs), such as apixaban, rivaroxaban, dabigatran, and edoxaban, over vitamin K antagonists, such as warfarin. Dabigatran and edoxaban, like warfarin, require a transition period with parenteral therapy before continuing the oral treatment.
For patients with VTE and significant preexisting cardiopulmonary disease, as well as for patients with pulmonary embolism (PE) and hemodynamic compromise, the ASH guideline suggests anticoagulation alone rather than anticoagulation plus insertion of an inferior vena cava (IVC) filter; the guideline also suggests that an IVC filter may be considered in patients with an absolute contraindication to anticoagulation. This patient has no contraindication to anticoagulation, so an IVC filter would not be indicated (Option B). Studies have shown that, in patients with severe PE, the use of an IVC filter with anticoagulation does not lead to a reduction in symptomatic recurrent PE compared with anticoagulation alone, so it should not be recommended in this patient.
Thrombolytic therapy is generally recommended in the setting of massive PE resulting in shock, hypotension, or severe cardiac compromise (profound bradycardia or pulselessness) (Option C). For patients with PE and echocardiographic evidence or biomarkers compatible with right ventricular dysfunction without hemodynamic compromise (submassive PE), the ASH guideline suggests anticoagulation alone instead of thrombolytic therapy and anticoagulation. The 2021 CHEST guideline recommends against thrombolytic therapy in most patients with acute PE not associated with hypotension. This patient does not have massive PE, so thrombolytic therapy would not be appropriate.
Parenteral therapy with unfractionated heparin (UFH) is not preferred, because variations in bioavailability and potential delay in arriving at a therapeutic dose are more likely than with low-molecular-weight heparin (LMWH) or a DOAC (Option D). UFH should therefore be reserved for patients for whom LMWH is contraindicated or in those who require anticoagulation that can be stopped quickly, generally in anticipation of an invasive procedure or surgery.
Halloween was celebrated for the first time ever in the United States in what year?
A. 1820s
B. 1840s
C. 1920s
D. 1940s
B. 1840s
When was the song "Monster Mash" released?
1962
An 84-year-old man is evaluated during a routine physical examination. His only concern is a gradual loss of stamina and low energy. He can no longer complete his routine 2-mile run without stopping to rest with a prolonged recovery time. He has hypertension, for which he takes lisinopril.
On physical examination, blood pressure is 125/78 mm Hg and pulse rate is 52/min. Heart rate is regular. The remainder of the examination is unremarkable.
Laboratory studies are within normal limits, including a recent thyroid-stimulating hormone measurement.
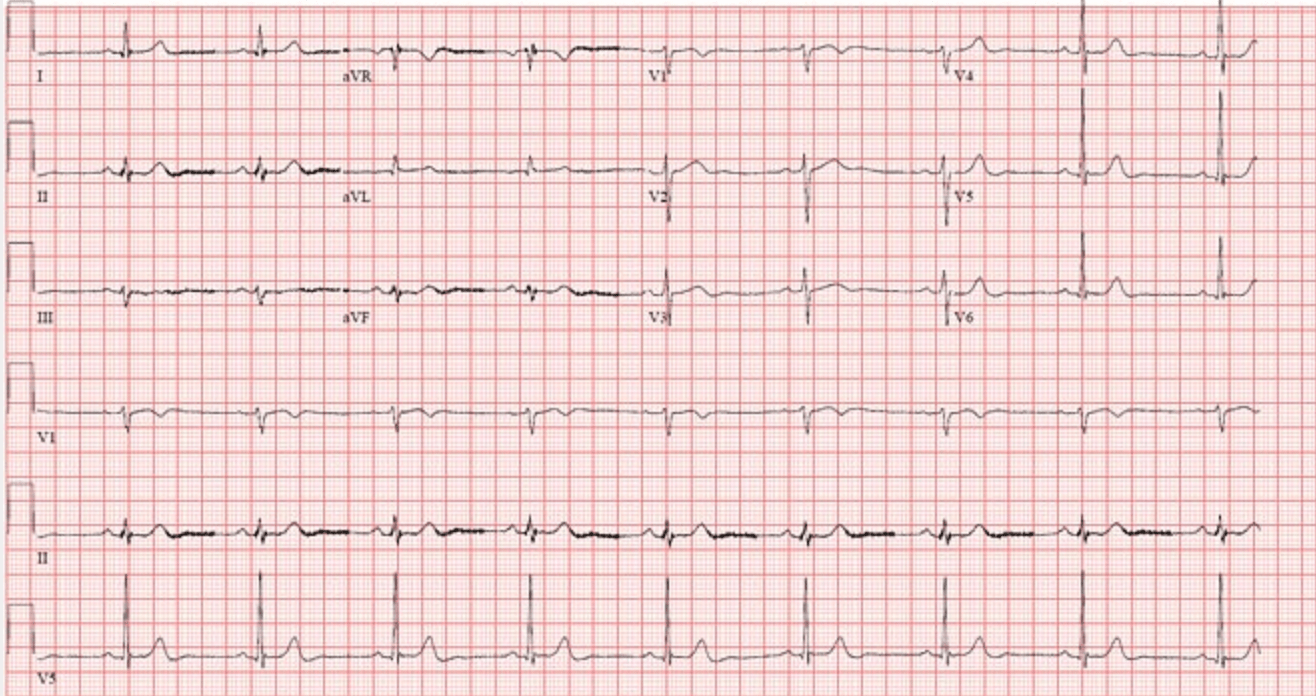
ECG is shown. Ambulatory 48-hour ECG monitoring shows a maximum heart rate of 72/min during vigorous aerobic activity. An echocardiogram and exercise stress test performed 1 year ago for chest pain revealed normal left ventricular function and no ischemia, with appropriate augmentation of heart rate.
Which of the following is the most appropriate management?
A. Hospital admission
B. Pacemaker implantation
C. Switch lisinopril to amlodipine
D. Reassurance and clinical monitoring
B. Pacemaker implantation
Pacemaker implantation (Option B) is the most appropriate next step in management for this patient who presents with signs and symptoms of sinus node dysfunction. Common indications for permanent pacemaker implantation include symptomatic bradycardia without reversible cause; permanent atrial fibrillation with symptomatic bradycardia; alternating bundle branch block; and complete heart block, high-degree atrioventricular (AV) block, or Mobitz type 2 second-degree AV block, irrespective of symptoms. This patient is bradycardic at baseline, does not mount a tachycardic response to activity on ambulatory ECG monitoring, and has low energy. There is no threshold that defines an inadequate heart rate response; it is determined by symptoms suggesting that the heart rate is not meeting the patient's physiologic demands. A common challenge among these patients, many of whom are older, is differentiating between age-related decline in physical activity and pathologic, symptomatic sinus node dysfunction. The former is less likely to improve with cardiac pacing, and the latter often improves dramatically. In this case, the patient is very active, with distinct loss of energy and ECG findings of sinus bradycardia. Recent stress test results confirm normal left ventricular function and no ischemia; thus, cardiac pacing is the next appropriate step.
Patients with sinus node dysfunction are rarely unstable, but if there is evidence of hemodynamic instability, hospitalization (Option A) is indicated. Warning signs and symptoms of hemodynamic instability warranting hospitalization include hypotension, altered mental status, ischemic chest pain, and acute heart failure. This patient's condition is not acute or dangerous, and thus inpatient care is not warranted.
Lisinopril is unlikely to be contributing to this patient's bradycardia, although his hypertension is likely a risk factor for sinus node dysfunction. Although amlodipine is a dihydropyridine calcium channel blocker, use of this drug may actually worsen bradycardia; therefore, switching lisinopril to amlodipine (Option C) is not indicated.
Reassurance with ongoing monitoring (Option D) is not appropriate, because it is likely that this patient's loss of energy is pathologic and related to symptomatic bradycardia.
A 30-year-old woman is evaluated for fatigue and abdominal pain of 4 months' duration. She has lost 2.3 kg (5.1 lb) during that time. She has no other medical problems and takes no medications.
On physical examination, blood pressure is 110/72 mm Hg sitting and 90/62 mm Hg standing. Pulse rate is 70/min sitting and 88/min standing. Remaining vital signs are normal. BMI is 19. The patient has intensely tanned skin and hyperpigmented buccal mucosa and palmar creases. Visual field testing is normal.

Which of the following is the most appropriate next step in management?
A. Cosyntropin stimulation test
B. Hydrocortisone plus fludrocortisone
C. Pituitary MRI
D. Prednisone
E. Serum aldosterone
B. Hydrocortisone plus fludrocortisone
The most appropriate management is to treat with hydrocortisone twice daily and fludrocortisone once daily (Option B). This patient has primary adrenal insufficiency, as evidenced by the combination of her low morning serum cortisol and elevated adrenocorticotropic hormone level. The most common cause of primary adrenal insufficiency is autoimmune destruction of all layers of the adrenal cortex, which leads to progressive mineralocorticoid, glucocorticoid, and adrenal androgen deficiency. Most patients have positive 21-hydroxylase antibodies, and approximately 50% develop another autoimmune endocrine disorder in their lifetime, such as celiac disease, thyroid disease, or type 1 diabetes mellitus. Given that this patient has primary adrenal insufficiency, she requires both glucocorticoid and mineralocorticoid therapy. The preferred glucocorticoid for treatment of adrenal insufficiency is hydrocortisone two or three times daily to better mimic the circadian rhythm of endogenous cortisol secretion. The higher dose of hydrocortisone is given in the morning (typically 10-15 mg), and the lower dose is given in the afternoon (approximately 5 mg).
Although the cosyntropin stimulation test (Option A) is often used to diagnose adrenal insufficiency, in this patient, the diagnosis has already been confirmed by a morning serum cortisol level of less than 3 μg/dL (83 nmol/L). As a result, a cosyntropin stimulation test is not required for diagnosis and will not change management.
Given the high adrenocorticotropic hormone level, which indicates that pituitary function is intact, the etiology is confirmed to be primary and not secondary (central) adrenal insufficiency. Therefore, a pituitary MRI (Option C) is not indicated.
Adherence to multiple daily doses of hydrocortisone can be challenging. Once-daily prednisone (Option D) can be used as an alternative, but it also must be combined with fludrocortisone. Prednisone alone would not provide adequate mineralocorticoid replacement.
Serum aldosterone measurement (Option E) is not required to diagnose primary adrenal insufficiency, especially because this patient already has hyperkalemia and hyponatremia, which suggest aldosterone deficiency.
A 75-year-old man is evaluated for an elevated INR found on routine monitoring. He is otherwise well and has no evidence of bleeding. Medical history is significant for atrial fibrillation. His only medication is warfarin.
Laboratory studies show a normal hemoglobin level and INR of 8.5.
The patient is instructed not to take his warfarin until further INR evaluation.
Which of the following is the most appropriate additional management?
A. 4-factor prothrombin complex concentrate
B. Factor VIIa
C. Fresh frozen plasma
D. Vitamin K
E. Observation
E. Observation
The most appropriate management of this patient in addition to withholding warfarin is observation (Option E). He has an elevated INR on routine laboratory testing but no signs or symptoms of bleeding. Bleeding risk increases as the INR increases. Additionally, patients older than 75 years, those with previous cerebrovascular accidents, and those with previous gastrointestinal bleeding are at increased risk of bleeding independent of the INR. Bleeding risk is elevated to a higher degree in patients taking concomitant aspirin, clopidogrel, or other antiplatelet agents. If a patient's INR is between 4.5 and 10, warfarin must be withheld until the INR returns to the therapeutic range; without bleeding, no other treatment is required, and observation is recommended. If the INR is greater than 10 without any bleeding, then vitamin K is recommended in addition to withholding warfarin (Option D). In any patient taking warfarin with an elevated INR who presents with life-threatening bleeding, then warfarin is withheld, and vitamin K and a prothrombin complex concentrate (PCC) should be administered (Option A). The PCC may be 3-factor (containing factors II, IX, and X) or 4-factor (containing factors II, VII, IX, and X), although 4-factor PCC is preferred because of more predictable warfarin reversal.
Factor VIIa is used to treat bleeding in patients with hemophilia (Option B). It plays no role in warfarin reversal.
Fresh frozen plasma (FFP) is not the preferred agent when treatment of life-threatening bleeding is necessary for a patient with a supratherapeutic INR (Option C). 4-Factor PCC has been found to be noninferior to FFP in the treatment of life-threatening bleeding. Additionally, 4-factor PCC has a faster infusion time, more rapid reversal of INR, and lower risk of volume overload. For these reasons, 4-factor PCC is the preferred agent for warfarin reversal when a reversal agent is necessary.
In The Nightmare Before Christmas, what was Oogie Boogie made of?
He was a burlap sack filled with spiders, insects, and a snake for a tongue.
A 73-year-old woman is hospitalized for progressive dyspnea. Six months ago, she developed chronic sinusitis and nose bleeds. Four months ago, a persistent dry chronic cough developed, followed by myalgia and distal paresthesia. She has lost 13.6 kg (30 lb).
On physical examination, temperature is 38.2 °C (100.8 °F), blood pressure is 148/96 mm Hg, pulse rate is 104/min, respiration rate is 24/min, and oxygen saturation is 94% with the patient breathing ambient air. Dry crackles are heard at the lung bases. There is loss of sensation to light touch in the left foot. Numerous small palpable red-purple lesions are present on the lower legs.
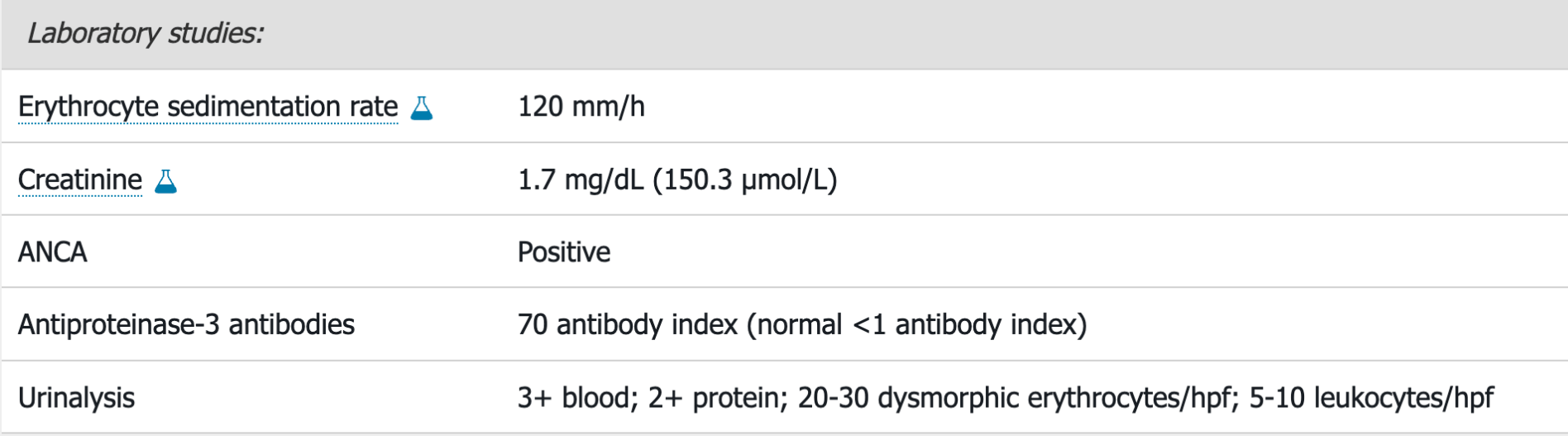
Chest radiograph shows peripheral pulmonary parenchymal opacities. Chest CT scan shows multiple opacities and nodules throughout both lungs.
Kidney biopsy results are pending.
High-dose glucocorticoids are started.
Which of the following will most likely be the appropriate additional treatment?
A. Azathioprine
B. Methotrexate
C. Mycophenolate mofetil
D. Rituximab
D. Rituximab
The most appropriate treatment is high-dose glucocorticoids and rituximab (Option D). This patient has granulomatosis with polyangiitis (GPA). ANCA-associated vasculitis is suggested by the severe and inflammatory multisystemic illness. Clues that this is GPA specifically include sinus, kidney, and lung involvement; the skin findings (palpable purpura is not specific for GPA but strongly suggests a small-vessel vasculitis); peripheral nervous system involvement (left foot sensory loss); and the presence of antiproteinase-3 antibodies. To confirm the diagnosis and guide management, tissue biopsy (in this case, kidney) may be done if possible. High-dose glucocorticoids plus either rituximab (preferred) or cyclophosphamide is the appropriate treatment for induction of remission in severe organ-threatening or life-threatening GPA. Selected patients may benefit from plasma exchange. Once remission is achieved, patients should receive maintenance therapy consisting of rituximab, methotrexate, or azathioprine; rituximab appears to be most effective for preventing relapse and is guideline preferred. On their own, high-dose glucocorticoids are not sufficient for induction and maintenance treatment of ANCA-associated vasculitis. Mortality rates in patients receiving only glucocorticoids are high. Observational studies from the 1970s and 1980s demonstrated that glucocorticoids plus cyclophosphamide was associated with a significant improvement in survival, five times that of historical controls, and a lower frequency of relapse.
Glucocorticoids plus azathioprine (Option A) is not adequate for inducing remission of GPA. Azathioprine has been used to maintain remission once achieved (although rituximab is superior for maintenance of remission), but this combination has never been shown to induce remission in active ANCA-associated vasculitis.
Although glucocorticoids plus methotrexate (Option B) are preferred for active, nonsevere GPA, this patient has severe systemic GPA and therefore requires high-dose glucocorticoids plus rituximab.
Although glucocorticoids plus mycophenolate mofetil (Option C) can induce remission in ANCA-associated vasculitis, patients treated with this therapy have a higher rate of relapse than those treated with glucocorticoids plus rituximab. Because ANCA-associated vasculitis is a chronic condition, the treatment least associated with relapse is the most preferable.
A 66-year-old woman is evaluated for a 6-month history of right shoulder pressure that occurs after walking half a mile and improves with 5 minutes of rest. She has no dyspnea, nausea, or fatigue. The frequency and duration of her symptoms have not changed. Her history is otherwise unremarkable.
On physical examination, vital signs are normal. BMI is 33. Other than a paradoxically split S2, the cardiac examination is normal. The lungs are clear to auscultation.
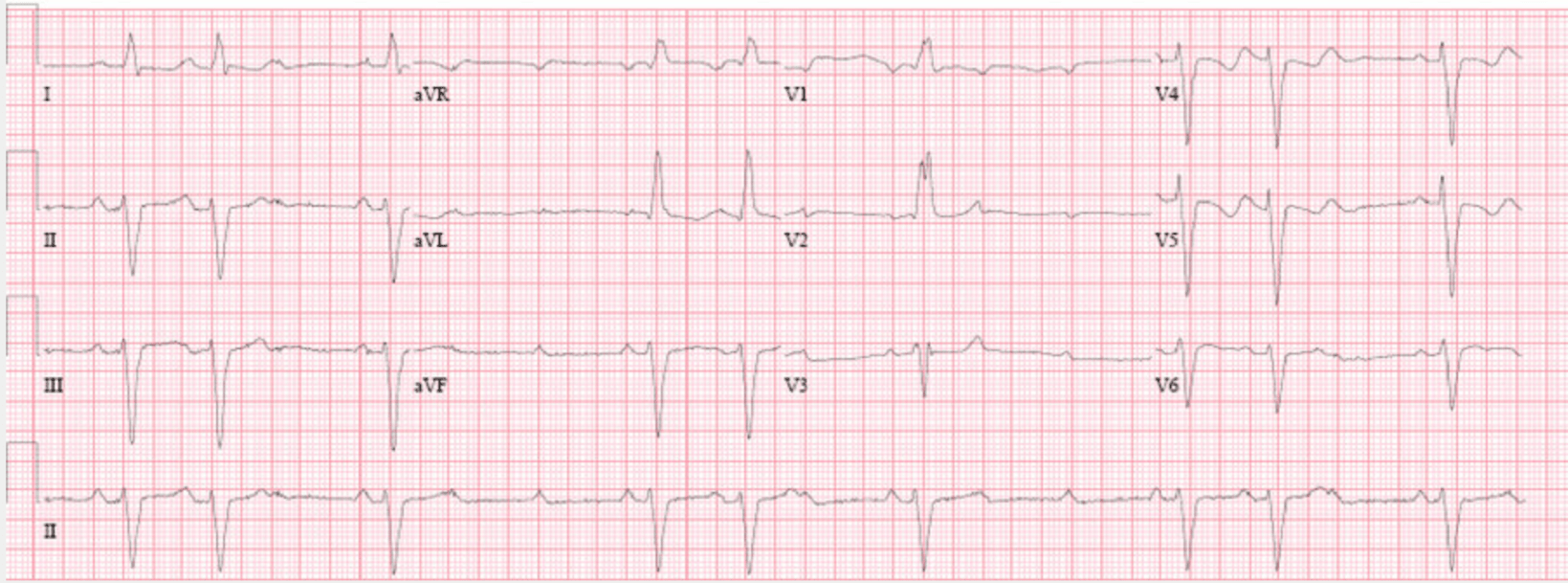
A chest radiograph is normal. ECG is shown.
What is the most appropriate next best step?
A. coronary angiography
B. Exercise ECG
C. Pharmacologic myocardial perfusion imaging
D. Transthoracic echocardiography
E. No further testing is required
C. Pharmacologic myocardial perfusion imaging
Pharmacologic myocardial perfusion imaging (Option C) is the most appropriate next test. The evaluation of angina should include a physical examination to detect conditions that may mimic symptomatic coronary artery disease (CAD), as well as a focused history to assist in determining the pretest probability of CAD. A resting ECG is required to evaluate for ongoing ischemic insult and to guide the choice of subsequent diagnostic testing. This 66-year-old woman with clinical features of possible angina has an intermediate pretest likelihood of CAD, an indication for stress test diagnostic evaluation. In addition to its role as a first-line test in the evaluation of possible CAD, stress testing with imaging is indicated in patients with an inability to exercise, baseline ECG abnormalities (such as left bundle branch block [LBBB]) that limit interpretation of the exercise ECG, or indeterminate findings on the exercise ECG. In patients able to exercise but with underlying LBBB, such as this patient, pharmacologic stress testing with imaging (myocardial perfusion, cardiac magnetic resonance, or echocardiographic) is appropriate to reduce the rate of false-positive test results associated with exercise ECG (Option B) in this population.
Coronary angiography (Option A) is not indicated for stable, low-risk clinical features. It should be reserved for patients with a high pretest likelihood of CAD and unstable symptoms, or for those in whom optimal medical therapy has been ineffective.
Resting transthoracic echocardiography (Option D) can provide helpful prognostic information related to ventricular function and is useful in assessing for noncoronary cardiac causes of chest pain. It is not as helpful as exercise stress testing as an initial test for symptomatic CAD.
Reassurance without additional testing (Option E) may be appropriate when an alternative cause of chest discomfort has been identified in a patient with a low pretest probability of CAD, but this patient's ongoing exertional chest pain and intermediate likelihood of CAD require further investigation.
A 30-year-old woman is evaluated for a 2-month history of anorexia, insomnia, palpitations, diarrhea, and an 11-kg (24.0-lb) weight loss. She reports no neck pain. She has been well otherwise and takes no medications.
On physical examination, temperature is 37.9 °C (100.0 °F), blood pressure is 90/58 mm Hg, and pulse rate is 101/min. BMI is 18. The thyroid is firm and not enlarged, with the left lobe larger than the right. No proptosis, thyroid nodules, or adenopathy are noted, and no thyroid tenderness is present.
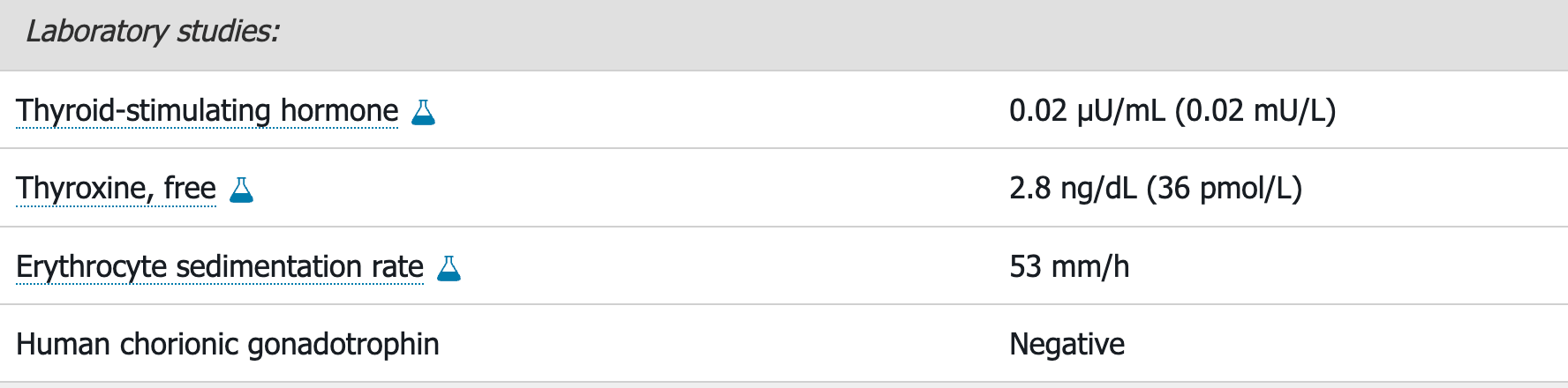
The radioactive iodine uptake scan is shown. Uptake at 24 hours is 0.3%.
Which of the following is the most appropriate treatment?
A. Atenolol
B. Methimazole
C. Prednisone
D. Propylthiouracil
A. Atenolol
The most appropriate treatment is atenolol (Option A). This patient presents with symptoms of thyrotoxicosis. Laboratory studies show suppressed thyroid-stimulating hormone (TSH) level and elevated free thyroxine (T4) level. Examination shows a firm nonenlarged thyroid. Thyroid scintigraphy with radioactive iodine uptake (RAIU) is used to distinguish between the hyperthyroidism produced by Graves disease or toxic nodular goiter and thyrotoxicosis of destructive thyroiditis. RAIU is high (above 30%) or inappropriately normal in hyperthyroidism due to Graves disease and low (less than 10%) in other causes of thyrotoxicosis such as destructive thyroiditis. Defining the cause of thyrotoxicosis helps dictate the use of antithyroid medications (methimazole or propylthiouracil), symptomatic treatments (β-blockers), or anti-inflammatory treatments (prednisone, NSAIDs).
The radioactive iodine uptake at 24 hours is low, indicating that the iodine uptake is appropriate for the low TSH (the thyroid is not functioning autonomously as seen in Graves disease). Thyroiditis is also supported by the lack of proptosis seen in Graves disease and the elevated erythrocyte sedimentation rate. Thyrotoxicosis occurs in destructive thyroiditis as a result of unregulated release of preformed thyroid hormone from thyroid follicles damaged by inflammation. Thyroiditis typically has three phases: thyrotoxic, hypothyroid, and return to euthyroidism. The first two phases can last up to 3 months each. Symptomatic thyroiditis is treated with β-blockers for tachycardia and palpitations and anti-inflammatory treatments (prednisone, NSAIDs) for thyroid tenderness and pain. Most patients with thyrotoxicosis benefit from β-blockers to reduce adrenergic symptoms rapidly. Atenolol and metoprolol are preferred because of once-daily dosing and their cardioselective nature.
Because this patient does not have Graves disease, methimazole (Option B) is not indicated.
Prednisone (Option C) is only indicated in patients with thyroiditis if symptoms included thyroid tenderness. This patient has no indication for prednisone.
Propylthiouracil (Option D) is also not indicated because this patient does not have Graves disease.
A 55-year-old man is hospitalized for confusion and abdominal pain. Medical history is notable for alcohol-related liver disease. He takes lactulose and spironolactone.
On physical examination, the patient is somnolent but arousable. Temperature is 37.7 °C (99.9 °F), blood pressure is 90/50 mm Hg, pulse rate is 110/min, and respiration rate is 17/min. Ecchymoses are noted on the upper and lower extremities. Ascites is present, and the abdomen is diffusely tender on palpation.
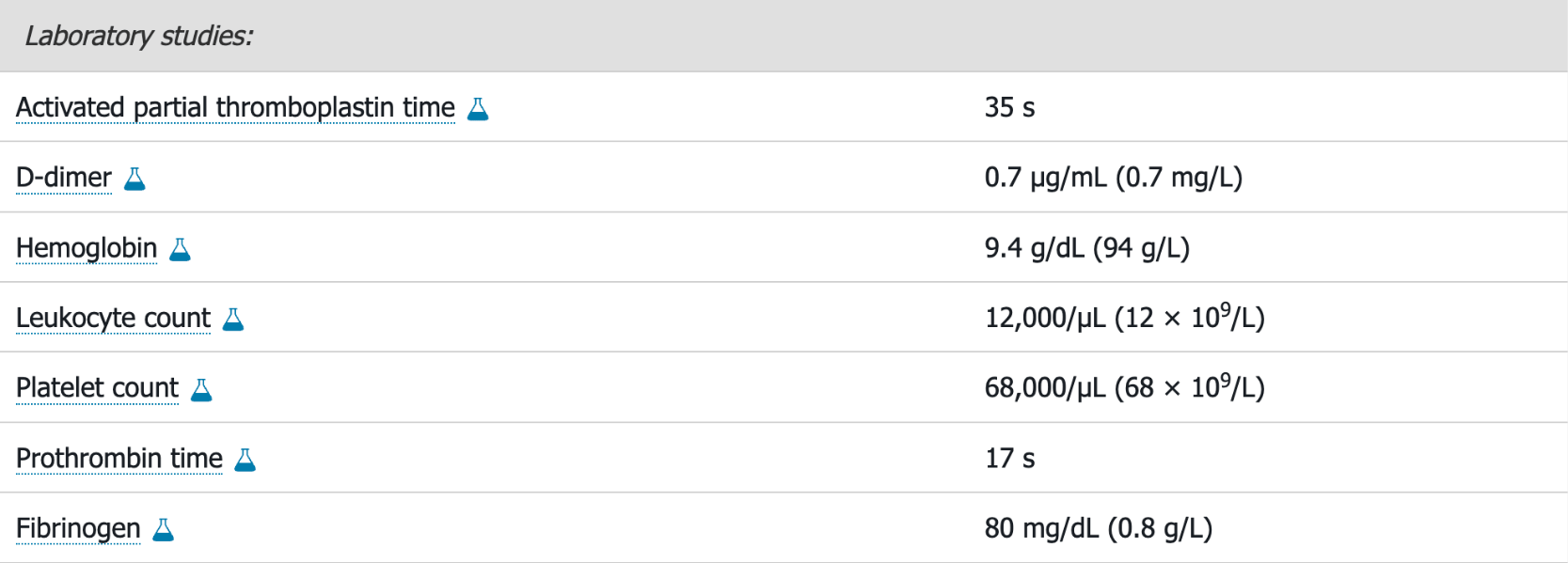
Abdominal ultrasonography demonstrates a nodular appearance of the liver, moderate splenomegaly, and large amount of ascites. Paracentesis confirms a diagnosis of spontaneous bacterial peritonitis, and treatment is initiated.
Which of the following tests will be most helpful in the evaluation of the patient's coagulopathy?
A. Factor II level
B. Factor VIII level
C. Factor X level
D. Thrombin time
B. Factor VIII level
The most appropriate test to evaluate the patient's coagulopathy is the factor VIII level (Option B). In addition to thrombocytopenia, the patient has a coagulopathy as evidenced by the prolonged coagulation studies, low fibrinogen level, and elevated D-dimer level. The main diagnostic considerations for his thrombocytopenia and coagulopathy include liver disease and disseminated intravascular coagulation (DIC). Laboratory overlap between these diagnoses is considerable, making it difficult to differentiate them on testing alone. Additionally, they are often present simultaneously, and treatment considerations are heavily influenced by the overall clinical picture. Distinguishing between liver disease and DIC may be challenging, but measuring the factor VIII activity is a theoretical means of separating these disorders. Factor VIII is often normal or elevated in patients with liver disease because factor VIII is produced in hepatic and nonhepatic endothelial cells; however, factor VIII is consumed in DIC. A normal or elevated factor VIII level will support liver disease as the cause of this patient's coagulopathy.
Factors II and X are reduced in liver disease, vitamin K deficiency, and DIC (Options A, C). Measuring these levels would not be helpful in evaluating this patient's coagulopathy.
Thrombin time measures the final step in coagulation (conversion of fibrinogen to fibrin) by measuring the time to fibrin clot formation (Option D). This test will be prolonged in the presence of heparin, low fibrinogen level, or abnormal fibrinogen (dysfibrinogenemia) but is normal in patients with pure vitamin K deficiency. A thrombin time will not distinguish between coagulopathy from DIC or liver disease, because the fibrinogen level is characteristically low, resulting in prolongation of the thrombin time, in both conditions.
What are some of the most popular Halloween candy options in the United States?
1. M&M's
2. Reese's cups
3. skittles
4. snickers
5. candy corn
6. Hershey kisses
7. tootsie pops
JK Rowling stated that Lupin was one of her favorite characters in the Harry Potter series. Lupin being a werewolf was used to explain as a metaphor for which illness that had stigmas associated with them in the real world.
What was that illness?
HIV/AIDs