For maximum efficacy, the HPV vaccine should ideally be administered:
before sexual contact
1.What is the recommended age to start regular cervical cancer screening as per WHO guidelines?
30 years
What should be done for a 35 year old woman with CIN 2 who are not eligible for ablative treatment?
Excisional treatment
.In the context of colposcopy, what does a 'Type 3' transformation zone indicate?
The transformation zone extends into the endocervical canal and is not fully visible.
VIA is appropriate to use in women upto which age and why?
in women whose transformation zone is visible (typically in those younger than 50 years).
This is because once menopause occurs, the transformation zone, where most pre-cancer lesions occur, frequently recedes into the endocervical canal and prevents it from being fully visible
What is the primary focus of the WHO's HPV vaccination strategy?
preventing cervical cancer
In a 'screen-and-treat' approach, what follows a positive primary screening test for cervical cancer?
Immediate treatment
Which gene mutation is most closely associated with HPV-related carcinogenesis?
P53
what are the different types of cone biopsies
1. Cold knife cone
2. laser cone
3. LLETZ cone
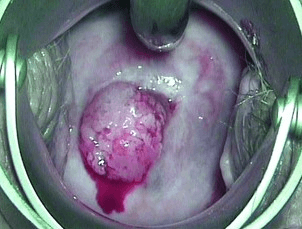
suspicious of cervical cancer so needs biopsy
Which HPV vaccine has the broadest coverage in terms of HPV types?
Gardasil 9
In PRIMARY HPV DNA SCREENING AND VIA TRIAGE (SCREEN, TRIAGE AND TREAT APPROACH) the HPV is positive and VIA is negative in a NON HIV positive patient
how should we manage such woman?
repeat HPV test in 2 years
What is the follow-up protocol for a patient with a negative result after immediate HPV triage following an ASCUS cytology finding?
Rescreen in 3 years with cytology
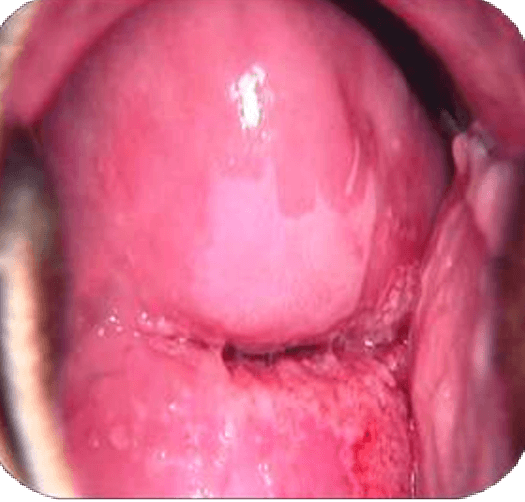
A 40 year old with PCB has come to your clinic. these are VIA results
VIA positive and suggestive of HGSIL
Knife cone biopsy is the preferred excisional method in preinvasive disease in which two conditions
when invasive cancer or glandular disease is suspected
At what age does the dosage schedule change from 2 doses to 3 doses for Gardasil?
15 years and above
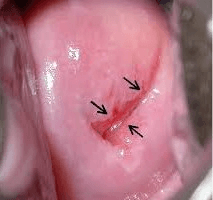
Besides screen and treat approach visual inspection with acetic acid is also used for
determining eligibility for ablative treatment
what are the eligibility criterias for ablative treatment for pre invasive lesions
1. The entire lesion is on the ectocervix.
2. The lesion does not cover more than three-quarters of the cervix.
3. All margins of the lesion are visible.
What is a key piece of information we as providers need to know about the colposcopy in order to determine treatment modalities?
whether colposcopy was adequate or inadequate
VIA negative
HPV testing is not recommended in women less than 30 years of age because
because of high rate of transient infections
What is the maximum room temperature stability duration for self-collected HPV DNA test specimens
30 days
If treated with ablation or LLETZ without histopathology results available, or if treated based on histopathology of CIN2/3 or AIS, when should the follow up testing be done
After 12 months
What is schiller's test
a preliminary test for cancer of the uterine cervix in which the cervix is painted with an aqueous solution of iodine and potassium iodide and which shows up healthy tissue by staining it brown and possibly cancerous tissue as white or yellow due to its failure to take up the stain because of a deficiency of glycogen in the cells
When should a VIA positive woman undergoing cryotherapy have repeat screening?
One year