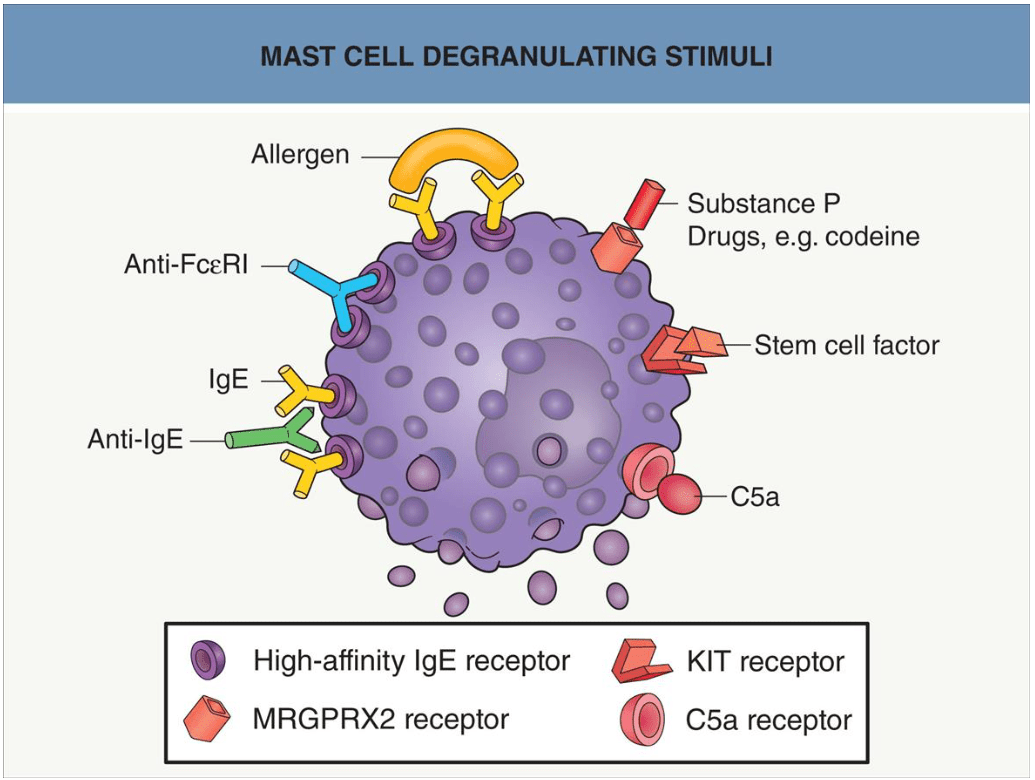
Name 3 signaling stimuli that can trigger mast cell degranulation
FcεRI based mechanisms:
- IgE crosslinked via allergen
- Anti-FcεRI Ab
- IgE crosslinked via Anti-IgE Ab
Other mechanisms:
- MRGPRX2 receptor
- KIT receptor
- C5a receptor
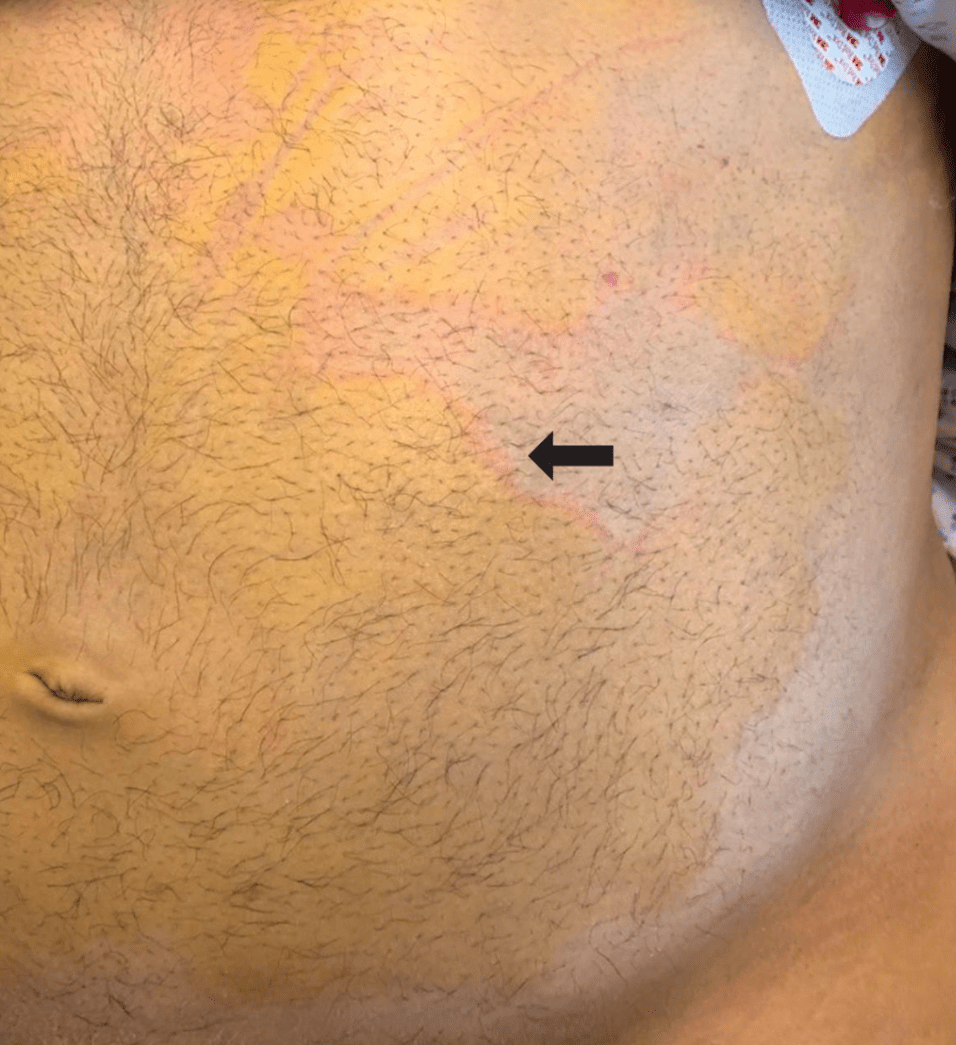
Name this koda
- Name 3 examples of locations where this could present (besides what's in the photo) and reasons why someone would get this at these locations

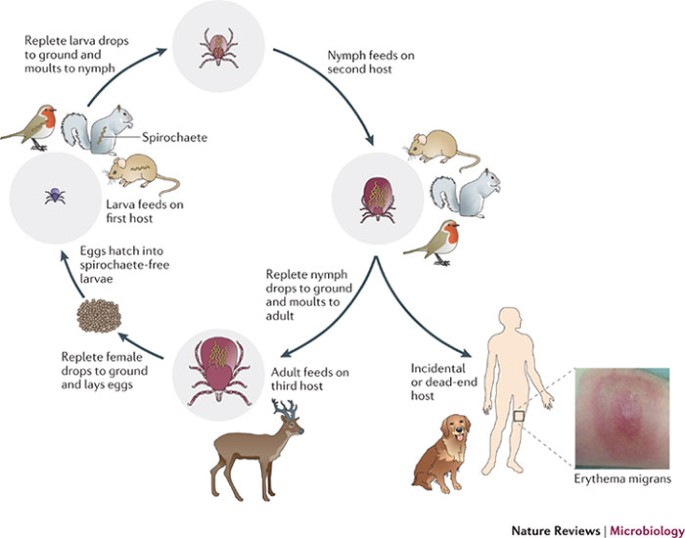
Delayed pressure urticaria
Development of deep erythematous swellings at sites of sustained pressure to the skin, after a delay of 30 minutes to 12 hours
Urticaria may persist for several days.
Examples:
- Waistline due to wearing tight clothes
- Ankles due to wearing socks
- Feet due to wearing right shoes
- Palms after manual labor
- Soles of feet after walking
- Genitals after sexual intercourse
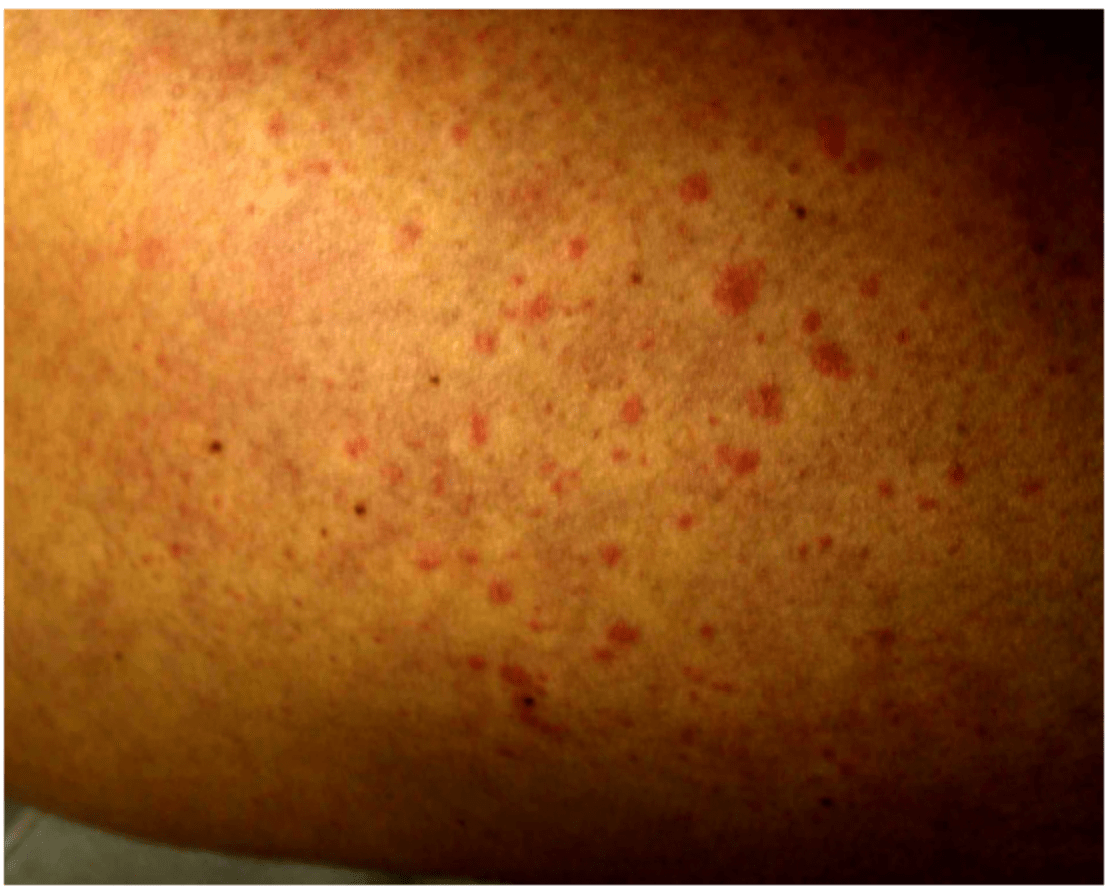
Young woman looks like this after eating some spicy food, name this koda
Bonus: Name 3 distinguishing features between this and heat urticaria
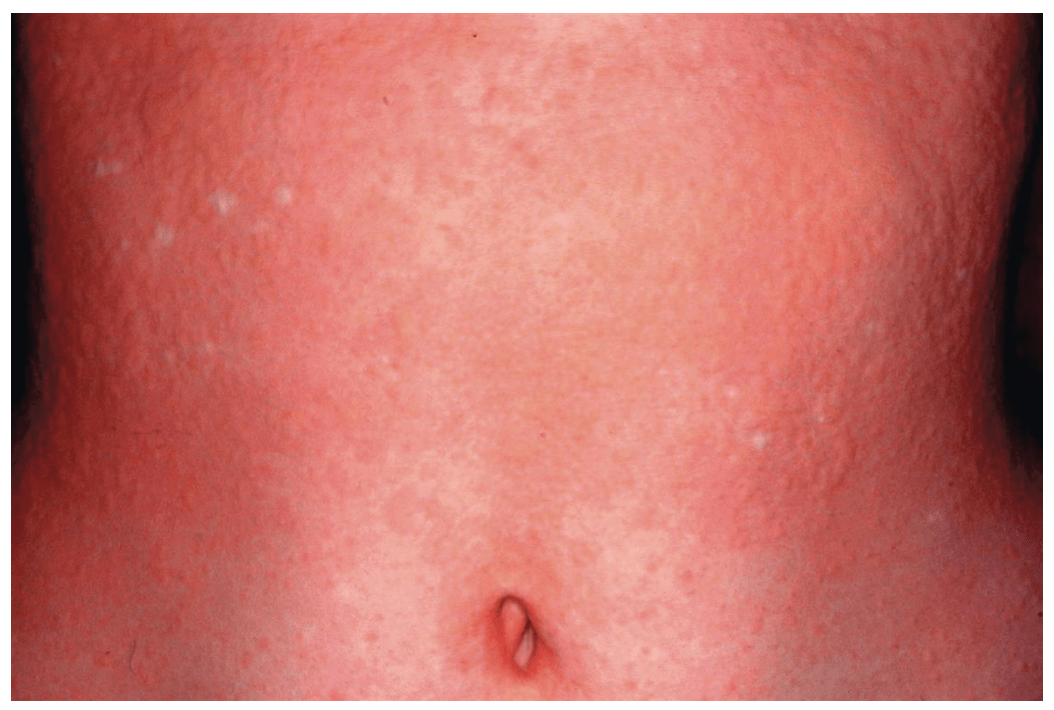
Cholinergic urticaria:
- Multiple, transient, papular wheals 2–3 mm in diameter surrounded by a flare
- Occur within 15 minutes of sweat inducing or body temperature increasing stimuli: Exercise, hot bath, stress, hot room, alcohol, spicy food
Differences between heat urticaria and cholinergic urticaria:
- Heat urticaria: Triggered by external heat, larger more classic wheals, more localized, positive response to local heat challenge test, direct mast cell activation by heat
- Cholinergic urticaria: Triggered by increase in core body temperature, smaller more pinpoint wheals, more generalized, positive response to exercise challenge or hot bath test, acetylcholine-mediated mast cell degranulation
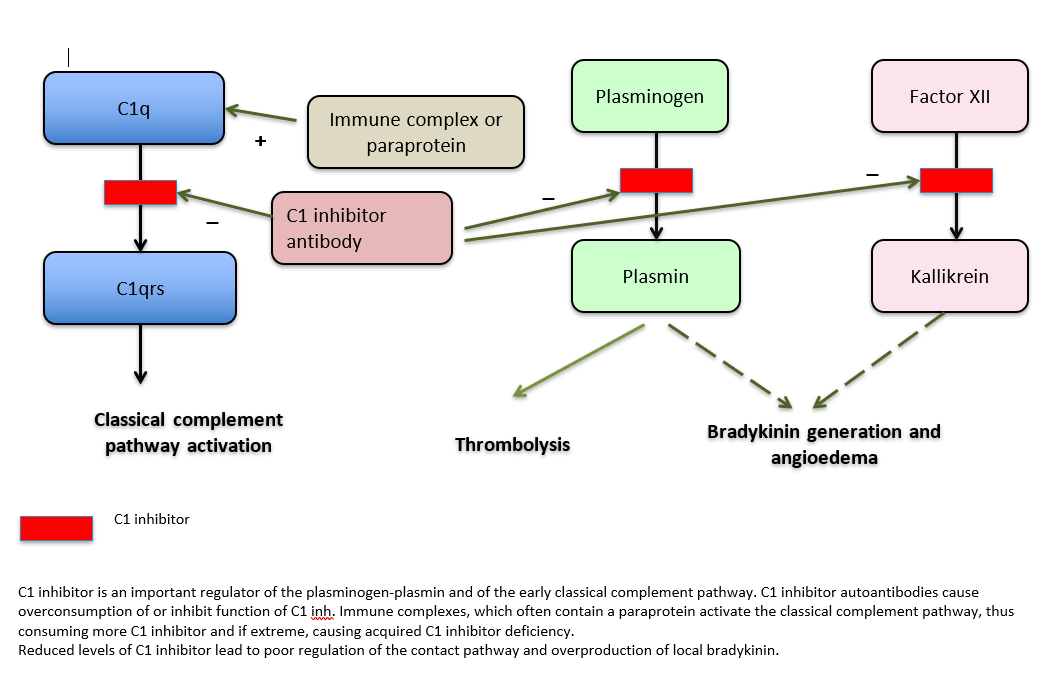
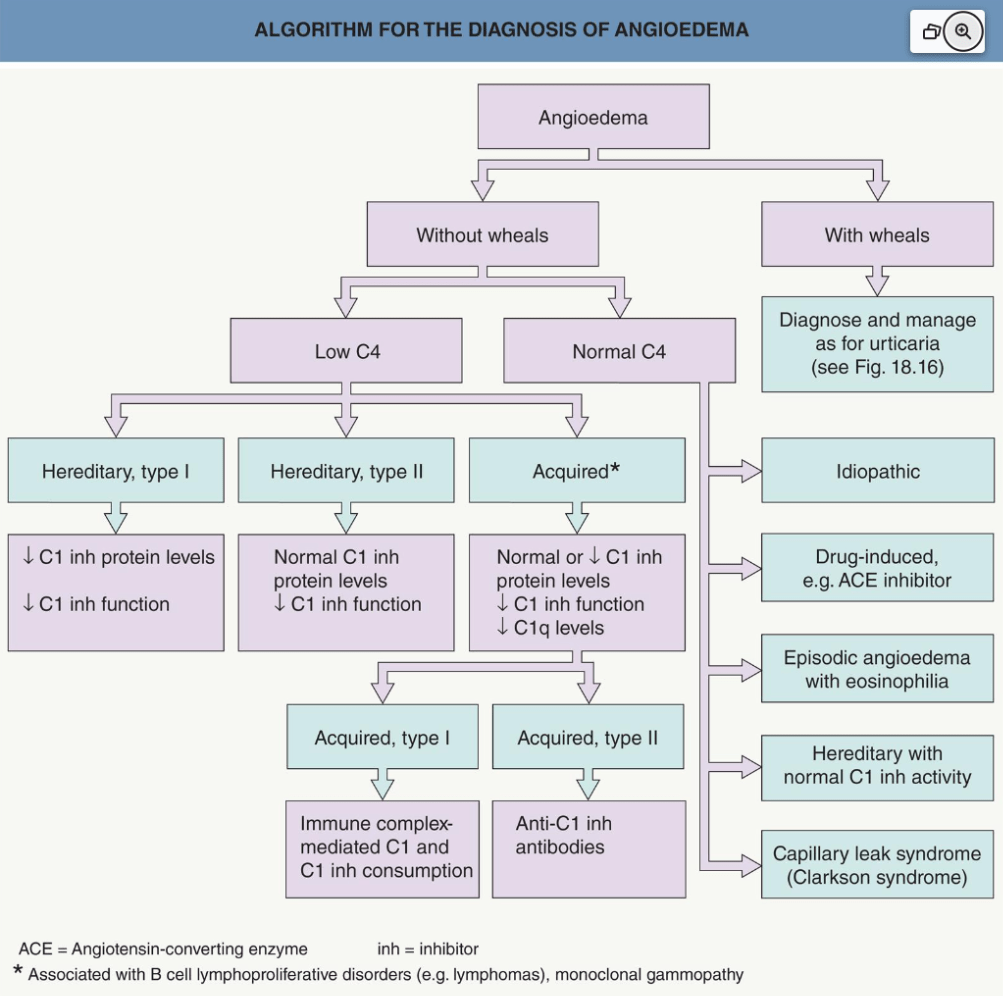
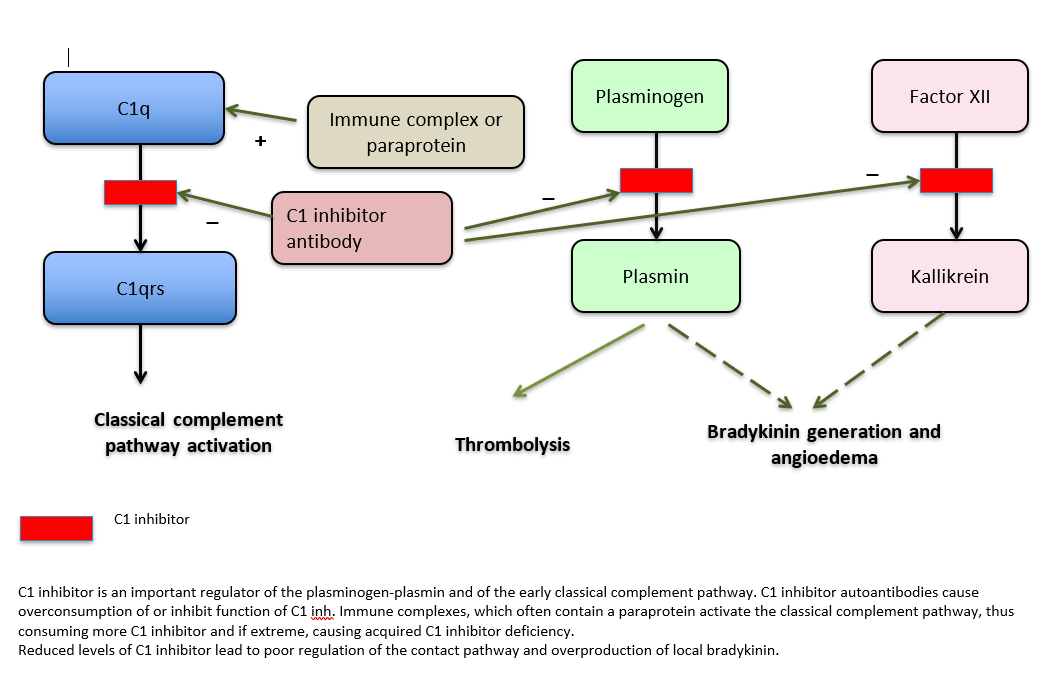
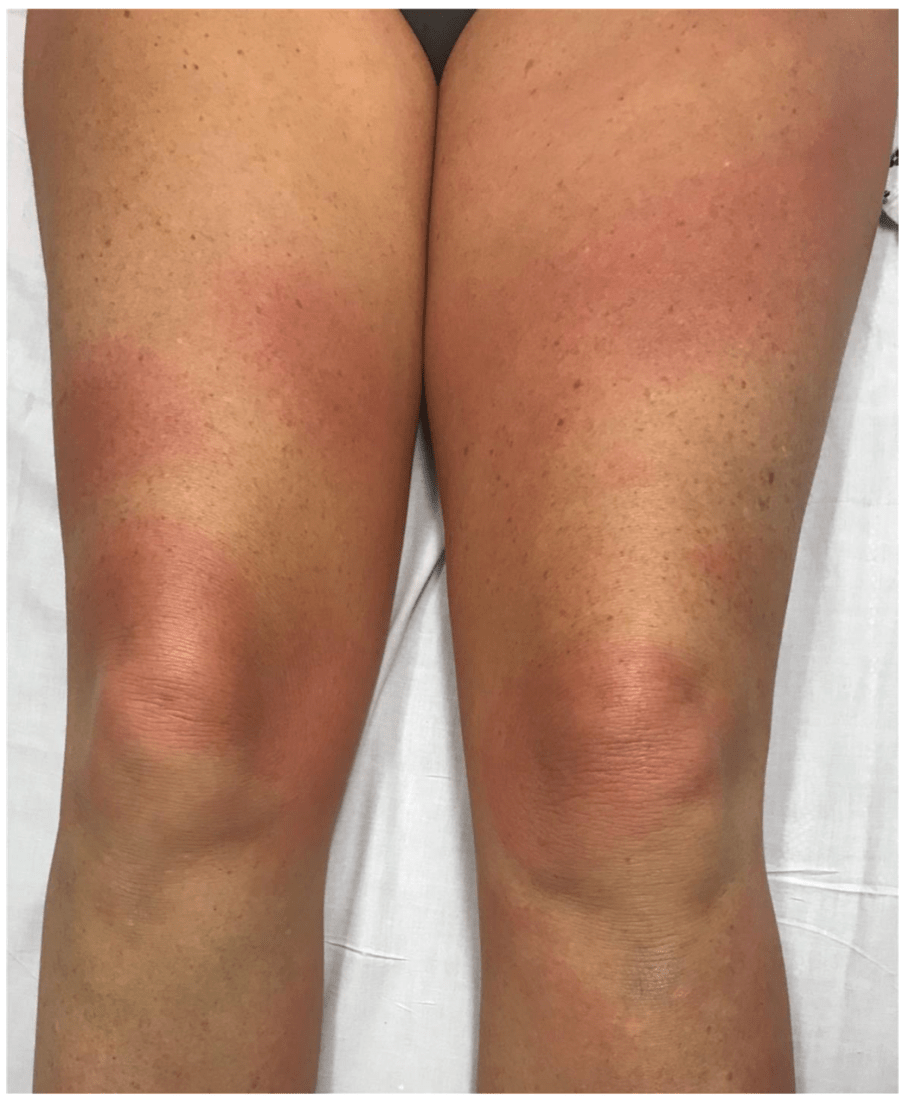
Mechanism of acquired angioedema (AAE) types 1 and 2
Bonus: Diseases that are associated with AAE types 1 and 2
Bonus: Factor that is typically decreased in AAE but NOT in HAE
AAE type 1: Consumption of C1 inh
AAE type 2: Inhibitory antibodies against C1 inh
Associated diseases: B-cell lymphoproliferative disorders, plasma cell dyscrasias, autoimmune connective tissue diseases
Will see decreased levels of C1q in about 70% of AAE cases due to excessive complement activation and consumption
See this with hypereosinophilia, weight gain, and fever
What syndrome is it?

Gleich syndrome:
- Episodic angioedema
- Urticaria
- Hyper-eosinophilia
- Fever
- Periodic weight gain
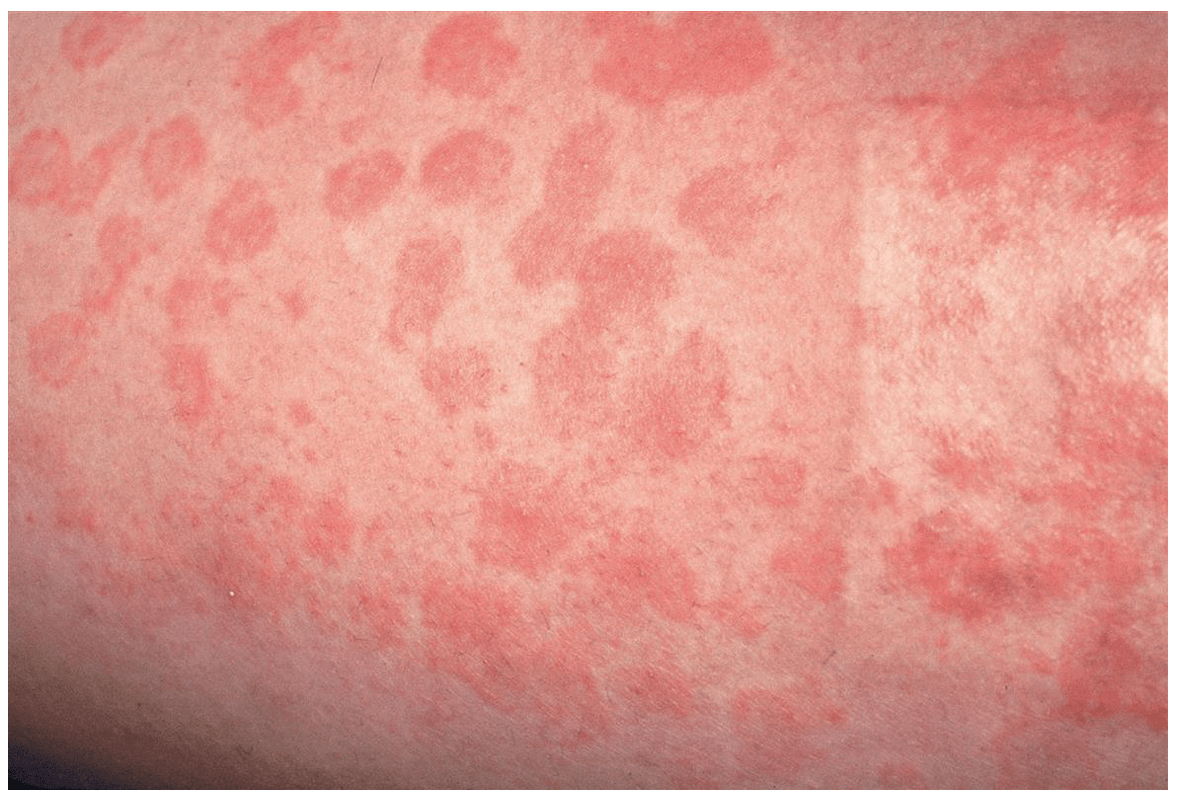
Name the figurate erythema in someone with acute rheumatic fever
Bonus: Name the JONES cardinal signs of rheumatic fever

Erythema marginatum
- Occurs 2-5 weeks after group A strep throat
- Erythematous macules that rapidly spread peripherally and become patches or plaques without scale (can be polycyclic)
- Most common on trunk, axillae, and proximal extremities (spares face)
-Remember JONES: Joints (arthritis), O (chamber like a heart, carditis), subcutaneous Nodules (over bony prominences in patients with longstanding disease), Erythema marginatum, Sydenham chorea
- On path: Interstitial and perivascular neutorphilic infiltrate w/o vasculitis
- EM usually seen with carditis
- Caused by abnormal humoral and cellular immune response to antigens associated with group A β-hemolytic streptococci
Name the lesion, and how long it should typically last
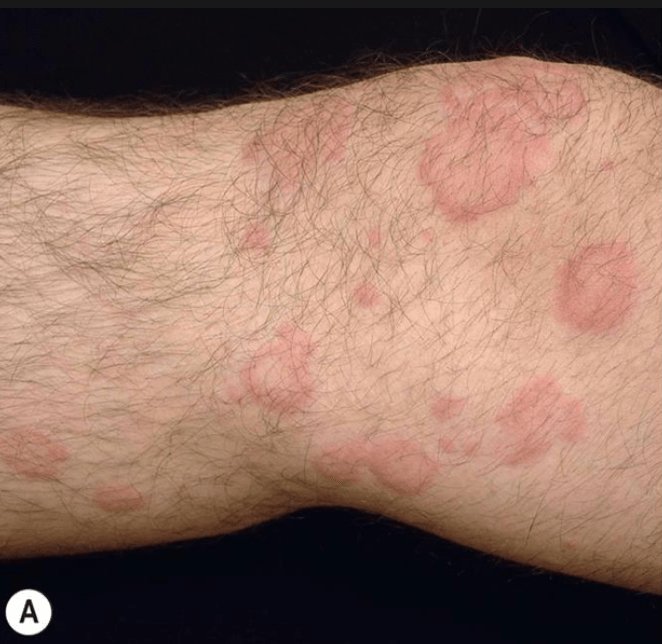
Wheals: Individual lesions should last < 24 hours

They can be annular and arcuate:


And even unusual colors like this patient with hyperbilirubinemia secondary to hepatic cirrhosis (note the elevated pink border):
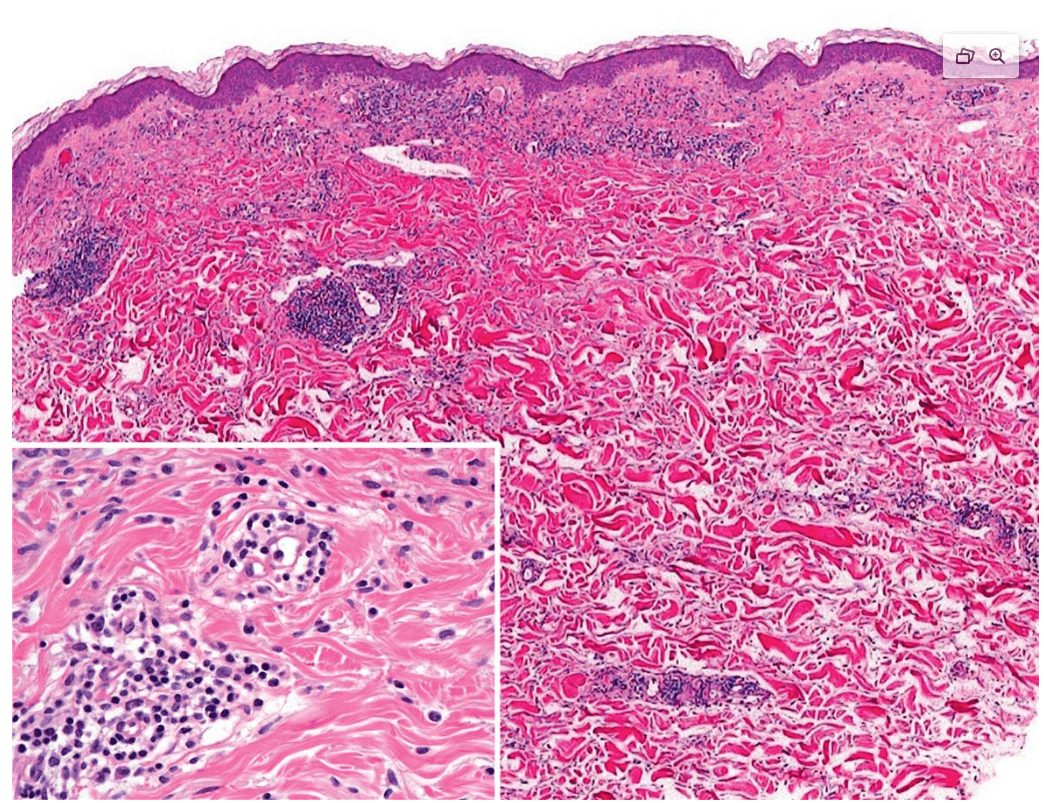
Histology findings of urticaria
Upper dermal edema w/ mild mixed perivascular infiltrate with lymphocytes, eosinophils, basophils, and neutrophils
Here we see a predominantly neutrophilic pattern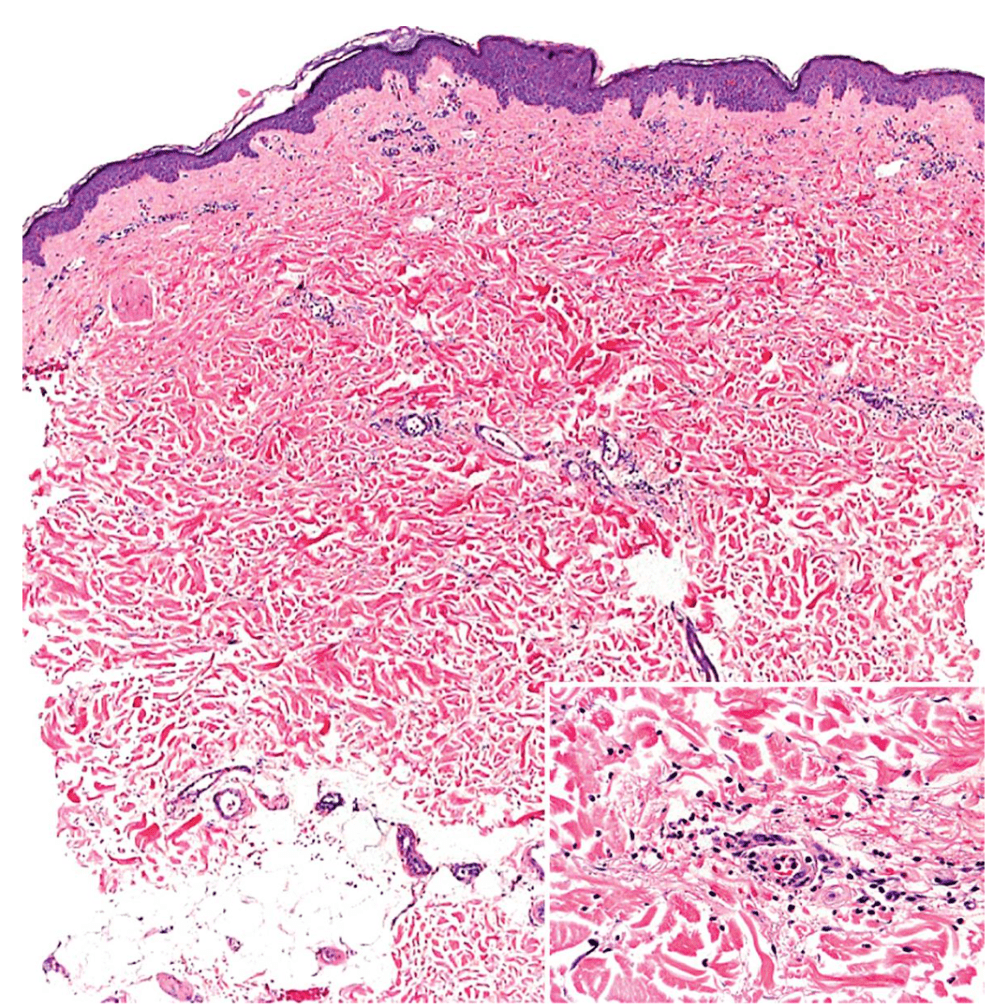
You put an ice cube on someone's arm, 10 minutes later you see this, name the class of urticaria and what subtypes of this class of urticaria do they likely NOT have
Likely don't have reflex cold and familial cold urticaria
- Primary cold contact urticaria: Generally idiopathic, most common in young adults, can have systemic symptoms (ie flushing, headache, syncope, and abdominal pain, if large enough area is affected)
- Secondary cold contact urticaria: Due to cryoglobulinemia, cryofibrinogenemia, hepatitis B/C, lymphoproliferative disease, or mononucleosis
- Reflex cold urticaria: Generalized cooling of the body induces widespread whealing
- Familial cold urticaria: Inherited inflammatory disorder following generalized exposure to cold, favors extremities, associated with fevers, arthralgias, and conjunctivitis
What tests should you obtain to figure out the etiology of angioedema?
C4
C1 inh
C1 inh activity
C1q
Anti - C1 inh Ab
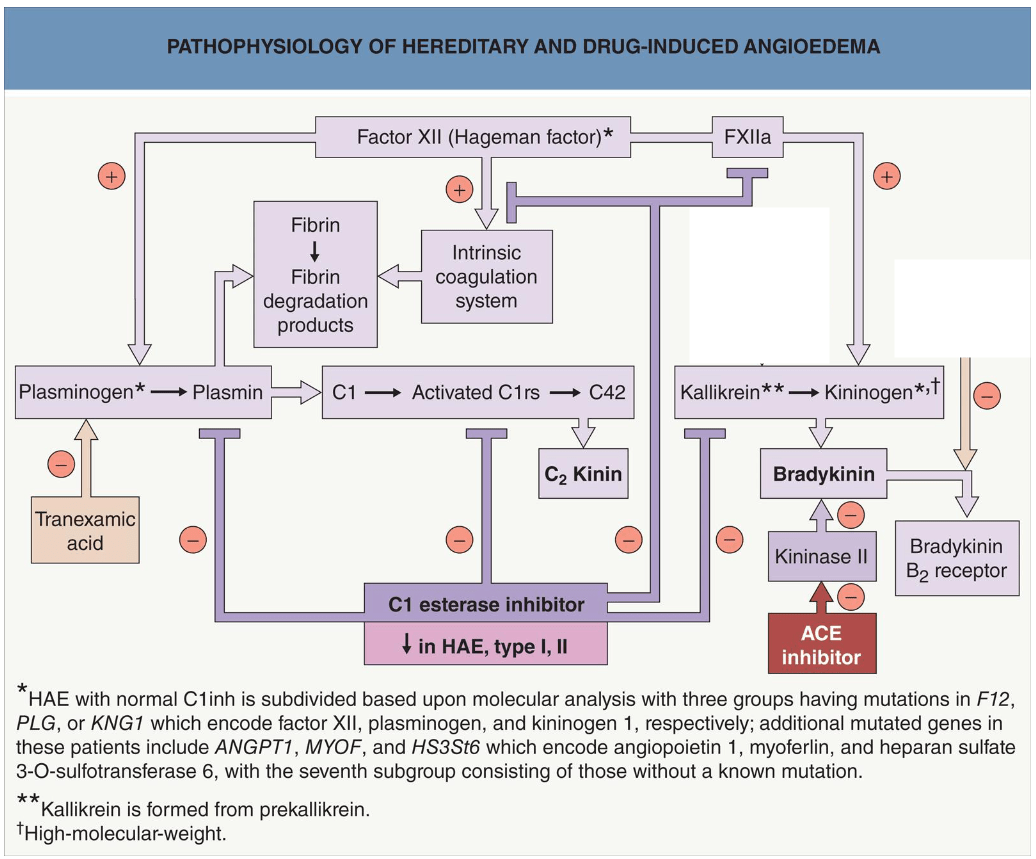
Treatment of acute life threatening flare of C1 inh deficiency
Long term prophylaxis of C1 inh deficiency
Treatment of acute life threatening flare of C1 inh:
- IV C1 inh concentrate or recombinant C1 inh (or FFP if neither is available)
- Ecallantide subq (kallikrein inhibitor)
- Icatibant subq (bradykinin B2 receptor antagonist)
- WHAT DOESN'T WORK: antihistamines, steroids, epinephrine
Long term prophylaxis of C1 inh deficiency:
- C1 inh subq or IV (every 3–4 days)
- Lanadelumab subq (kallikrein inhibitor, every 2 weeks)
- Berotralstat PO (kallikrein inhibitor, QD)
How do you treat erythema marginatum?

- No specific therapy for this
- Clinical course is unaltered by treatment of underlying rheumatic fever
- Usually resolves on its own
Name the top 3 causes of acute urticaria in order
Bonus: Definition of acute urticaria
1. Idiopathic
2. URIs
3. Drugs
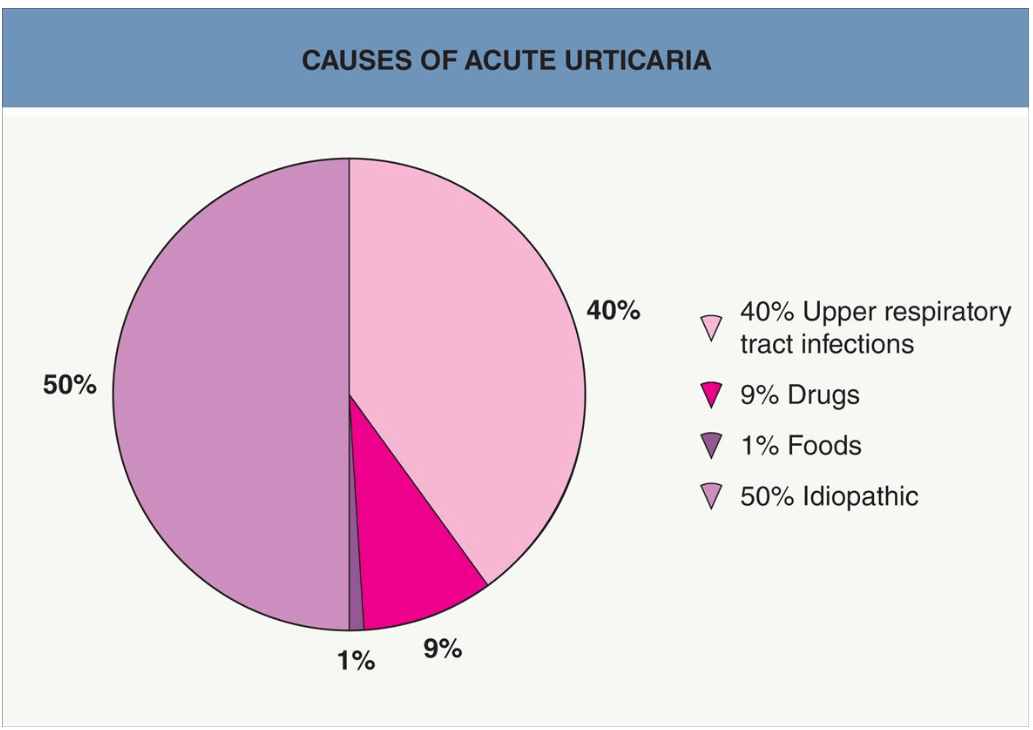
Urticaria that lasts < 6 weeks
See these lesions that each last > 24 hours, with systemic symptoms, what is it most likely, and what disease is associated with it? (Be specific)
Hypocomplementemic urticarial vasculitis, a/w SLE
Urticarial vasculitis:
- Normocomplementemic: Skin limited, idiopathic
- Hypocomplementemic: Usually a/w systemic disease
Females > 50 yo
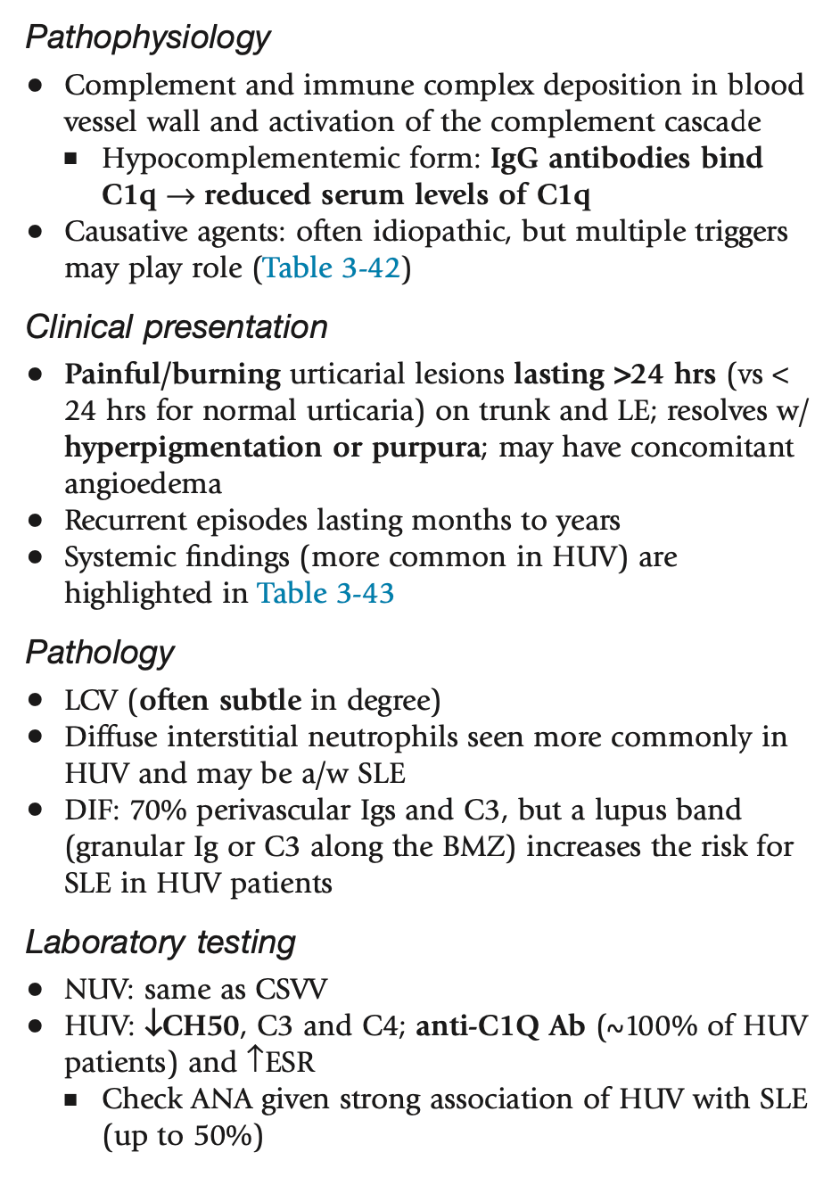
Laboratory workup besides bx: CBC, CMP, UA, viral hepatitis panel, HIV, ASO, ANA, lupus antibody panel, Sjogren's antibody panel, RF, anti-CCP antibody, serum complements, SPEP, cryoglobulins
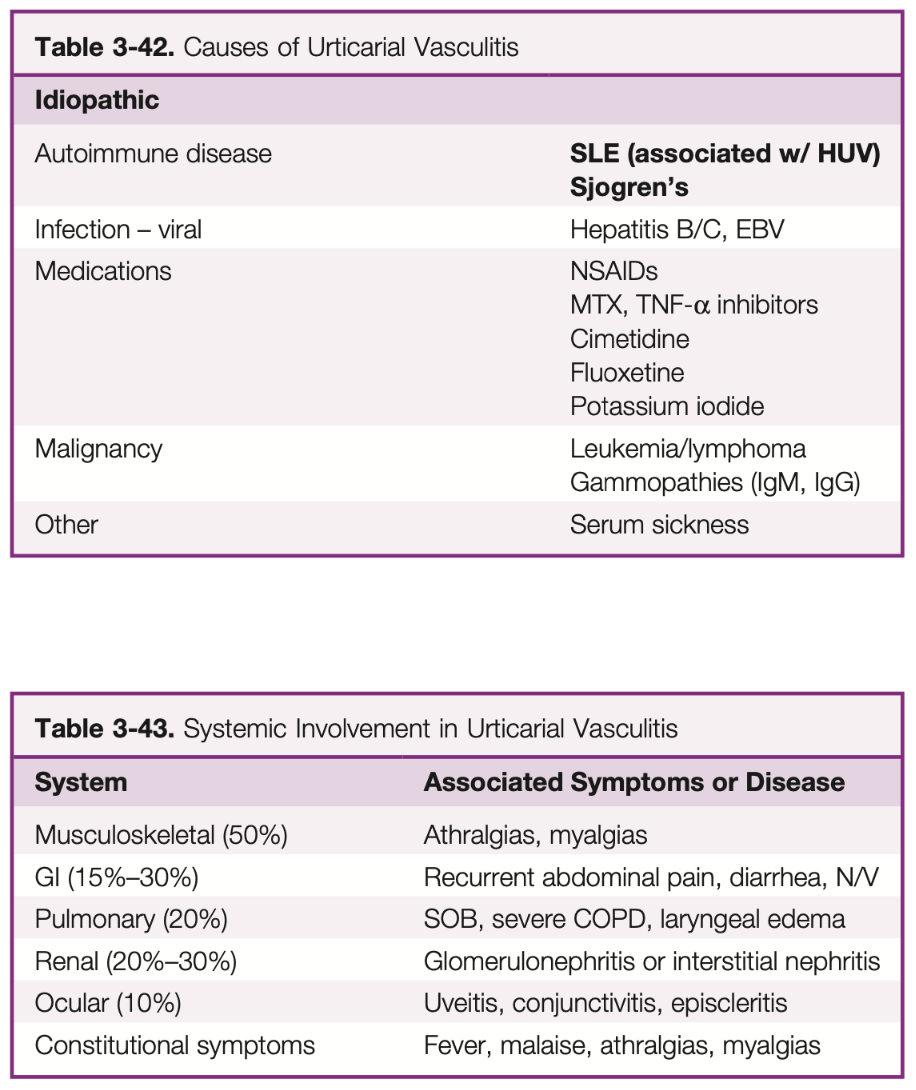
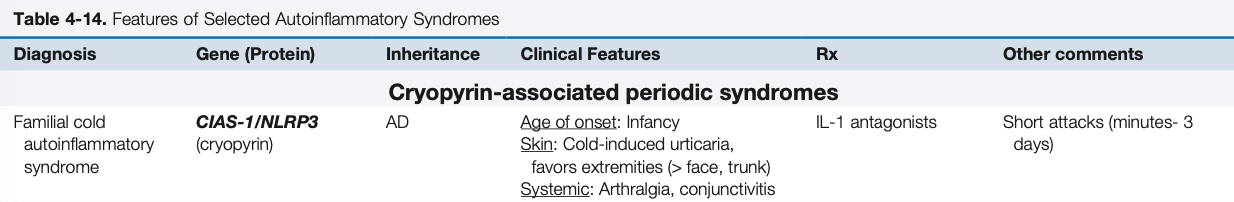
Infant after cold exposure, what gene is likely mutated?
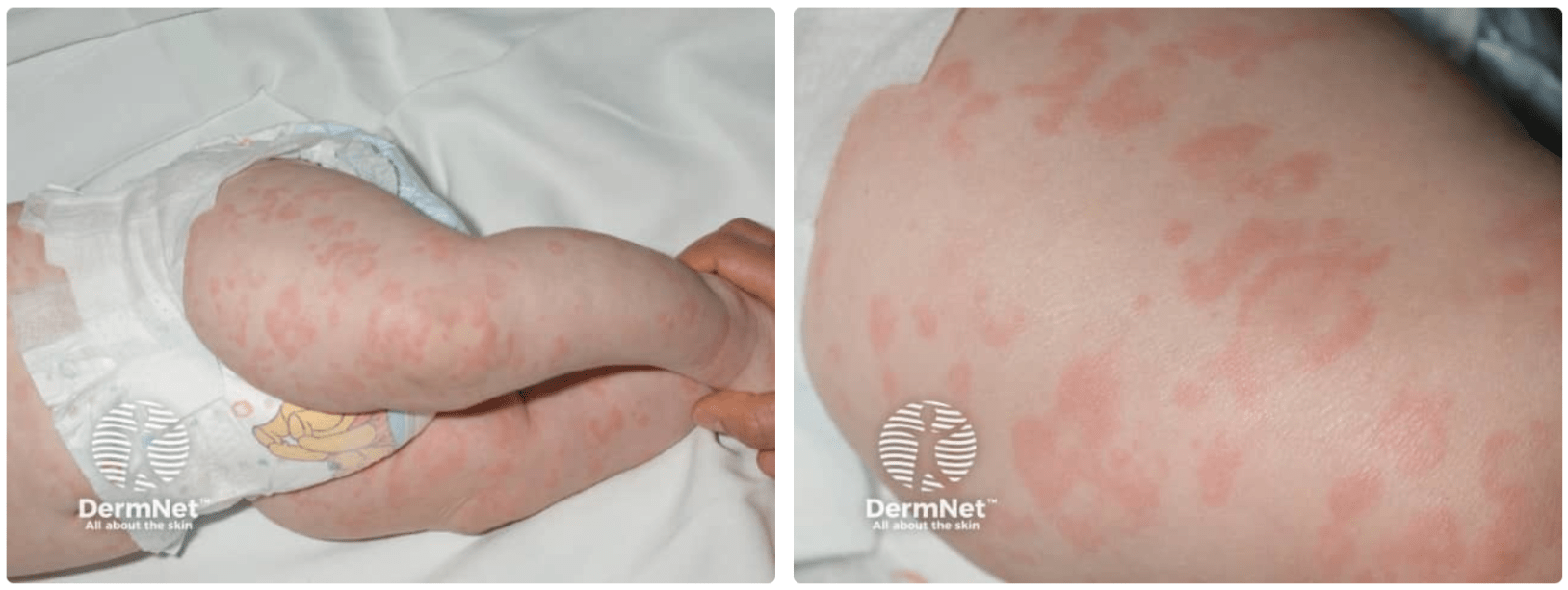
CIAS-1/NLRP3
Familial cold urticaria, AKA familial cold autoinflammatory syndrome (FCAS):
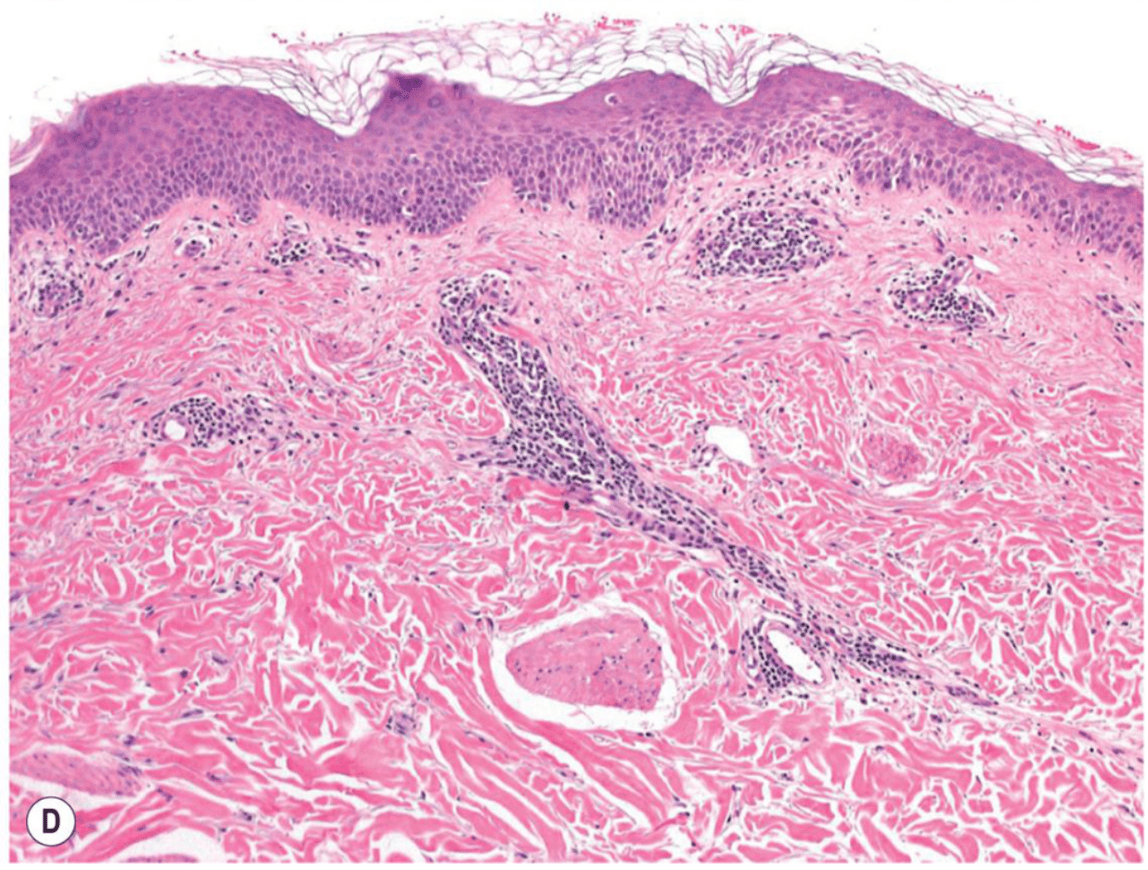
How high can you increase the dose of a 2nd generation H1 antihistamine to deal with urticaria?
Bonus: Which antihistamines are preferred in pregnancy?
Up to 4x the labeled dose
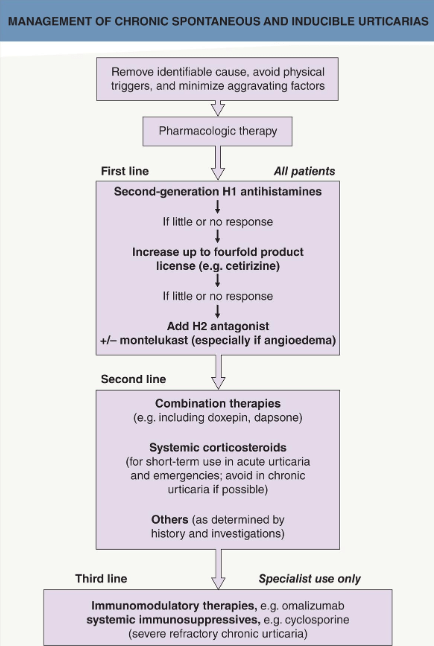
Loratidine and cetirizine are preferred for use in pregnancy, esp in 2nd and 3rd trimester
Non drug therapies:
- Some studies showing success with exclusion of food additives and natural salicylates... but its debatable
- Can induce tolerance with repeated exposure to physical stimulus in physical urticaria
Next stop, figurate erythemas!
But first...
STRETCH BREAK
And the first person to turn on their camera and says something gets 500 points

Name the figurate erythema
Name the disease it's associated with

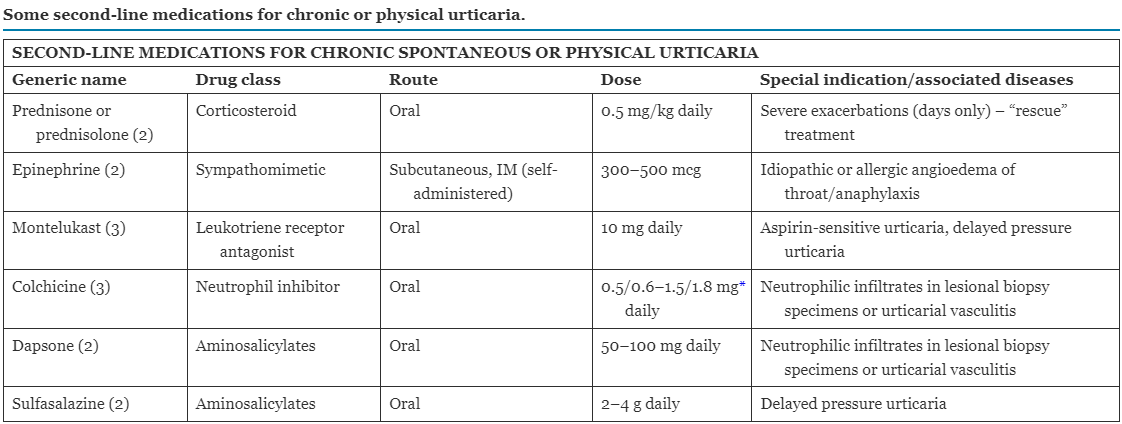
Erythema migrans, associated with Lyme disease
- Usually seen in NE, mid-Atlantic, and Great Lakes parts of the US and northern or eastern Europe
Pathogenesis: Ixodes tick bites you, infects you with Borrelia burgdorferi
Spirochetal lipoproteins trigger innate immune response, Th1 pathway also is activated
1-2 weeks later, from the center of the bite: erythematous, expanding, circular or annular plaque that MAY have bull’s-eye appearance

Center can become violaceous:

Untreated, it lasts < 6 weeks
Rash can also be disseminated if there are multiple tick bites or in disseminated disease:
On path: Superficial and deep lymphoid perivascular infiltrates
Name the top 3 causes of chronic urticaria
Bonus: Definition of chronic urticaria, definition of episodic urticaria
1. Idiopathic
2. Inducible (ie external physical stimuli like temperature, external subtance, etc)
3. Autoimmune processes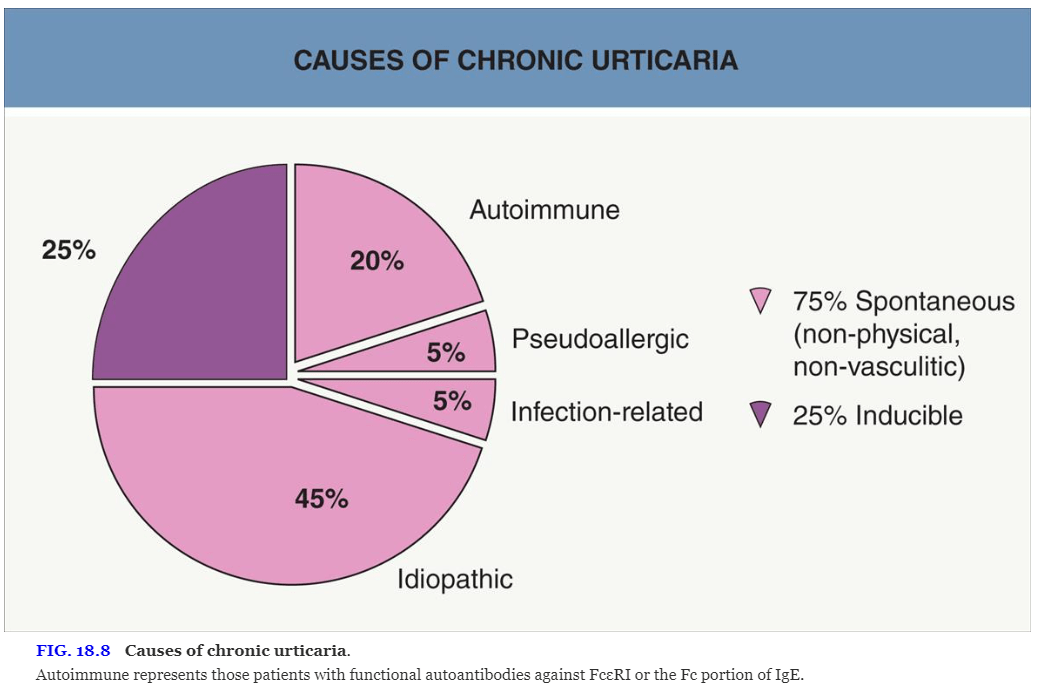
Chronic urticaria: Urticaria lasting >/= 6 weeks that occurs AT LEAST 2x a week off therapy
Episodic urticaria: Urticaria lasting >/= 6 weeks that occurs LESS THAN 2x a week off therapy
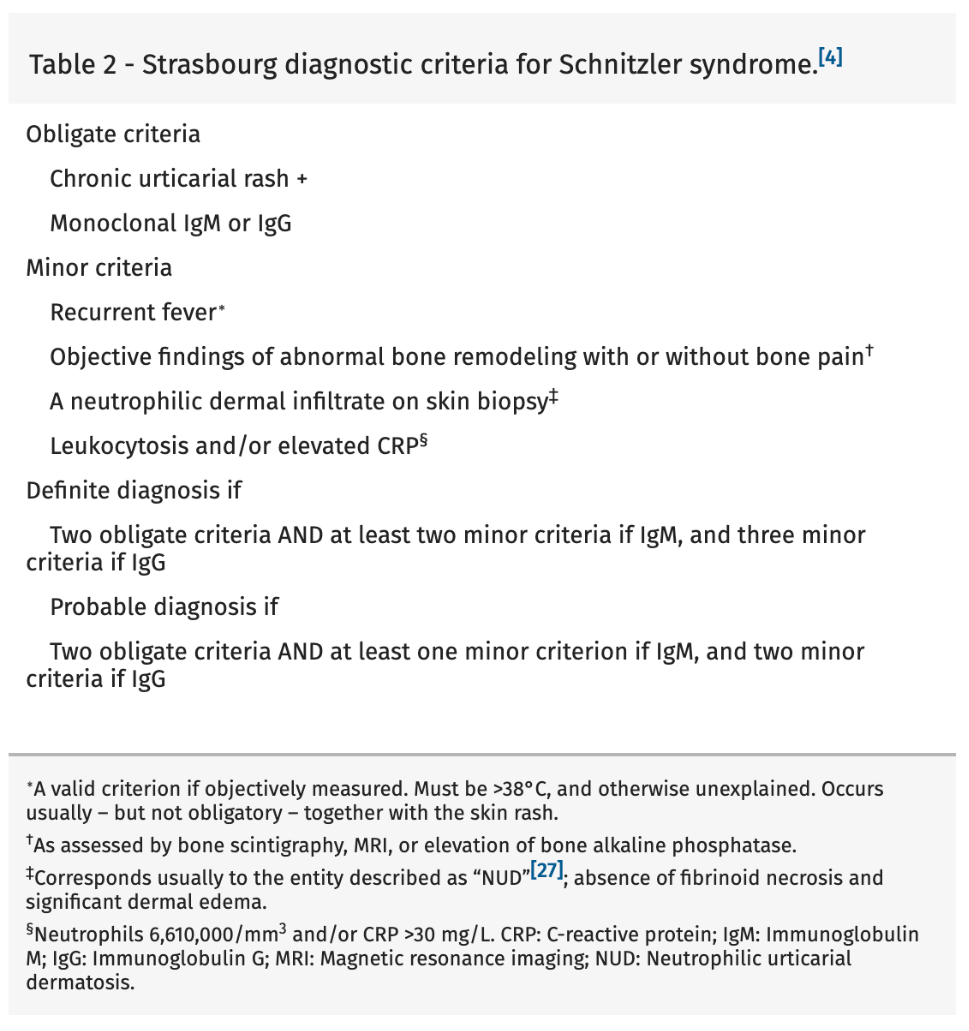
- See this with elevated ESR and IgM gammopathy
Name the koda and a drug (and it's mechanism) that can treat it

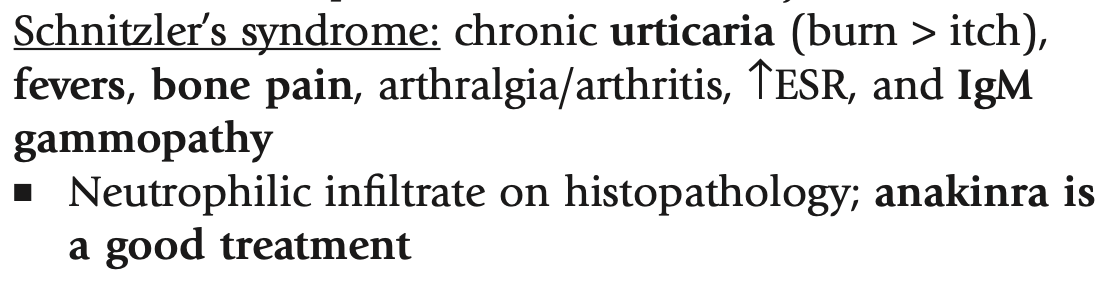
Meds to treat it:
- Anakinra: IL-1 receptor antagonist
- Canakinumab: Anti-IL-1β
- Rilonacept: Anti-IL-1β
Name the exam finding and how long it usually lasts for:

Angioedema, usually lasts 2-3 days
- Swelling in the deep dermis and subq or submucosa
- Can affect oropharynx and rarely the bowel
- Usually normal to faint pink in color and painful, larger, and less well defined than wheals
Quick! You have a patient with severe exacerbation of their urticaria with life-threatening angioedema!
What 2 drugs do you give ASAP?
Epinephrine
Systemic steroids (prednisone or prednisolone)
Name the figurate erythema
Erythema annulare centrifugum
- Peak incidence in 5th decade
- Believed to be a hypersensitivity to an antigen
- Itchy, firm pink papules that expand centrifugally and develop central clearing
- Can have incomplete arcs, polycyclic lesions, or festooned bands
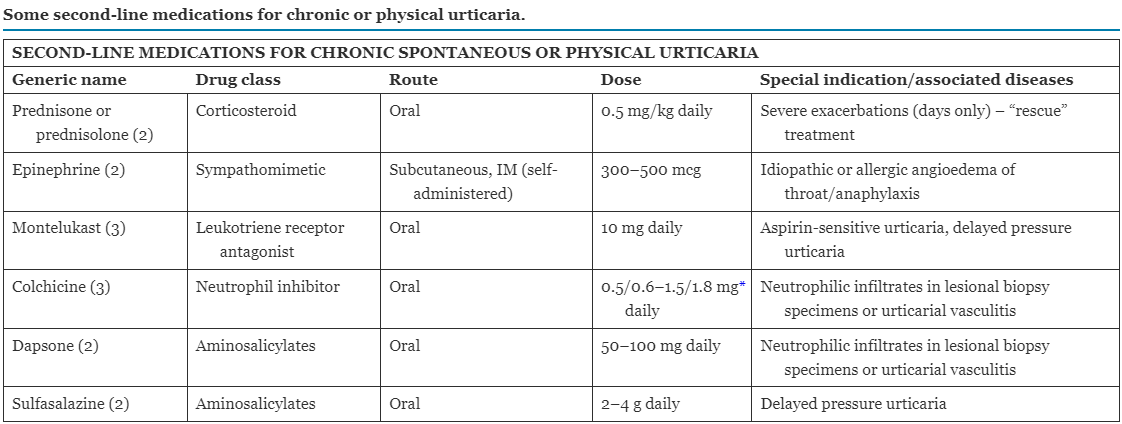
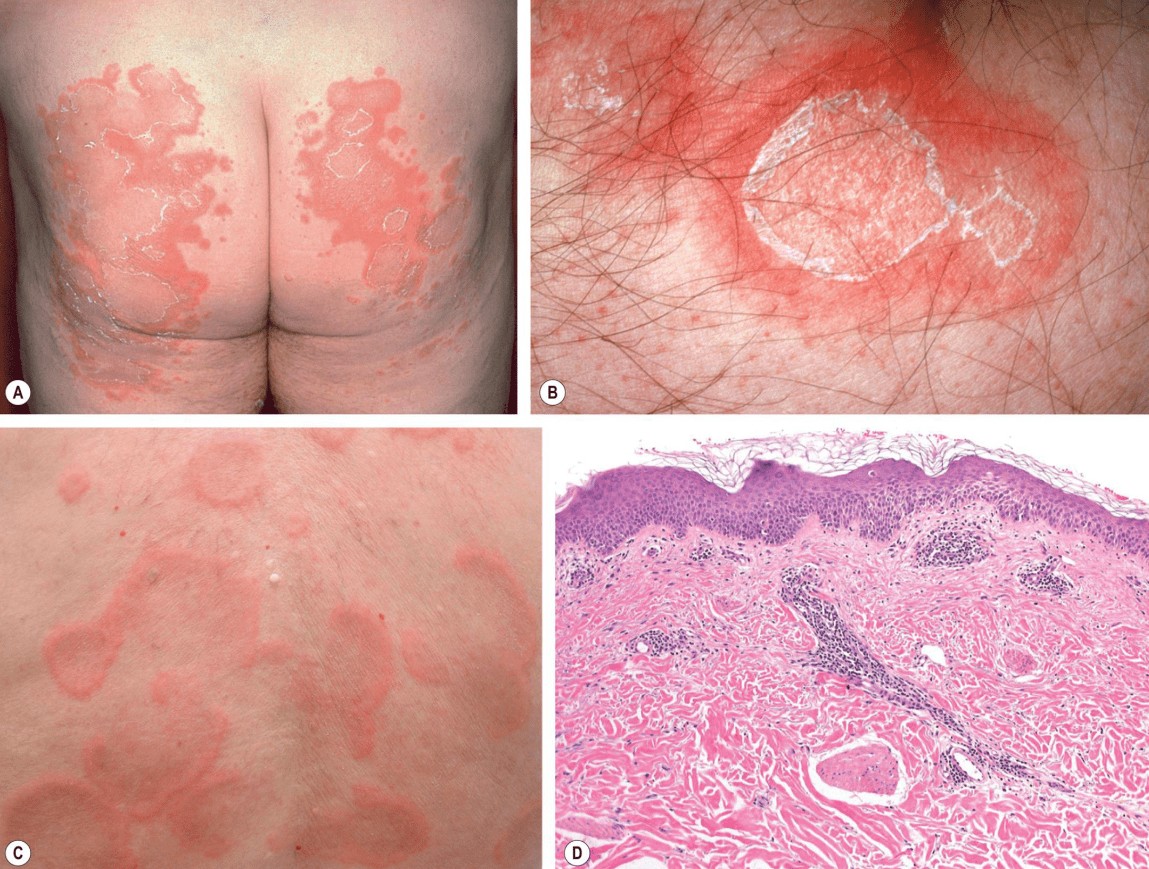
- Lesions can persist for weeks/months
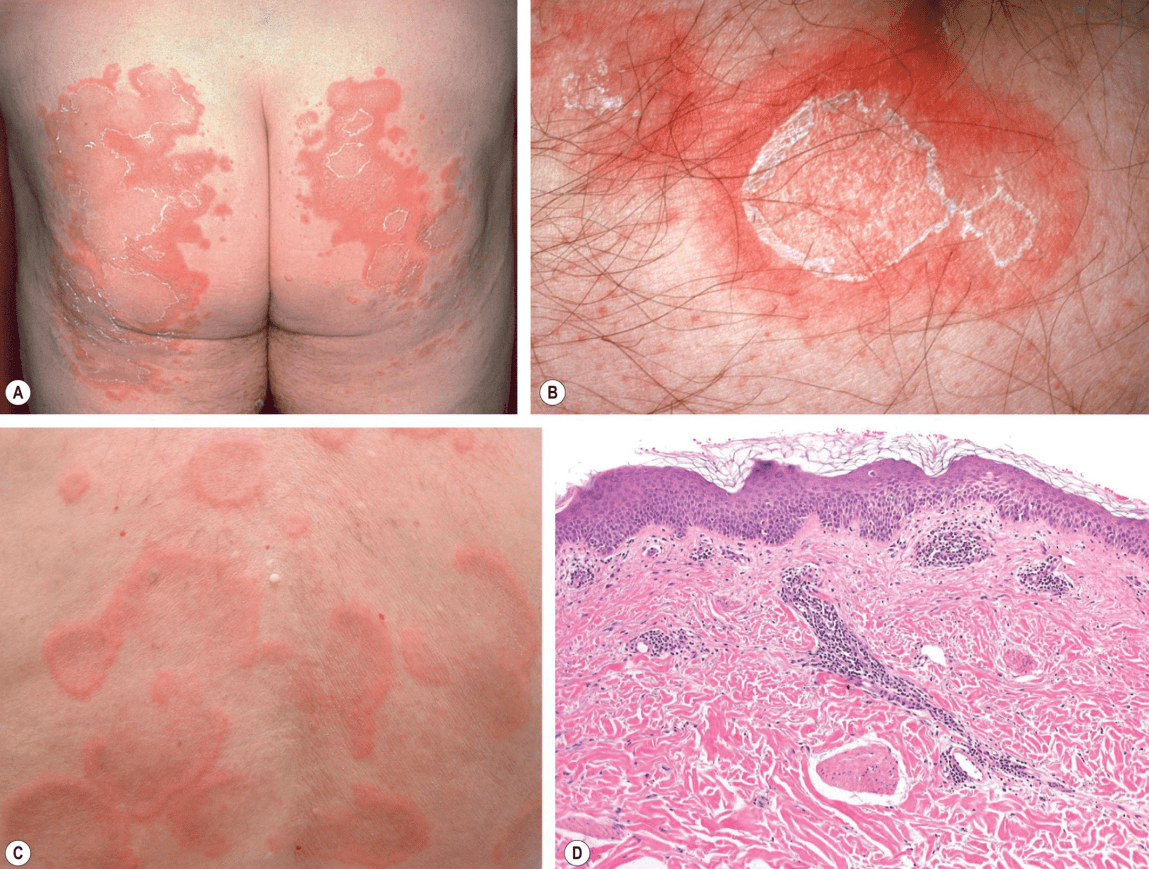
A, B. Superficial form: Minimally elevated lesions with trailing scale with itchiness
C. Deep form: Significant elevation of edges without trailing scale or itchiness
D. Typically pathology of superficial form: Mild spongiosis, microvesiculation, associated focal parakeratosis, mild superficial perivascular lymphohistiocytic infiltrate that forms a tight "coat sleeve"
In deep form: Epidermis is normal. Mononuclear cell infiltrate with a sharply demarcated perivascular arrangement in mid and lower dermis, resulting in their more elevated appearance and absence of scale
Name the 3 phases of Lyme Disease and their characteristics

- Regional lymphadenopathy
2. Early disseminated:
- Meningitis, neuritis, bell palsy, radiculoneuropathy
- Arthralgia, myositis
- AV block, myopericarditis, pancarditis
- Lymphadenopathy
- Conjunctivitis, iritis
- Hepatitis
- Microscopic hematuria or proteinuria
3. Chronic:
- Encephalopathy, encephalomyelitis, neuropathy
- Chronic arthritis
Name 4 autoimmune conditions associated with chronic spontaneous urticaria
- Autoimmune thyroid disease
- Vitiligo
- DM1
- Rheumatoid arthritis
- Pernicious anemia
Name the koda
Name the two more common types of this koda and their definitions
Bonus: Name 2 rarer types of this koda
Dermatographism = Dermographism
- Simple immediate dermatographism: Asymptomatic wheal development shortly after stroking the skin
- Symptomatic immediate dermatographism: Itchy wheal development shortly after stroking the skin
Bonus:
- Delayed dermatographism: Wheal development at least 30 minutes after stroking skin
- Red dermatographism: Wheal development after rubbing (not stroking) the skin
- Cholinergic dermatographism: Small punctate wheals, triggered by both mechanical stimulation and cholinergic factors
- Localized dermatographism: Only occurs on specific parts of the body
- Darier’s sign: Dermatographism after rubbing cutaneous mastocytosis
What ONE question (found in Bolognia) could you ask your patient that would change diagnosis/management of chronic urticaria?
How long do individual wheals last?
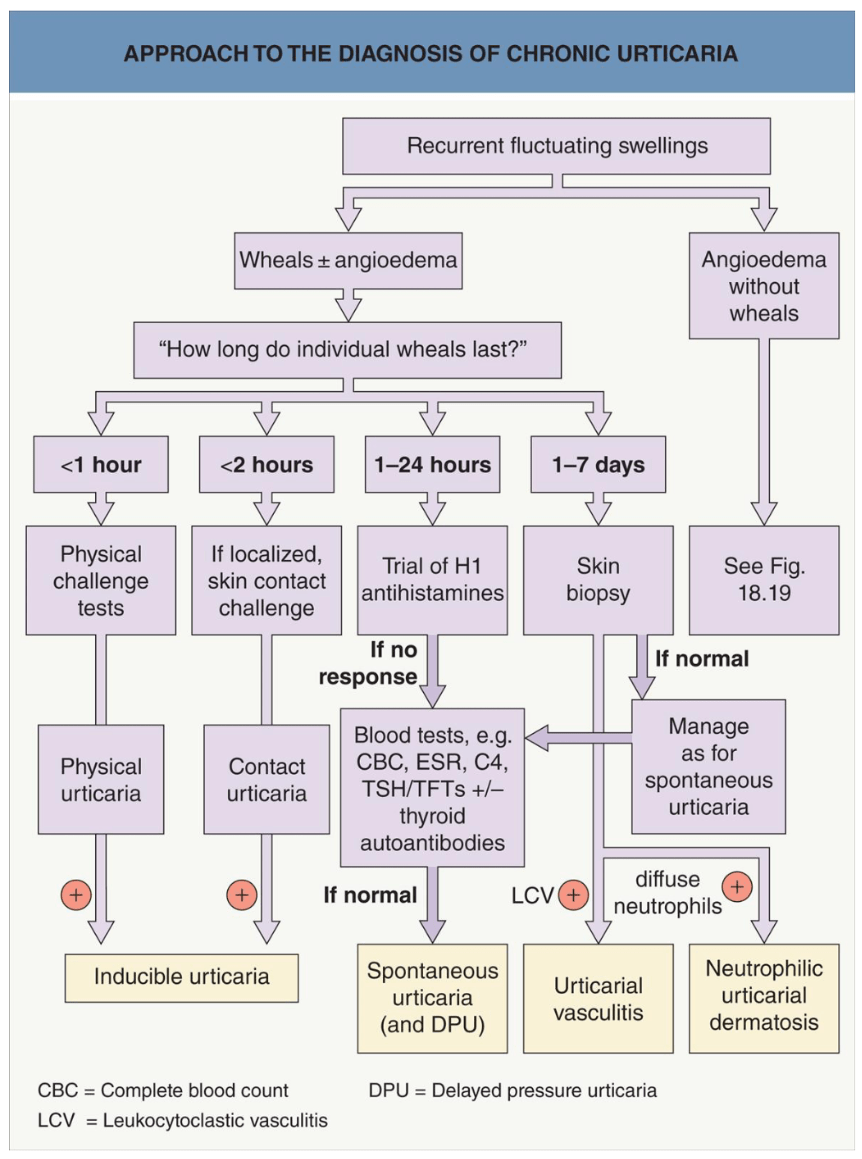
Examples of utilities of testing:
- CBC w/ diff: Eosinophilia of intestinal parasitosis
- ESR: Normal in CSU, elevated in urticarial vasculitis
- TFTs and thyroid autoantibodies: Abnormal in autoimmune urticaria
So you've tried your first line and 2nd line therapies and now you're onto omalizumab for CSU...
Wait what is omalizumab and how does it work?
Bonus: If omalizumab doesn't work, what else can you try for CSU?
Omalizumab:
- Humanized anti-IgE monoclonal antibody
- Usually given for 6 months before being discontinued but longer courses can be required
Bonus:
Other treatments you can try include cyclosporine (generally the next step) followed by (in no particular order) methotrexate, MMF, azathrioprine, and a BTK inhibitor coming soon to a pharmacy near you
Name 2 infectious associations of EAC
Name 2 drug associations of EAC
Infectious associations of EAC: Dermatophytes, fungi (Candida, Penicillium), viruses (poxvirus, EBV, varicella–zoster virus, HIV), parasites, ectoparasites
Drug associations of EAC: diuretics, NSAIDs, antimalarials, finasteride, amitriptyline, nivolumab, sorafenib, rituximab, pegylated interferon-α-2a plus ribavirin, ustekinumab
Other associations: Crohn disease, pregnancy, autoimmune endocrinopathies, hypereosinophilic syndrome, malignancy
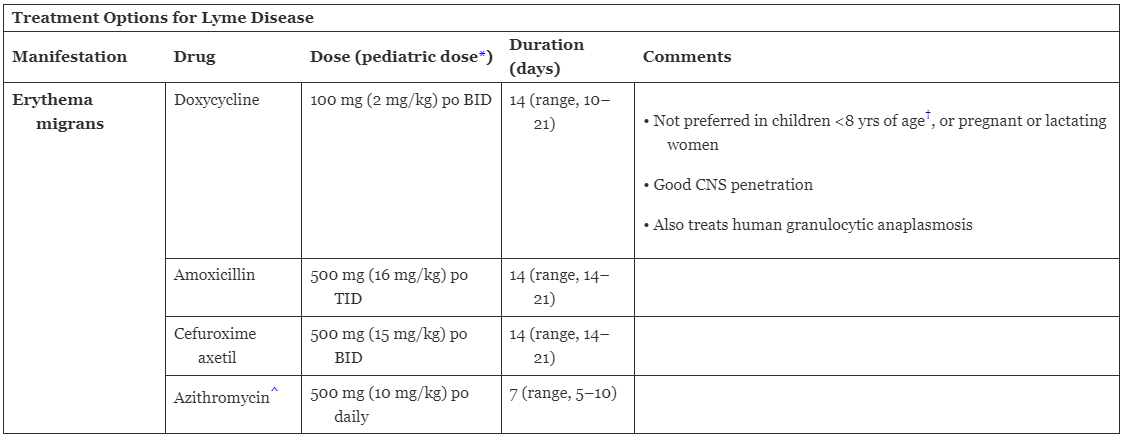
Name 2 possible treatments of erythema migrans (when in the early stages)
Name the 6 most common categories of stimuli of inducible urticaria (in no particular order)
- Mechanical
- Temperature change
- Sweat / stress
- Contact
- Solar
- Aquagenic
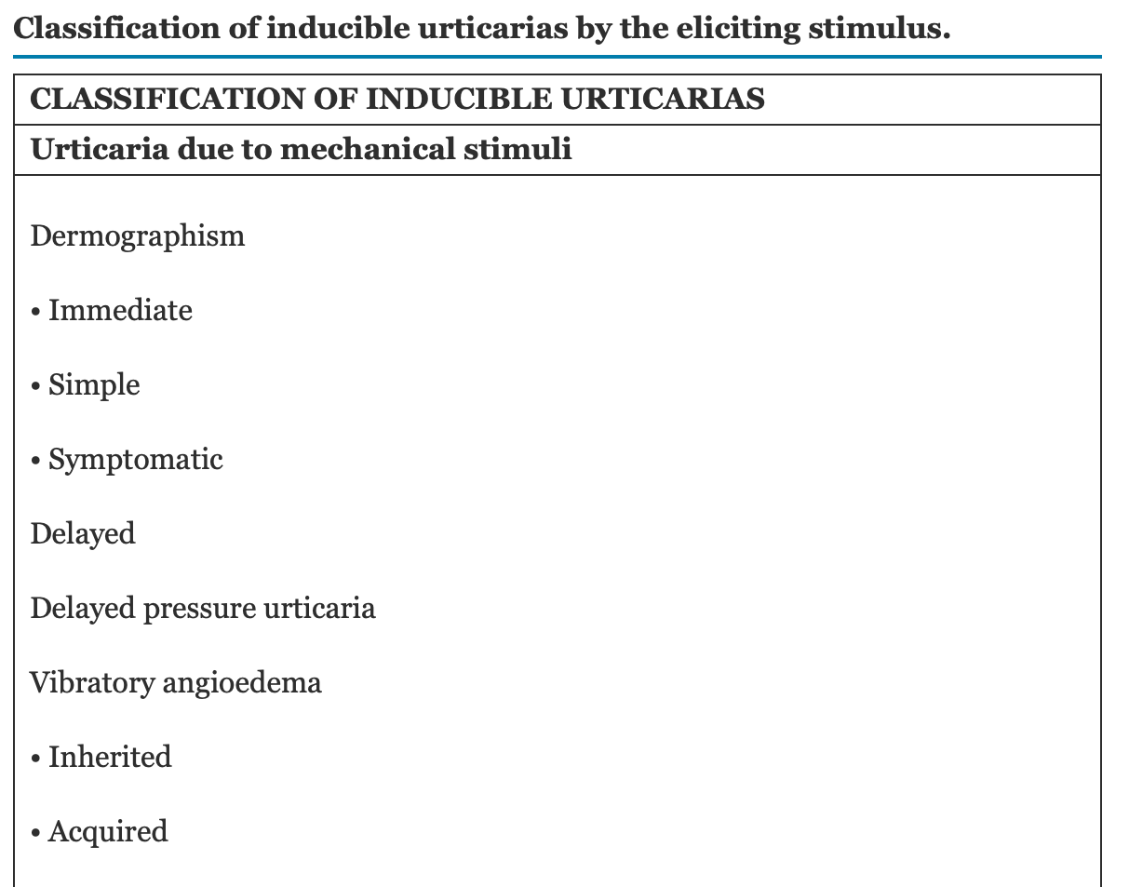
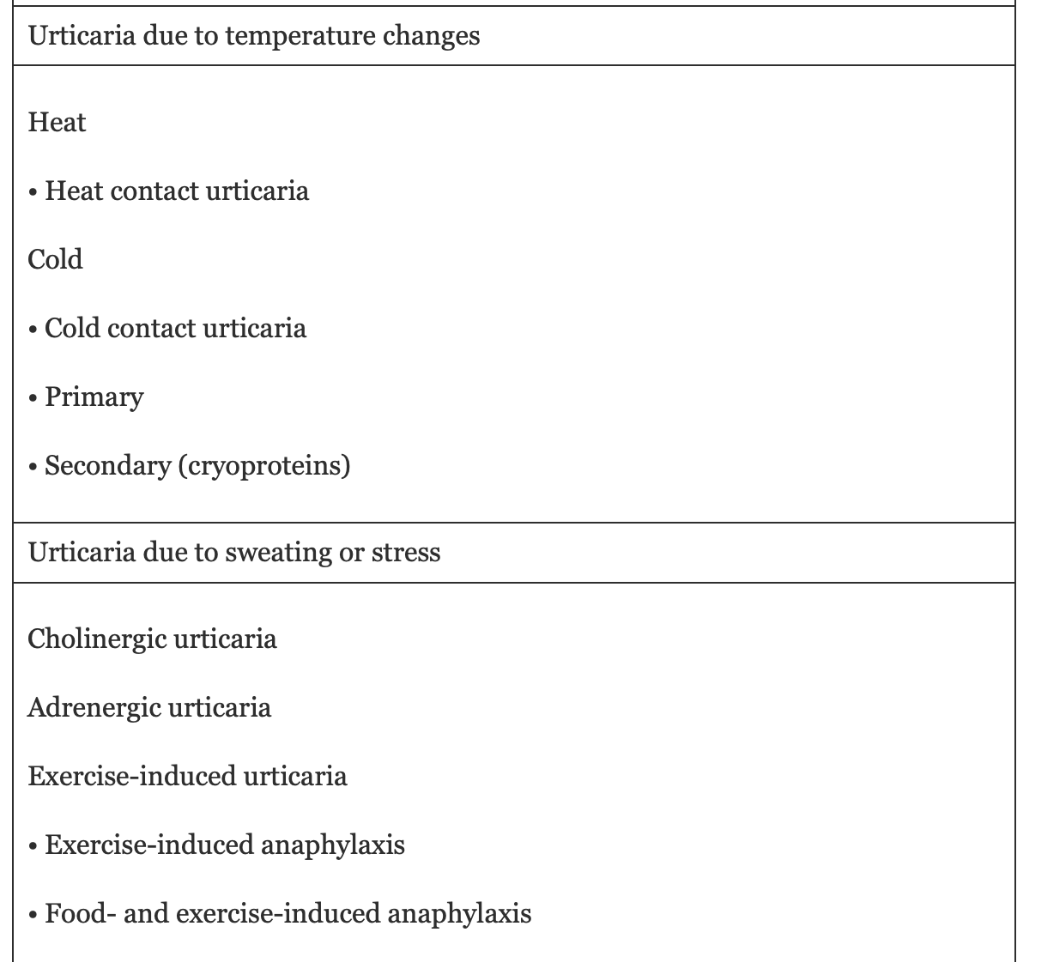
Generally localized to stimulated area of skin, but sometimes there can be a systemic change (ex: change in body temperature) that triggers widespread urticaria
Name the koda:
Adrenergic urticaria: Blanched vasoconstricted halos around wheals
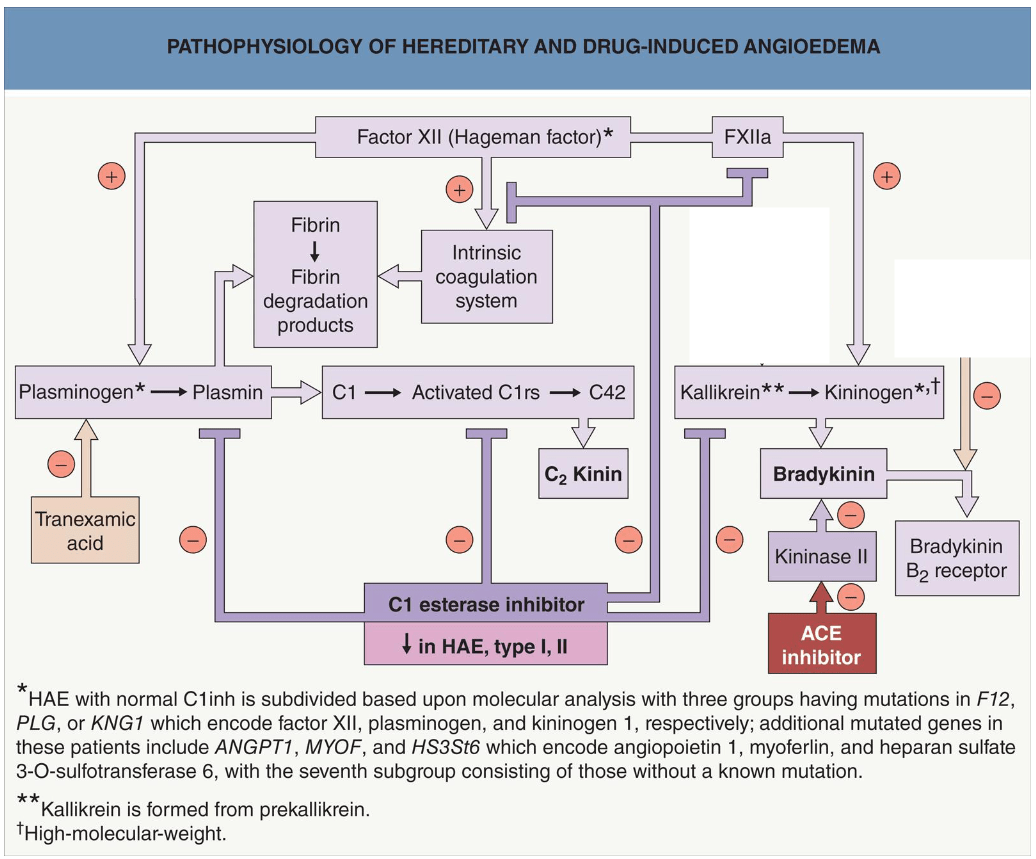
Gene that is mutated in the first 2 major forms of hereditary angioedema (HAE), and its typical inheritance pattern when mutated
Bonus points: Difference between HAE types 1, 2, and 3
C1NH/SERPING1, autosomal dominant inheritance
HAE type 1: Reduced levels of C1 esterase inhibitor
HAE type 2: Reduced function of C1 esterase inhibitor
HAE type 3: Normal C1 esterase inhibitor, activating mutation in Factor XII
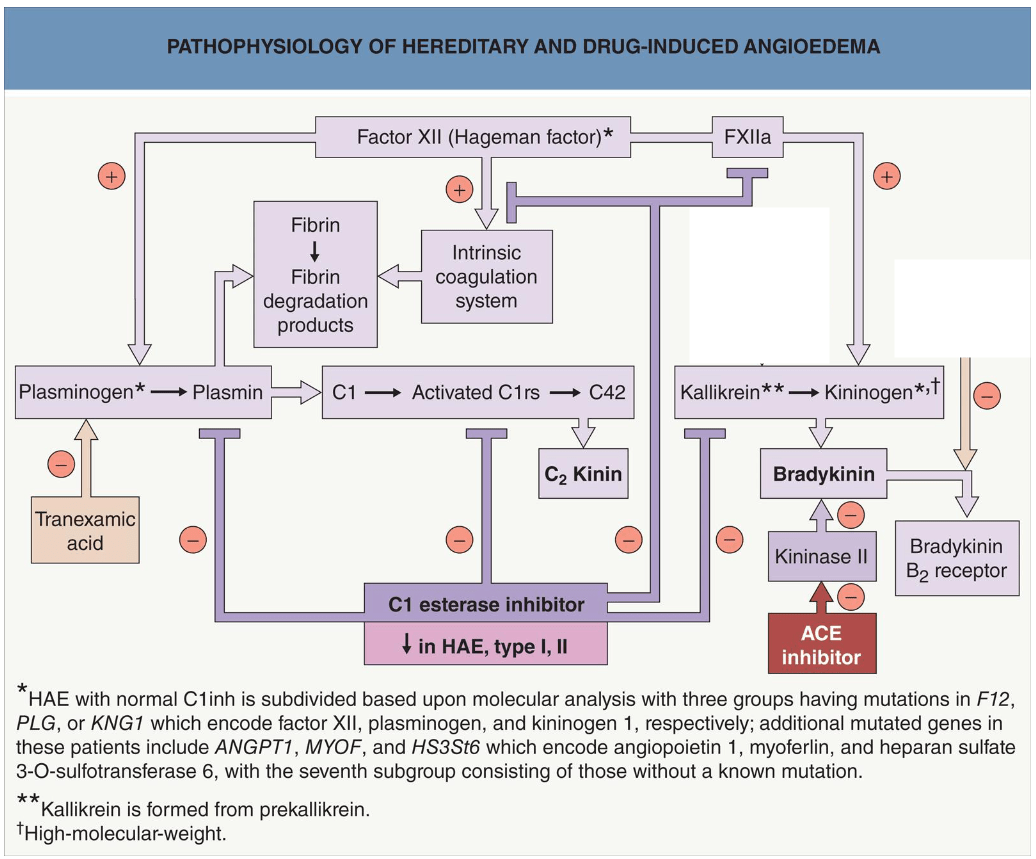
Name 3 kallikrein inhibitors
Bonus: Name their typical uses
Bonus: Name how they are administered
Ecallantide (subq): Emergency treatment of HAE
Lanadelumab (subq), Berotralstat (oral): Prevention of HAE attacks
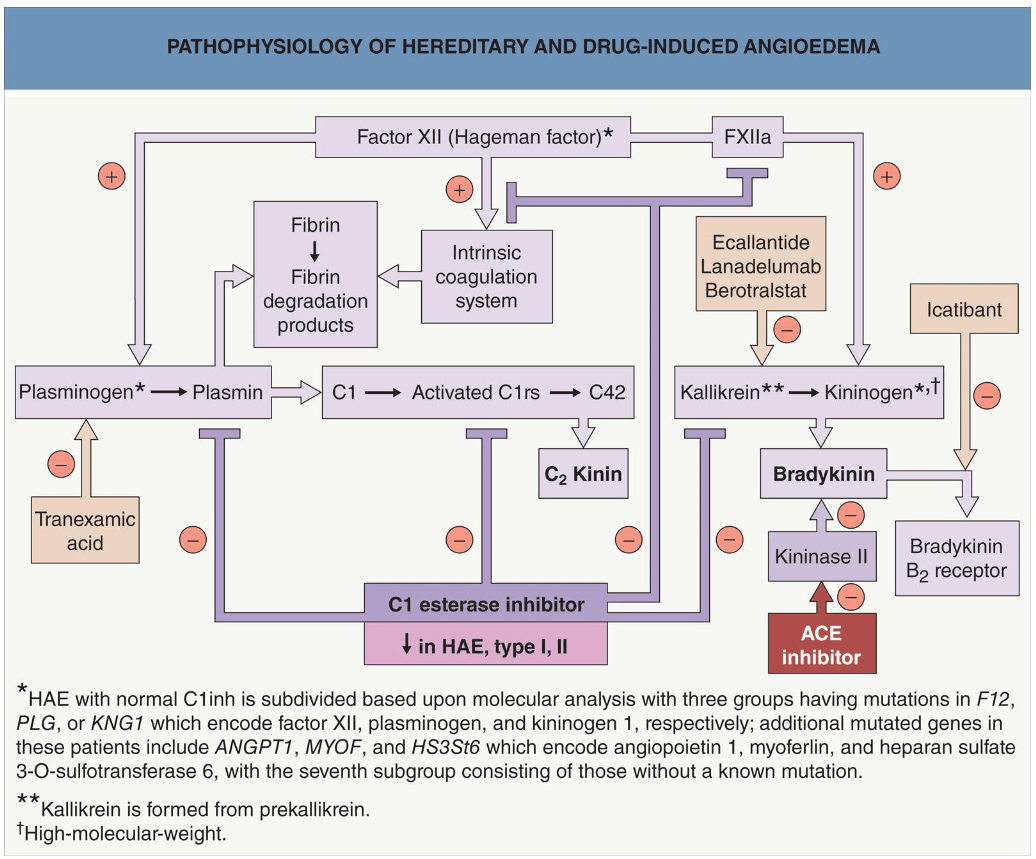
Kallikrein converts HMW kininogen to bradykinin which promotes angioedema
How to treat EAC?
- Deal with the underlying disorder
- Topical corticosteroids, sometimes empiric use of antibiotics or antifungals
Last figurate erythema, I promise, what is it and what is it associated with:

Erythema gyratum repens
- Multiple, annular or polycyclic, erythematous lesions with leading scale and rapid advancement (up to 1 cm per day)
- Wood-grain or zebra-like pattern, rings within rings
- Can also see associated ichthyosis, palmoplantar keratoderma, and peripheral eosinophilia
- Associated with cancer (lung > breast > esophageal > stomach), lesions usually develop between 1 year prior to 1 year after cancer diagnosis
- Believed to be immune mediated cross-reaction between tumor and cutaneous antigens
- Pathology: Nonspecific, hyperkeratosis, focal parakeratosis, moderate patchy spongiosis and a mild, perivascular lymphohistiocytic infiltrate
- Treatment: Treatment of the underlying cancer
- If it comes back after cancer treatment, the cancer likely came back