Which phase signifies expiration on waveform capnography?
1. Phase 0
2. Phase 1,2
3. Phase 2,3
4. Phase 3
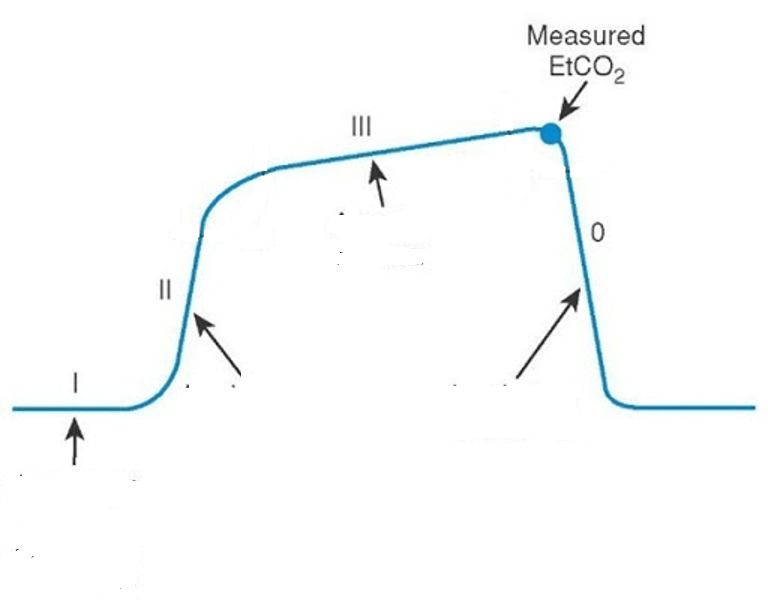
What is phase II and III?
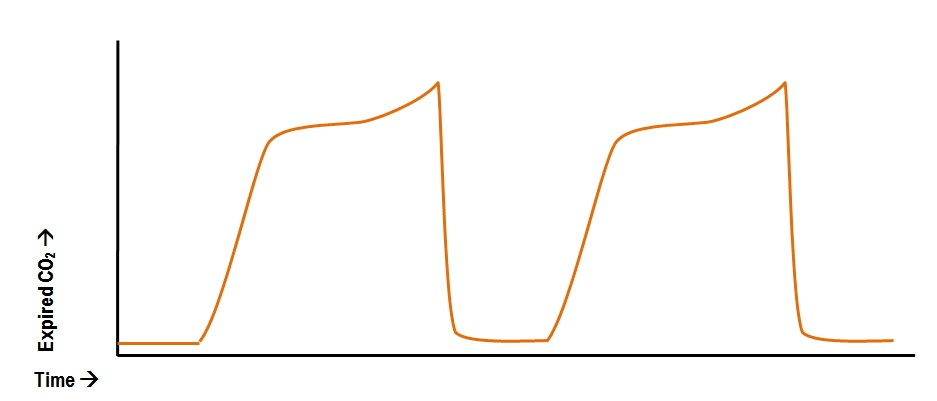
Capnography phases:
Phase I: The inspiratory baseline, which reflects inspired air that is normally devoid of CO2. This phase is a flat line at or very close to zero.
Phase II: The expiratory upstroke, which is the transition between dead space to alveolar gas. There is a rapid increase in PECO2, which represents exhalation of mixed air.
Phase III: The alveolar plateau, which reflects the alveolar expiratory flow. PECO2 is close to alveolar carbon dioxide tension (PACO2).
You are called to the bedside due to the ventilator alarming. Describe the wave form.
What is double triggering?
Double triggering is defined as two ventilator insufflations delivered within one patient inspiratory effort. The root cause for this dyssynchrony is a disproportionately shorter inspiratory time (I‑time) of the mechanical breath in comparison to patient neural I‑time. Other causes include patient-ventilator asynchrony, specifically insufficient pressure support during the inspiratory phase. The resultant premature cycling of the first breath can result in accidental delivery of a subsequent second breath during a single inspiratory activation.
Which part of Virchow's triad is most commonly involved in PE provoked by 14 hour international flight ?
What is venous stasis?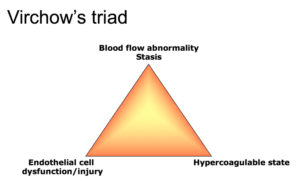
Virchow's triad is a model that describes three factors that contribute to the formation of blood clots, including venous stasis, which is altered blood flow
- Venous stasis: A type of altered blood flow which is a key component of Virchow's Triad, occurs when blood flow slows or becomes stagnant, increasing the risk of clot formation.
- Endothelial injury: The endothelium maintains anticoagulant and anti-platelet properties through glycoproteins like thrombomodulin and tissue factor, which are involved in regulating coagulation and minimizing thrombosis. Endothelial damage leads to the release of these molecules into the bloodstream, increasing thrombosis.
- Hypercoagulable state: Involves an increased tendency for thrombus due to genetic factors, malignancy, pregnancy or hormone therapy.
Venous stasis is considered the most important factor, when combined with vascular injury or hypercoagulability, the risk of thrombus increases significantly.
When is prone ventilation indicated?
"What is P:F ratio <150"
It is recommended for severe ARDS with PO₂/FIO₂ <150 mm Hg to improve oxygenation and lung protection.
Found no significant differences in 90-day mortality or ventilator-free days between cisatracurium and usual care.
What is the ROSE trial?
Patients with moderate-to-severe ARDS were randomized to receive either early continuous cisatracurium infusion with deep sedation (intervention group) or usual care with lighter sedation (control group). The control group received lighter sedation and higher PEEP compared to ACURASYS.
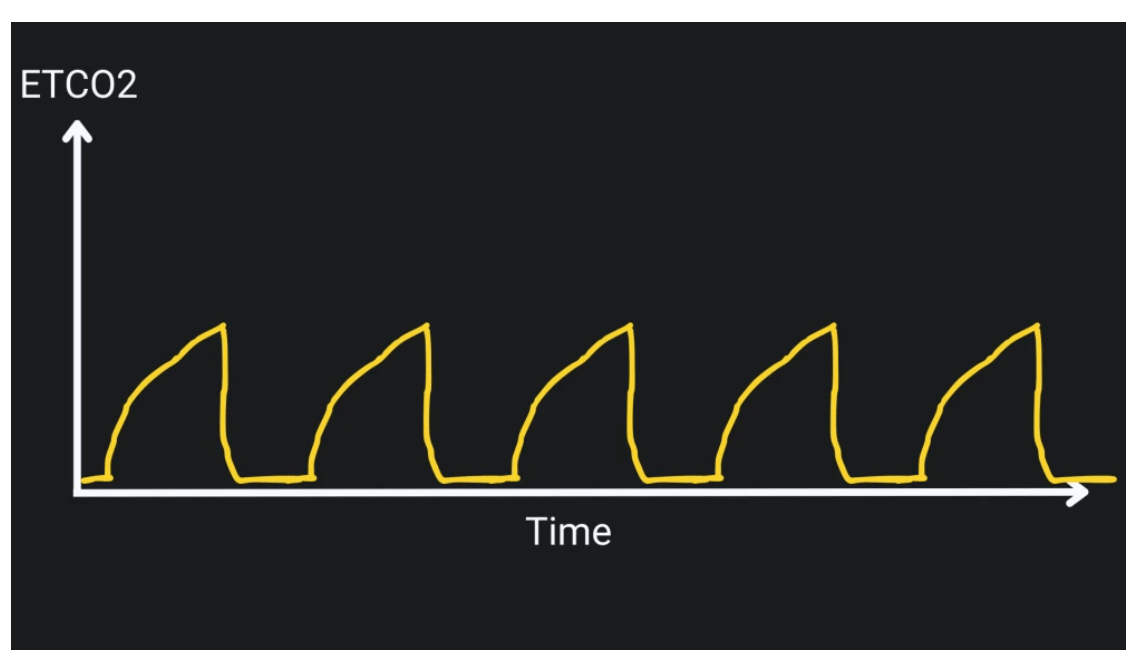
CPR is being performed on a patient and compressions are paused for pulse check. The following waveform is seen on the monitor. What does this waveform likely indicate?
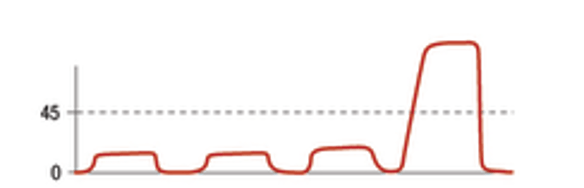
Answer: What is ROSC?
Explanation: This sudden jump in EtCO2 suggests ROSC.
- Return of circulation will often cause an abrupt jump in the etCO2.
- A rapid increase in etCO2 by >10 mm is highly suggestive of ROSC.
- Long B, Koyfman A, Vivirito MA. Capnography in the Emergency Department: A Review of Uses, Waveforms, and Limitations. J Emerg Med. 2017 Dec;53(6):829-842. doi: 10.1016/j.jemermed.2017.08.026. Epub 2017 Oct 7. PMID: 28993038.
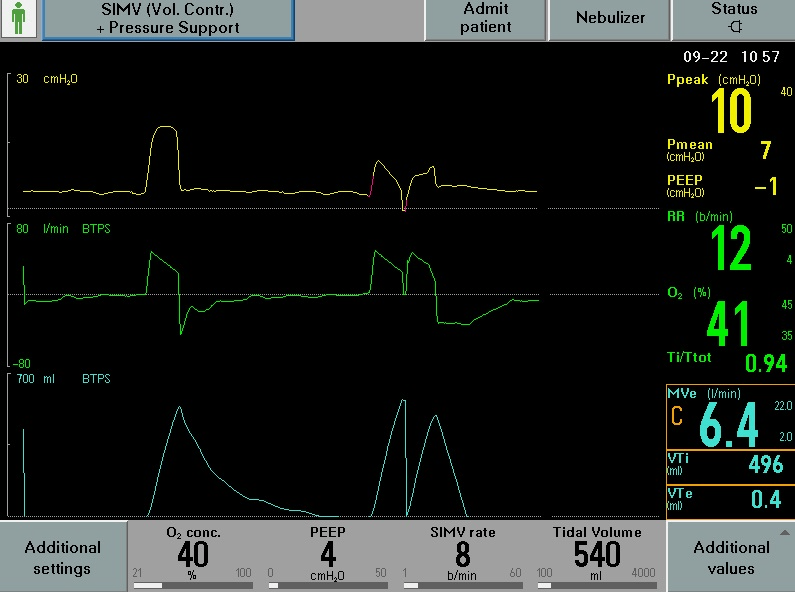
Identify the ventilator asynchrony shown in the image.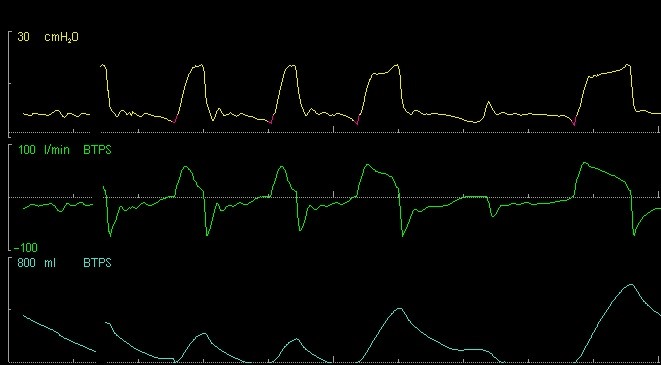
What is ineffective triggering?
In this asynchrony, the patient makes inspiratory effort, but the ventilator does not respond with a mechanical breath. Either the patient makes too weak an effort for the flow or pressure sensor/trigger or the sensor is not set at an adequate threshold. Multiple patient factors can result in ineffective triggers, such as excessive sedation and weakness/debility.
Describe the following sign in this ECHO.
What is McConnell's sign?

McConnell’s sign is defined as right ventricular free wall akinesis with sparing of the apex. Typically this looks as if the apex of the RV is a trampoline bouncing up and down while the rest of the RV remains still. This finding is not sensitive for acute PE, but is specific.
In ARDS from CAP, aside from standard of care for treating ARDS and infection, what additional therapy has shown mortality benefit?
What is Corticosteroids?
Recommended for severe CAP, especially in mechanically ventilated patients. Studies like CAPE COD show mortality reduction in critically ill CAP patients with steroids.
Common regimens include hydrocortisone 200 mg/day (CAPE COD) or dexamethasone 20 mg/day (DEXA-ARDS) for ARDS, followed by tapering.
Describe the waveform capnography pattern.
What is "rebreathing pattern"?
A rebreathing pattern in capnography is characterized by a rise in the baseline or phase I of the capnogram. This can be caused by low tidal volume, increased dead space, or inadequate fresh gas flow. This can be seen in faulty ventilator circuits or single-limb circuits without proper gas venting.
Out of these four conditions which one is the most likely cause of this wave form on capnography?
- COPD
- Pulmonary Fibrosis
- ETT obstruction
- Pneumothorax
Answer: What is COPD?
Explanation: Obstructive airway disease (e.g., asthma, COPD, or upper airway obstruction). The shape indicates slow exhalation due to airway narrowing or obstruction. The "shark fin" represents incomplete emptying of the lungs, often due to bronchoconstriction.
45 year old male with ARDS is on day three of mechanical ventilation. He is off paralytics and sedation is being weaned. Identify the following ventilator asynchrony.
(Hint: See red arrows)
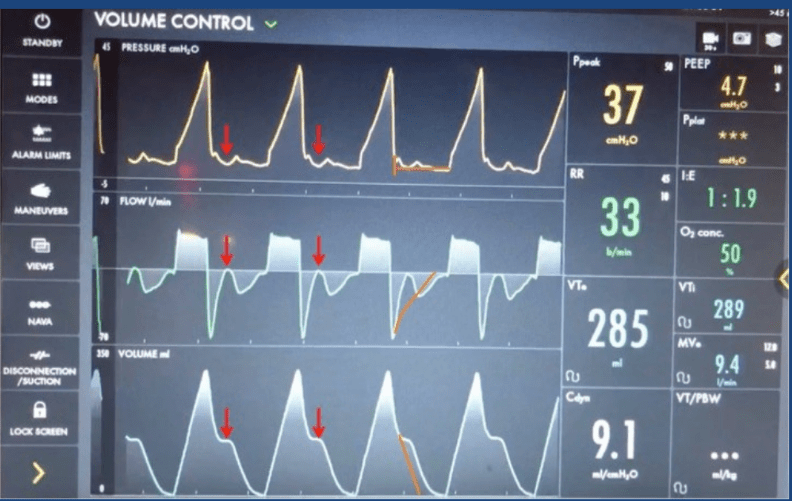
What is reverse triggering?
Reverse triggering is form of ventilator asynchrony where the ventilator-triggered breath inadvertently stimulates the patient’s spontaneous inspiratory effort, causing the patient to initiate a second breath during the ventilator’s inspiratory phase. This results in the patient’s breath occurring after the ventilator's inspiration has begun, creating a "reverse" pattern on the ventilator waveform. It can also occur in patients with neuromuscular weakness or excessive sedation that leads to paradoxical breathing patterns.
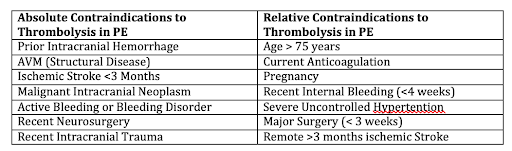
How long after a non-hemorrhagic stroke is tPA an absolute contraindication?
What is non-hemorrhagic stroke within the last 3 months?
The primary advantage of VV ECMO is to reduce what in ARDS?
What is Ventilator-associated Lung injury?
Both EOLIA and LIFEGARDS trials demonstrated that VV ECMO enabled significant reductions in key ventilator parameters:
- Tidal Volume (VT): Reduced to around 3.7 mL/kg ideal body weight (IBW) from control values of ~6.1-6.4 mL/kg IBW.
- Plateau Pressure (PPLAT): Lowered to 24 cm H₂O from control values of 28-32 cm H₂O.
- Driving Pressure (DP): Decreased to 13-14 cm H₂O from control values of 16-20 cm H₂O.
Describe the effect proning has on the heart in ARDS patients?
"What is improved RV function?"
Prone ventilation in severe ARDS can improve RV function by normalizing septal position, enhancing cardiac output and hemodynamics in addition to providing respiratory benefits.
Benefits of prone ventilation:
- Improves oxygenation, increases lung compliance, promotes homogeneous ventilation distribution, reduces ventilator-induced lung injury (VILI), and unloads the right ventricle (RV).
- RV Dysfunction in ARDS: Seen in ~25% of severe ARDS cases, often with septal deviation toward the left ventricle (LV), increased RV-to-LV end-diastolic area ratio, and tricuspid regurgitation.
- Prone ventilation can reduce RV size relative to the LV and normalize the position of the interventricular septum, shifting it back toward the RV, which may enhance RV function, stabilize cardiac output, and improve hemodynamics.
- Prone positioning generally increases lung compliance while decreasing chest wall compliance. The net effect is often stable or modestly increased overall respiratory system compliance, rather than a decrease.
- Prone ventilation typically raises the P/F ratio, often significantly, though the survival benefit is attributed to factors beyond improved oxygenation alone.
A 35-year-old male with alcohol withdrawal is intubated for airway protection. The patient is intubated and the following waveform appears on the monitor. What does this indicate?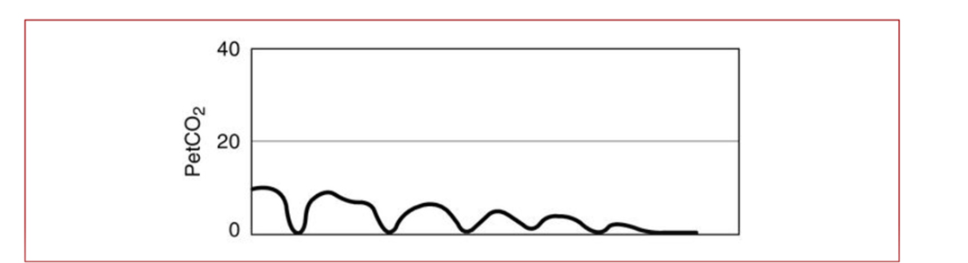
What is esophageal intubation?
This indicates that the endotracheal tube is in the esophagus rather than the trachea, leading to little or no CO2 being detected in exhaled air. It may also be seen in patients with poor lung perfusion.
You are called for an Increased respiratory rate. What is the diagnosis? 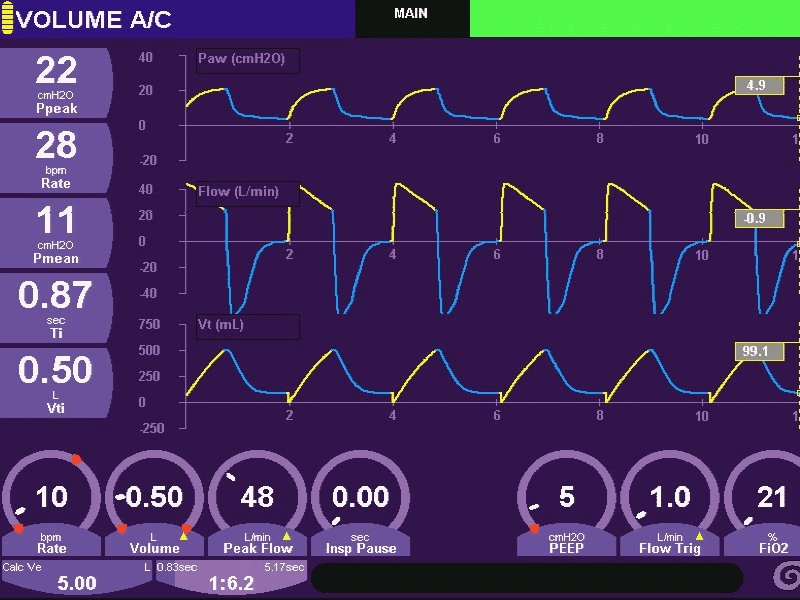
What is "air leak"?
On a ventilator waveform, an air leak is typically identified by an expiratory curve that does not fully return to baseline on a volume-time graph, indicating that some air is escaping from the system during exhalation, causing a "plateau" effect, and can also be seen as an incomplete loop on a pressure-volume (PV) or flow-volume (FV) loop, where the curve doesn't fully close at the end of the breath cycle; essentially showing a loss of volume that isn't fully exhaled due to the leak.
Possible causes of air leak could be ETT (Endotracheal tube) cuff leak, ventilator circuit traps which are loose, or ETT, which is of smaller size than the glottis. These abnormalities can be easily identified and can be corrected.
What RV:LV ratio is indicative of severe pulmonary embolism (PE) and is associated with increased mortality.
What is RV:LV Ratio >1?
An RV/LV ratio greater than 1.0 generally signifies right ventricular dilation which can occur in PE. Studies have shown that a higher RV/LV ratio on imaging is associated with a significantly increased risk of complications and mortality in patients with pulmonary embolism.
What trial showed referral to ECMO centers improved survival without severe disability over conventional care?
What is the CESAR trial?
The CESAR trial found that referral to extracorporeal membrane oxygenation (ECMO) for severe respiratory failure resulted in a higher survival rate without disability at six months compared to conventional management:
- Survival: 63% of patients in the ECMO group survived to six months without disability, compared with 47% of patients in the conventional management group.
- Quality-adjusted life-years: ECMO treatment resulted in a gain of 0.03 quality-adjusted life-years (QALYs) at six months.
- Cost: A lifetime model predicted that the cost per QALY of ECMO was £19,252.
The CESAR trial was designed to use current ECMO protocols and compare the benefit of ECMO to conventional therapy in patients with severe respiratory failure. The trial was conducted at multiple centers, including Glenfield Hospital in Leicester, UK, which had 17 years of experience with ECMO.
What does this wave-form capnography indicate about the respiratory lung physiology of a patient with pulmonary fibrosis?
What is Poor lung compliance?
The "pigtail" capnogram pattern typically appears in cases of poor lung compliance. It represents a sudden peak in pre-inspiratory expired CO2, which is caused by abrupt airway closure. This happens when a poorly compliant lung compresses the final milliliters of CO2-rich gas from the alveoli. Once the lung parenchyma collapses, it occludes the small bronchi, stopping the escape of gas.
Give the name and the diagnosis of the following capnography. 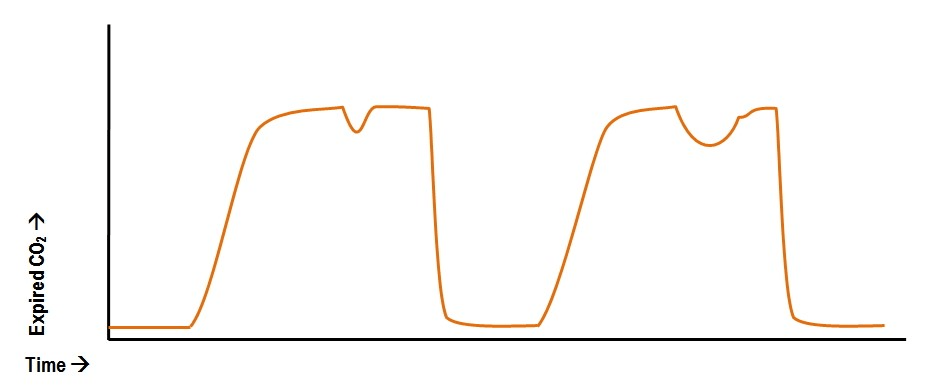
Answer: What is "curare" cleft?
Explanation:
This seen in the alveolar plateau is actually a patient making an attempt to breathe. With weak inspiratory effort, some fresh gas sucked from the ventilator tubing and past the capnometer, generates this pattern. It is most frequently seen in anesthetic machines where there is a constant flow of fresh gas across the circuit.
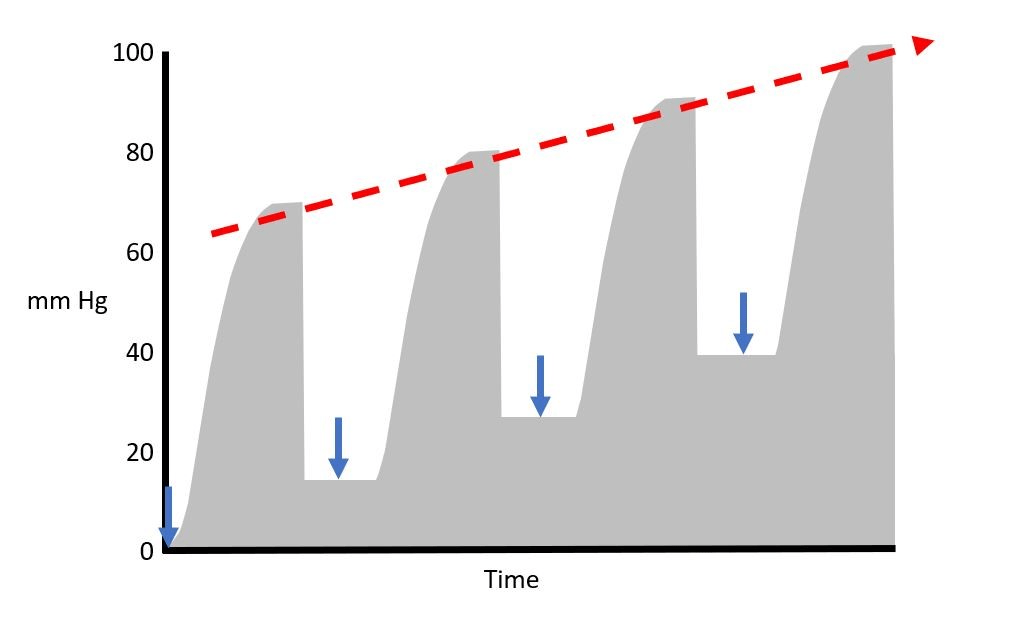
Because of concerns about ventilator asynchrony, you are called to the bedside of a patient receiving assist-control mechanical ventilation. The patient already has an esophageal balloon catheter in place to guide ventilator management, and you inflate the balloon during an episode of breath stacking. The figure displays the esophageal manometer waveform.
This esophageal waveform is most consistent with what form of ventilator asynchrony?
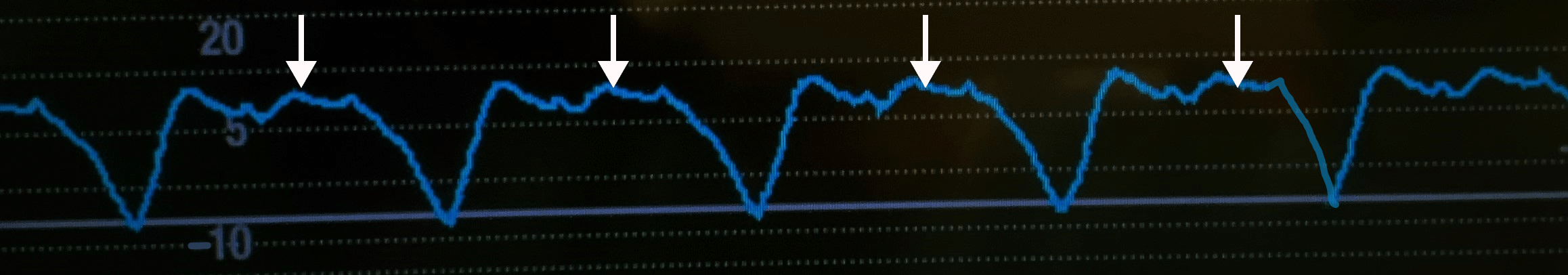
What is reverse triggering?
The esophageal waveform shown in the figure is most consistent with reverse triggering, which is also known as entrainment.
In this ventilator asynchrony, contraction of the diaphragm is triggered by the delivery of a ventilator-initiated breath. This leads to a patient-initiated breath at the end of the inspiratory phase of the ventilator-initiated breath, causing breath stacking. This asynchrony is increasingly recognized in patients receiving mechanical ventilation. In the figure, each white arrow demonstrates a ventilator-initiated breath that is followed, after a short time, by a large negative deflection in esophageal pressure. This negative deflection in esophageal pressure represents the generation of negative pleural pressure by a reverse-triggered patient-initiated breath. Reverse-triggered breaths can be difficult to identify, given that most patients do not have esophageal pressure monitoring. Other characteristic features of reverse triggering include breath-stacking events that universally begin with a ventilator-initiated breath and a regular 1:1 or 1:2 ratio of asynchronous to synchronous breaths, a phenomenon known as phase locking. Episodes of reverse triggering can be brief and interspersed between other patterns of ventilation. The causes of reverse triggering are not completely understood, but this phenomenon has been associated with deeper levels of sedation. On the basis of this observation, lightening of sedation has been suggested for patients with evidence of reverse triggering, though the clinical effect of this approach remains unclear.
Why is lower-dose alteplase preferred for catheter-directed thrombolysis (CDT) in pulmonary embolism (PE) compared to full-dose regimens used in myocardial infarction or ischemic stroke?
What is 100% of the dose is delivered to the RA?
What is complete resolution of clot is not necessary for hemodynamic improvement?
Lower doses of alteplase are preferred in PE because 100% of the infused dose reaches the pulmonary arteries, unlike in myocardial infarction, where only about 5% goes to the coronary arteries. In PE, occlusion is entirely due to clot formation, which contrasts with myocardial infarction, where there may be partial occlusion from plaque. The efficacy of thrombolysis is higher when the occlusion is mainly from clot, meaning a lower dose of alteplase may be effective. Where complete clot resolution is not required for a clinical benefit, and lower doses (e.g., 8-25 mg) are effective in improving pulmonary hemodynamics without significantly increasing the risk of hemorrhage.
What trial showed early prolonged prone positioning reduced 28-day and 90 day mortality in severe ARDS?
What is the PROSEVA trial?
The PROSEVA trial randomized 466 patients to either prone or supine positioning. Most patients had ARDS due to pneumonia, and most received vasopressors, neuromuscular blockers, and sometimes glucocorticoids. On average, prone patients spent 17 hours prone per day, for a total of 73% of the time they were on a ventilator.
The PROSEVA trial found that prone positioning significantly reduced mortality and the need for ventilation in patients with severe acute respiratory distress syndrome (ARDS):
- The 28-day mortality rate was 16% in the prone group and 32.8% in the supine group. The 90-day mortality rate was 23.6% in the prone group and 41% in the supine group.
- Proned patients were extubated more often and spent fewer days on a ventilator.
- The incidence of complications was similar between the groups, except for cardiac arrests, which were more common in the supine group.
Among critically ill patients undergoing tracheal intubation, the most common major adverse events during the peri-intubation period is?
What is Hemodynamic instability?
In an observational study of intubation practices in critically ill patients from a convenience sample of 197 sites across 29 countries, the most common major adverse peri-intubation event was hemodynamic instability.