90% Type I
10% type II
Segond fracture, pathognomonic for an ACL tear, represents the bony avulsion of this ligament

Anterolateral ligament (ALL)
Which of the following physical exam maneuvers would be MOST expected for a patient with the following radiograph?

1. Positive Lachman's test
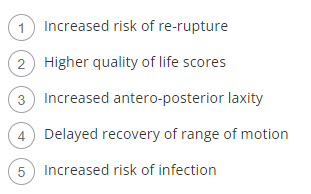
Which of the following is more likely to occur with use of a bone patellar bone allograft instead of a bone patellar bone autograft for anterior cruciate ligament (ACL) reconstruction in an 18-year-old high school or collegiate athlete?
3. ACL graft re-rupture
odds of graft re-rupture are 4.3 x higher in allograft for athletes aged 10-19
Compared with male athletes in the same sport, female athletes sustain anterior cruciate ligament (ACL) injuries:
- A: less frequently but are at increased risk for re-tear after return to sport.
- B: more frequently but are at reduced risk for re-tear after return to sport.
- C: more frequently and are at increased risk for re-tear after return to sport.
- D: less frequently and are at reduced risk for re-tear after return to sport.
- C: more frequently and are at increased risk for re-tear after return to sport.
The primary blood supply to the ACL
Middle geniculate artery
Which of the following bone bruise patterns seen on magnetic resonance imaging (MRI) is most consistent with an anterior cruciate ligament (ACL) tear?
A. Medial tibial spine and medial femoral condyle
B. Medial facet of patella and lateral femoral condyle
C. Posterolateral tibia and lateral femoral condyle
D. Posterolateral tibia and medial femoral condyle
E. Medial tibial spine and lateral femoral condyle
C. Posterolateral tibia and lateral femoral condyle
A high school athlete sustained a noncontact injury to his right knee. He says that during a football game he felt a pop and his leg gave way. On examination, As his knee is moved from full extension into flexion with an internal rotation and valgus force, you notice a "clunk" within the knee. What is the most likely biomechanical basis for the "clunk"?
4. In extension, the lateral tibial plateau is subluxated; as an internal rotation/valgus force is applied in conjunction with flexion, the lateral plateau reduces.
What is the effect on knee kinematics following placement of an anterior cruciate ligament (ACL) graft at the 12 o’clock position?
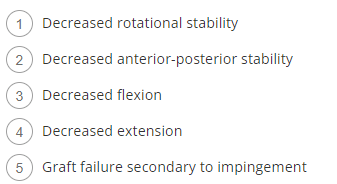
1. Decreased rotational stability
vertical femoral tunnel placement
cause by starting femoral tunnel at the vertical position in the notch (12 o'clock) as opposed to lateral wall (10 o'clock)
will cause continued rotational instability which can be identified on physical exam by a positive pivot shift
The anteromedial bundle footprints are represented by which two letters?
B&D
Name the anterior and posterior meniscofemoral ligaments that originate from the posterior horn of the lateral meniscus and insert into the PCL substance
Ligament of Humphrey (Anterior)
Ligament of Wrisberg (Posterior)
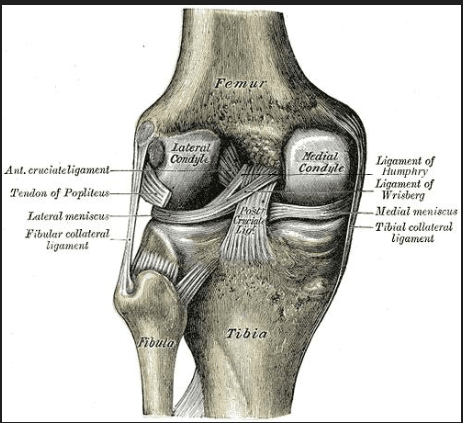
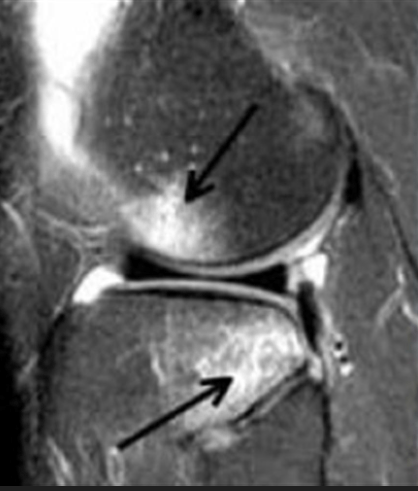
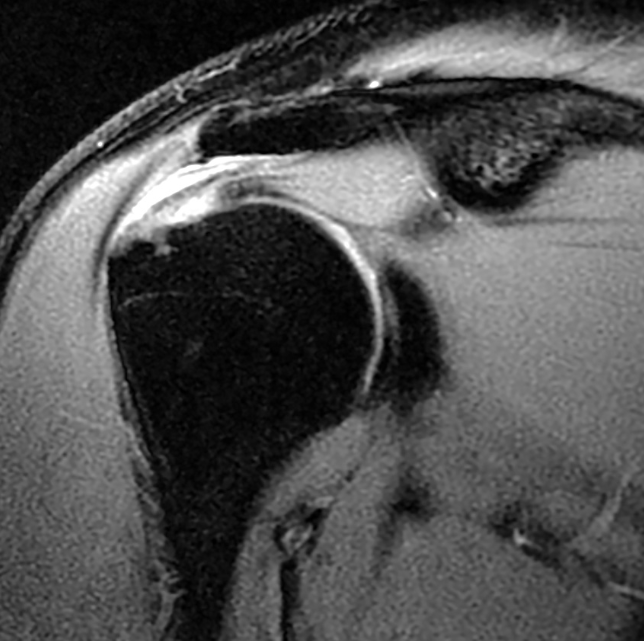
Figure below is a sagittal MRI cut of a 23-year-old male who injured his knee while playing soccer two days ago. Which of the following structures is most likely also affected in this acute injury?
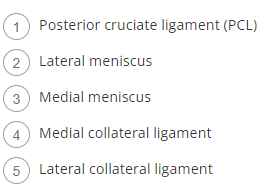
2. Lateral meniscus (54%)
Following ACL reconstruction, which of the following tests most closely correlates with patient satisfaction with their reconstructed knee?

4. Pivot shift test
A 27-year-old male presents to your clinic after injuring his knee playing recreational soccer several days ago. He reports a twisting injury with immediate swelling. On examination, you appreciate a grade 3B Lachman test. Based on this, you order an MRI which confirms your suspicion for a complete anterior cruciate ligament (ACL) rupture. If an ACL reconstruction is performed, which of the following factors most increases his risk for re-rupture?
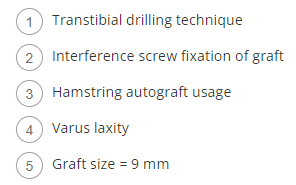
4. Varus Laxity
Concomitant posterolateral corner (PLC) injury which goes unrecognized at the time of anterior cruciate ligament (ACL) reconstruction places the graft at high risk for failure.
A 56-year-old man falls on an outstretched arm while skiing and sustains an anterior glenohumeral dislocation. Sixteen days after reduction in the emergency department, he is unable to abduct his shoulder. What is the most common reason for this finding?
1. Axillary nerve palsy
2. Cervical radiculopathy
3. Persistent glenohumeral dislocation
4. Supraspinatus tear
4. Supraspinatus tear
The rotator cuff plays important active and passive roles in glenohumeral stability. Rotator cuff injury can be common in patients over the age of 40 years in conjunction with glenohumeral dislocation, and persistent dysfunction after 2 to 3 weeks should prompt examination for such injuries. Although axillary injury and persistent glenohumeral dislocation can be complications associated with glenohumeral dislocation, they are less common than rotator cuff tears. Persistent pain after 2 weeks is uncommon and indicates concomitant injury. Rotator cuff injury is the most common injury seen; cervical radiculopathy is a less common injury.
Correctly identify structures labeled A and B in this image taken with the knee in 90 degrees flexion following debridement of native femoral attachment site of the ACL.
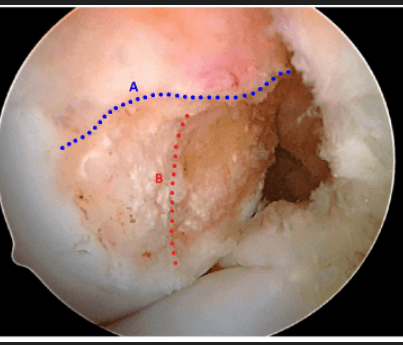
A = Lateral intercondylar ridge (residents)
B = Bifurcate ridge
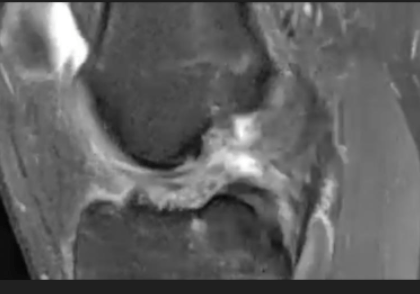
What is the most likely diagnosis?

A "Double PCL sign" is indicative of a bucket-handle medial meniscus tear
A 25-year-old male professional football player presents with severe right knee pain after he was tackled head-on at knee level by an opposing player. On physical examination, there is a large effusion of the right knee. Figure A is the clinical photograph with the patient laying on the exam table. Dial testing demonstrates 20° of increased external rotation of the right foot in 30° and 90° of knee flexion. What structures are most likely injured in this patient?

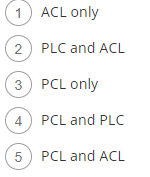
4. PCL and PLC
A 45-year-old man is involved in a motor vehicle collision where he rear ends a stopping vehicle ahead of him. He presents with knee pain and difficulty with weight bearing and climbing stairs. Radiographs and MRI are obtained and depicted in Figure A and B, respectively. During the maneuver depicted in Figure C, there is 2 degrees of asymmetry at 30 and 90 degrees. Which of the following is the best next step in management?

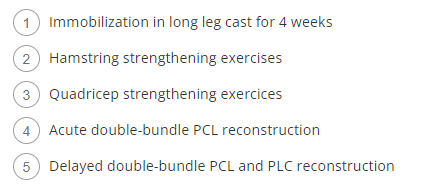
3. Quad strengthening exercises
This patient has sustained an isolated posterior cruciate ligament (PCL) injury, without a posterolateral corner (PLC) injury, as exhibited by the negative Dial's test on examination. Initial treatment for PCL injuries is non-operative, with a focus on quadriceps strengthening.
Figures 1 though 3 display the MRI scans from a 65-year-old man who is right-hand dominant. He reports 8 weeks of right shoulder pain. He localizes the pain to the anterior and lateral shoulder, and the pain is worse with overhead activities, reaching behind the back, and sleeping. He cannot recall any fall or other mechanism of injury. He is an avid tennis player and has not been able to play since the pain began. He would like to return to tennis as soon as possible. On physical examination, his rotator cuff strength is normal; he is tender over the bicipital groove; and he has positive Neer, Hawkins, Jobe, and Yergason tests. What is the best next step?
1. PT, NSAIDs, possible corticosteroid injection
2. Shoulder arthroscopy, rotator cuff debridement, biceps tenodesis
3. Obtain CT to visualize humeral head contour
4. Open rotator cuff repair
1. PT, NSAIDs, Injection
This patient has a partial articular side supraspinatus tear. He has not had any nonsurgical treatment, so it would be most appropriate to start with physical therapy and NSAIDs and discuss the risks and benefits of a corticosteroid injection. If nonsurgical treatment fails, then a shoulder arthroscopy to address the rotator cuff tear and any biceps pathology could be considered. An acute, full-thickness rotator cuff tear would be an indication for urgent surgery.
Anteromedial bundle of the ACL is tightest in ____ and primarily responsible for _______
Posterolateral bundle of the ACL is tightest in _____ and primarily responsible for ________
Anteromedial bundle is tightest in flexion and primarily responsible for restraining anterior tibial translation
Posterolateral bundle is tightest in extension and primarily responsible for rotational stability
The findings from the MRI depicted in Figure A have been shown to predict which of the following outcomes after anterior cruciate ligament (ACL) reconstruction?

4. Delayed recovery of ROM
A soccer player sustains a knee injury. He is noted to have a significant increase in tibial passive external rotation both at 30 and 90 degrees. Which of the following structures is least likely to be injured?
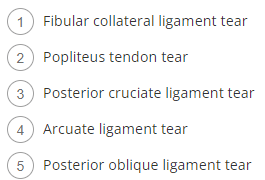
5. Posterior oblique ligament tear
The posterior oblique ligament is a structure on the medial aspect of the knee.
The fibular collateral ligament (also known as lateral collateral), Arcuate ligament, and popliteus tendon are all components of the postero-lateral corner (PLC). A positive dial test at 30 degrees indicates an isolated PLC injury, while a positive dial test at 30 and 90 degrees indicates PLC and concurrent posterior cruciate ligament (PCL) injury.
A 21-year-old male collegiate basketball player presents with left knee pain and swelling after landing awkwardly from a rebound. The patient previously underwent an ACL reconstruction of the left knee at 16 years of age with ipsilateral bone-patellar tendon-bone autograft. On physical examination, the patient has a large effusion with a range of motion limited from 10° to 80° of knee flexion. Lachman's and pivot shift are both positive. Radiographs are unremarkable for any fractures but demonstrate 10° of mechanical axis varus, an 87° mechanical lateral distal femoral angle, and 15° of posterior tibial slope. CT scan confirms appropriate tunnel position, with the largest diameter measuring 10mm. He wants to continue playing at the same level. Which of the following would be the most appropriate treatment option?
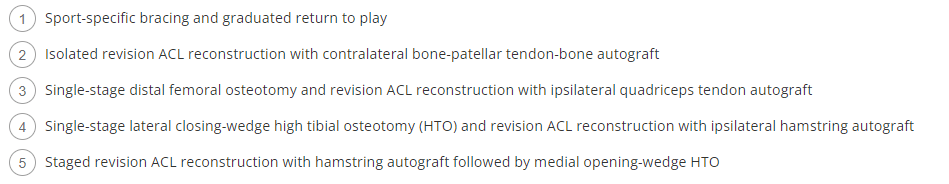
4. Single-stage lateral closing-wedge HTO and revision ACL with hamstring autograft
The patient sustained a recurrent ACL rupture in the setting of varus malalignment of the tibia and an increased posterior tibial slope. The ideal treatment for this patient would include simultaneous correction of the tibial varus and neutralization of the tibial slope through a lateral closing wedge osteotomy combined with a revision ACL reconstruction. The ACL reconstruction can be performed in the same surgical setting of the high tibial osteotomy or staged following the high tibial osteotomy. While both medial opening-wedge and lateral closing-wedge high tibial osteotomy (HTO) can adequately address proximal tibial varus, a lateral closing-wedge osteotomy is more effective in simultaneously correcting the posterior tibial slope.
A 55-year-old man sustains a fall off of a two-step ladder and has pain and weakness in his right shoulder. His MRI scan shows medial subluxation of his biceps. What physical examination would confirm this finding?
1. Empty can test
2. External rotation lag sign
3. Abdominal compression test
4. Hornblower test
3. Abdominal compression test
Medial subluxation of the biceps tendon is indicative of a tear of the upper border of the subscapularis tendon. On physical examination, this would be identified by a positive belly press test. A positive empty can test implies injury to the supraspinatus, the external rotation lag sign indicates injury to the external rotators, and the Hornblower test is indicative of injury to the teres minor.