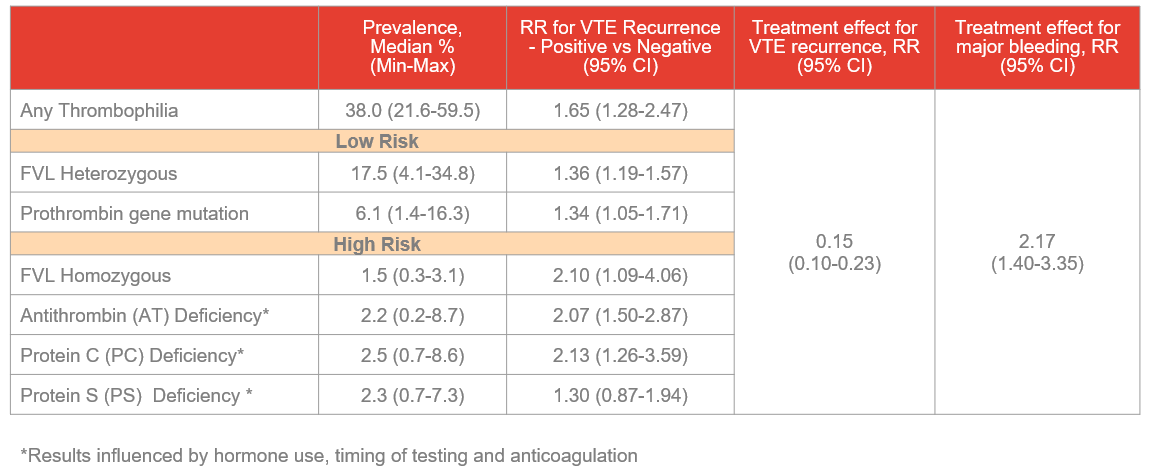
What are the two most common hereditary hypercoagulable conditions?
Factor V Leidin (note, heterozygous most common, but often unaffected)
Prothrombin
What type of cancer is treated with all-trans retionic acid (ATRA)
APML - usually characterized by the t(15;17) translocation which merges PML-RARa fusion protein, which repressers differentiation of promyelocytes -> granulocytes
ATRA binds to the altered RARα portion of the PML-RARα fusion protein, releating the transcriptional repression, allowing promyelocytes to resume normal differentiation into mature granulocytes.
What is now first line treatment for mild asthma
ICS-containing therapy (avoid SABA monotherapy - increased mortality, exacerbations)
First line low dose ICS-formeterol (expensive, hard to get for most patients)
Alt is ICS-SABA
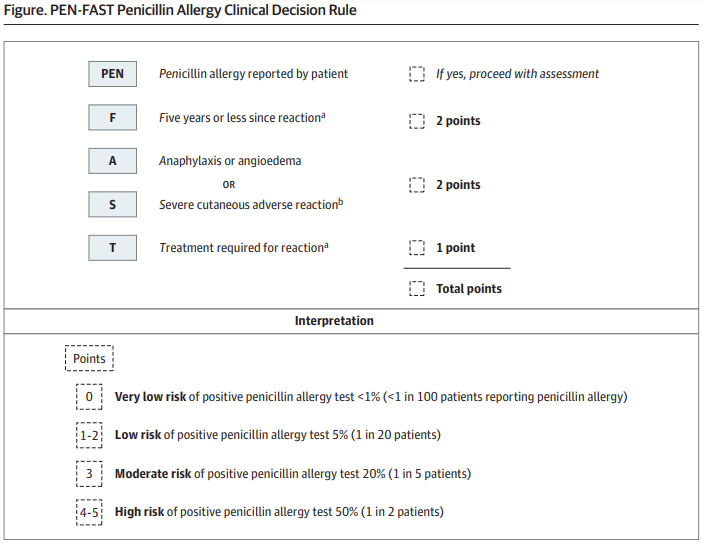
What risk stratification tool can you use to determine a patient's risk of penicillin allergy?
PEN FAST
A 28-year-old man presents for a routine check-up. He works as a software engineer and lives alone. His mother expresses concern that he has “difficulty connecting with others” and “takes things very literally.” He reports no history of psychiatric illness but notes that he has always struggled with small talk, prefers routines, and becomes anxious when plans change. He has an intense interest in astronomy, spending hours memorizing star charts. On examination, he makes limited eye contact, has a flat affect, and demonstrates minimal gestures when speaking. He is oriented, with normal speech, cognition, and memory.
What is the most likely diagnosis and the redacted eponym?
Autism spectrum disorder (high functioning)
Asperger's Syndrome
Which neurotransmitter requires vitamin C for synthesis?
Dopamine -> mood dysregulation
Norepi -> autonomic instability
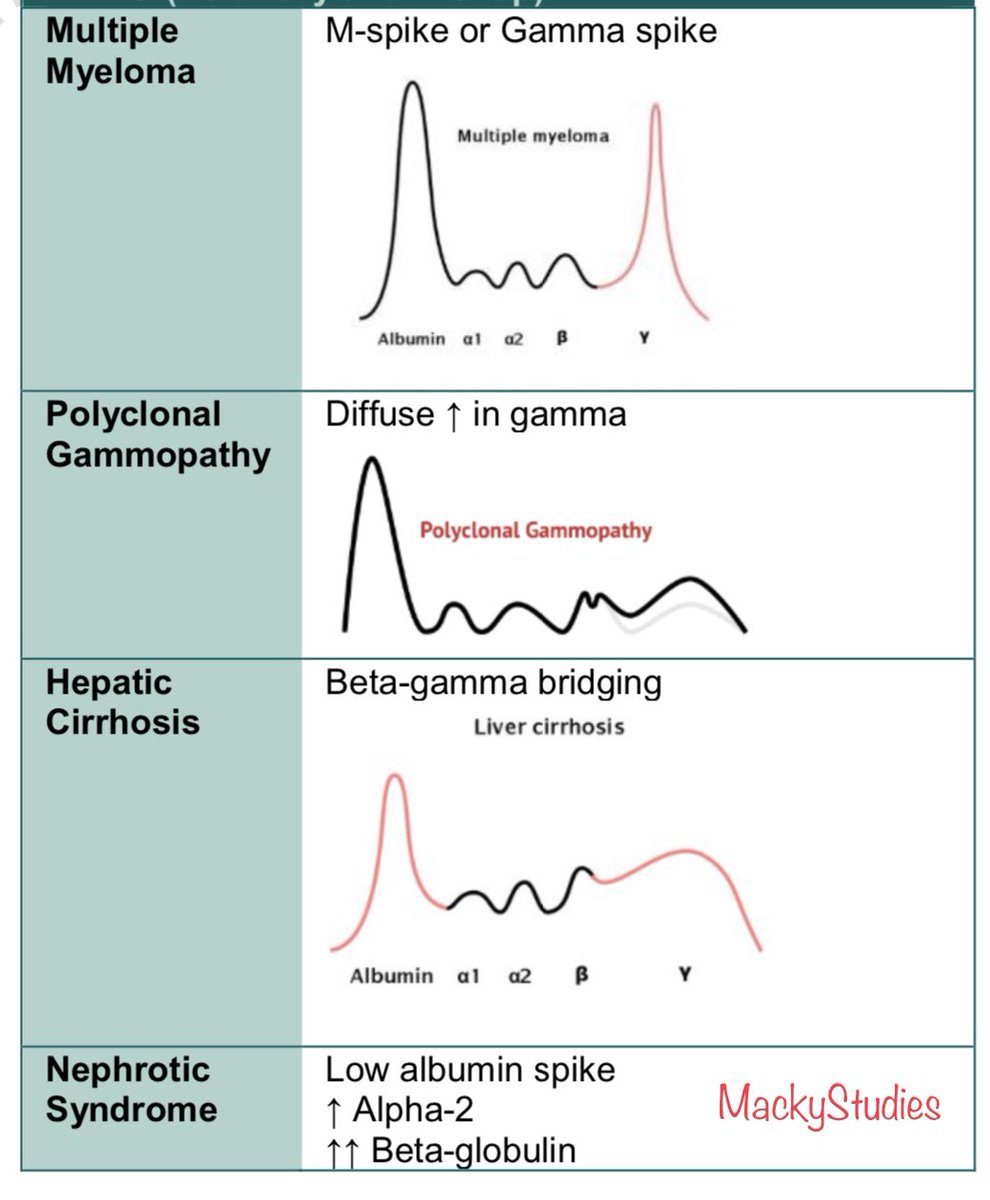
Name 2 causes of a polyclonal gammopathy (increase in some combination of IgG, IgM, IgA)
Polyclonal = think autoimmune or inflammatory!
E.g. viral infxn, liver disease, solid tumors, acute phase reactants
This asthma medication has a black box warning for psychiatric side effects
Montelukast - careful in patients w/ psych history, monitor for side effects
Class: Leukotriene receptor antagonist (LTRA)
Warning: Risk of serious neuropsychiatric events including:
Agitation
Depression
Suicidal thoughts and behavior
Sleep disturbances
How should pregnant patients allergic to PCN diagnosed with syphilis be treated?
Penicillin desensitization and treatment with penicillin
IgE-mediated hypersensitivity is established and need for drug is confirmed
Goal = “controlled anaphylaxis”
- Drug is given at a concentration and rate that will cause drug-specific IgE-armed mast cells to degranulate at low rates that do no precipitate a systemic reactions
Desensitized state will only last for up to 4 half-lives of the drug
- Sensitivity is assumed to return after and future treatment courses require repeated desensitizations
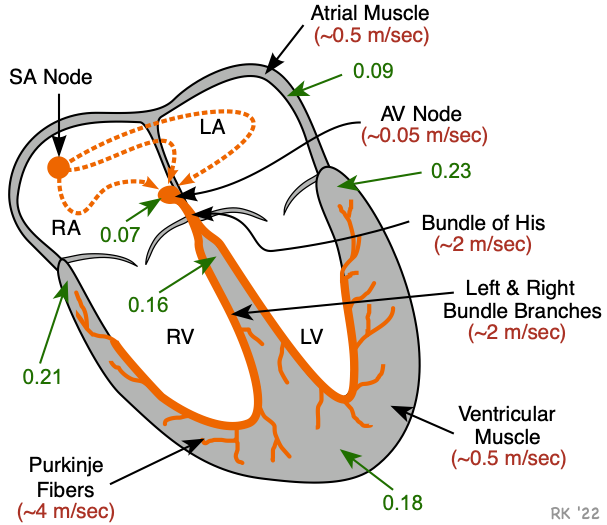
What is the rhythm, and where along the cardiac conduction system is the issue?
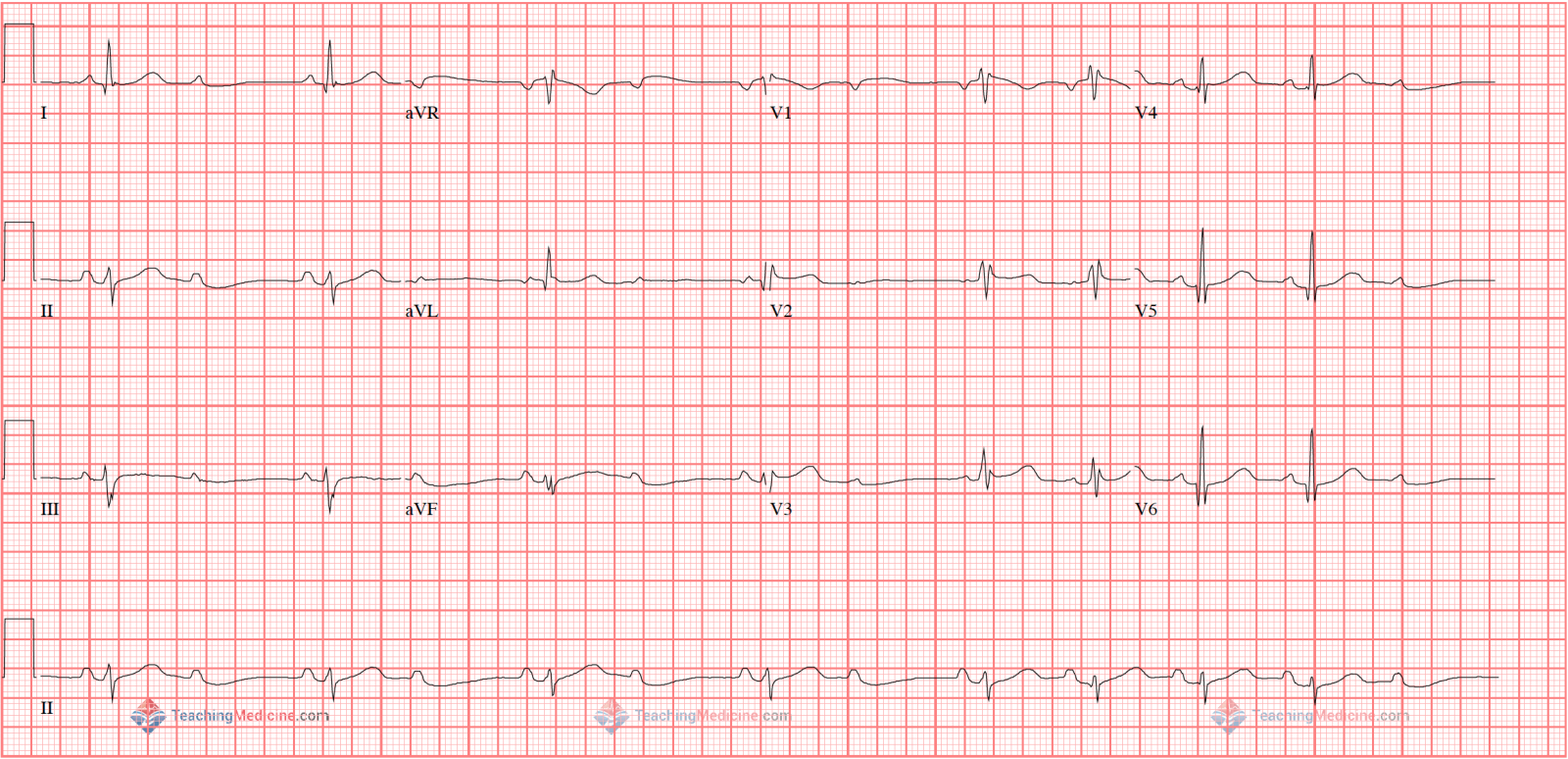
Type II AV block (Mobitz II)
in or below the Bundle of His, named for Willhelm His Jr
Preferred name Atrioventricular Bundle
25% narrow QRS in Bundle
75% wide QRS below Bundle (Purkinje System)
Interpret RHC numbers
RAP 7
PAP 80/40
mPAP 53
PCWP 16
CO 3.1
CI 2.1
PVR 12
Severe (mPAP > 45)
Post-capillary (PCWP > 16, PVR < 3)
Pulm HTN
With reduced cardiac output (4-8).
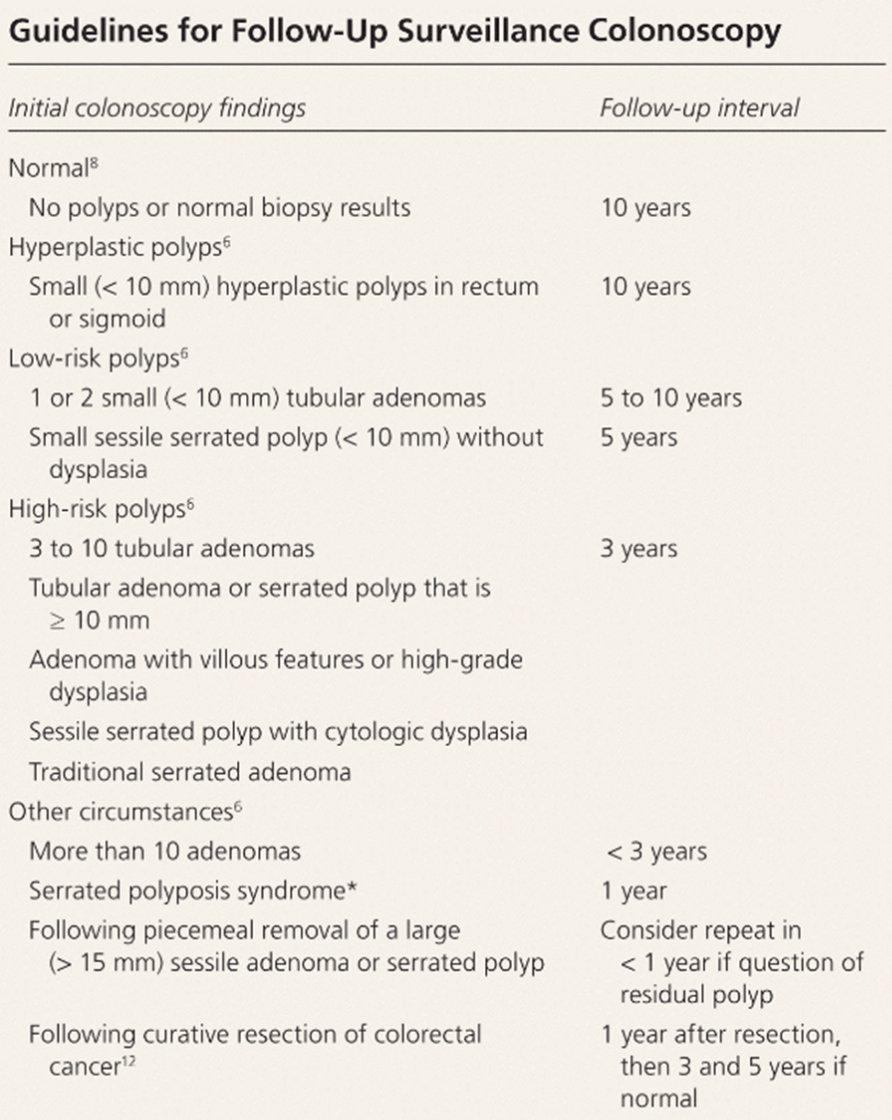
A patient undergoes screening colonoscopy and is found to have 2 tubular adenomas measuring 9mm and 1.4cm. Per guidelines when should they have follow-up surveillance colonoscopy?
3 years
Name 4 asthma syndromes
Allergic Asthma
Cough-variant asthma
Exercise-induced bronchoconstriction
Occupational
Reactive Airways dysfunction syndrome
Aspirin-Exacerbated respiratory disease
ABPA
What testing should you send when working up a patient for chronic urticaria?
CBC, CMP, TSH
thyroid antibodies (often have of develop subclinical/clinical hypothyroid)
ESR/CRP - prognostication
SPEP - MGUS often comorbid
Alpha-gal???
A 26-year-old man is evaluated for a 1-week history of pain and swelling in the left ankle, along with pain in the toes and tenderness in the left heel. Three weeks ago, he returned from a vacation in Central America. Before returning home, he experienced 4 days of diarrhea that spontaneously resolved. Current medication is acetaminophen as needed.
On physical examination, vital signs are normal. The left ankle is swollen, with reduced range of motion. Several toes are swollen, as shown, and the Achilles insertion on the left is swollen and tender. CRP is 3.5.

Which of the following is the next best step in management?
Azithromycin
HLA-B27 testing
Piroxicam
Stool cultures for enteric pathogens
What is the eponym associated with this disease?
Reactive arthritis, formerly Reiter's disease
Piroxicam
50-80% of patients with reactive arthritis are HLA-B27 positive, but does not change management
69 y/o w/ hx severe AS presents with UGIB. EGD + colonoscopy are normal. What is the most likely diagnosis and what is its pathophysiology?`
Heyde syndrome
Shearing of vWF through severe stenotic aortic valve -> acquired vWF deficiency -> promotes angiodysplasia/AVM formation -> UGIB
20% of AS
Most commonly jejunum, but also duodenum/ileum (EGD only reaches duodenum)
Waldenstrom Macroglobulinemia is characterized by monoclonal production of ___ and can present with ____ syndrome which requires emergent treatment
IgM
Hyperviscosity syndrome:
characterized by altered mental status and diverse central nervous system symptoms, dilated retinal veins on funduscopic examination, and mucosal bleeding from impaired platelet function and dysfibrinogenemia, require emergent plasmapheresis to remove excess IgM
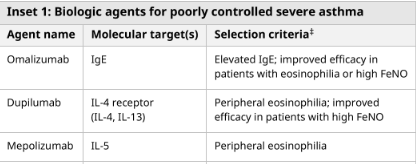
For patients with severe asthma, omalizumab can be used if ____ is/are high; Mepolizumab can used if ___ is/are high
You are on a long call and admitting a patient for angioedema. She was on an ACE inhibitor for 5 years prior to this presentation. You arrive at the bedside, and the patient notes that the swelling of her tongue and lips continues to worsen, despite the antihistamines, methylprednisone and epinephrine that the ED has given her. There is no stridor or respiratory distress. What further treatments would the patient benefit from?
Transexamic acid
Icatibant - Anti-bradykinin
C1-INH, FFP and anti-kallikrein also viable, but above 2 are more commonly available
Histamine-mediated angioedema - allergic type, responsive to anti-histamine/epi/steroids
Bradykinin-mediated angioedema - non-responsive to steroids/anti-histamines - ACEi angioedema and CI Esterase def
40 y/o F presents with SOB, AKI and diffuse GGO on chest CT. Workup is revealing for a positive antibody to PR3, and a negative MPO antibody. What is the eponym and first-line treatment for the severe version of her condition?
Formerly wegner's granulomatosous - preferred Granulomatosis with polyangitis
Severe disease - pulse steroids + rituximab, cyclophosphamide as an alternative.
Some patients also benefit from PLEX
Non-severe steroids + methotrexate
What workup should a 40 year old man with newly diagnosed iron deficiency anemia have done (4)?
Assume normal CMP + rest of CBC.
Celiac - TTG IgA + IgA level
H pylori
EGD + Colonoscopy
A 40-year old woman is evaluated at follow-up for stage I endometrial cancer diagnosed 6 weeks ago now s/p TAH-BSO is found to have MSH2 mutation on genetic testing. Colorectal cancer was diagnosed in her mother at age 55 years and her maternal aunt at 60 years.
What is the most appropriate screening strategy at this time?
Lynch Syndrome
EGD + Colonoscopy
This patient fulfill’s the Amsterdam II criteria for diagnosis of Lynch Syndrome. At least 3 family members with a Lynch syndrome-associated cancer in 2 successive generations with at least 1 first degree relative before the age of 50. Patients with Lynch syndrome should be screened with colonoscopy beginning at ages 20 to 25 years (or 2-5 years before earliest cancer diagnosis in the family) and screened for stomach and small-bowel cancers with EGD beginning at age 30 to 35 years.
Define autopeep.
What are 3 ways you reduce autopeep on a paralyzed ventilated patient?
Unplug the ventilator, allowing the patient to exhale completely
Decrease RR (increases expiration time)
Increase I:E ratio (usually set 1:2, can go to 1:3 or 1:4)
Reduce tidal volume (less volume needed to exhale)
Increase external PEEP (decreases airway resistance by keeping airways open)
Define TI and TIIb Chronic Spontaneous Urticaria by what antibodies are driving the reaction and what type of "auto" they are
TI - Auto-allergic - IgE antibodies directed at self-antigens, stimulating mast cells.
Responds well to anti-IgE (omalizumab)
TIIb - Autoimmune - IgG/IgM antibodies directed at IgE receptor or IgE itself - activating mast cells and histamine release.
Responds better to cyclosporine
A 50-year-old man with a 5-year history of compensated MASH cirrhosis presents with 1 week of rapidly progressive abdominal distention and new right upper quadrant abdominal pain, which he describes as sharper and more persistent than his usual discomfort. He reports a 10-lb weight gain. He abstains from alcohol and reports no recent medication changes, fever, or gastrointestinal bleeding.
He notes that he was previously told he had “slightly low platelets” but was otherwise stable, and he was evaluated 2 months ago with normal liver chemistries and INR. On exam, he has new splenomegaly and more prominent abdominal wall veins compared with prior visits; mild tenderness is present over the right upper quadrant.
A diagnostic paracentesis is performed and reveals:
Neutrophils: 100 cells/mm³
Ascitic fluid albumin: 1.5 g/dL
Serum albumin: 4.0 g/dL
What is the most likely cause of his decompensation and the best treatment?
Acute portal vein thrombosis (formerly called Cauchois-Eppinger-Frugoni syndrome) causing an abrupt increase in portal pressure and new-onset ascites.
Why PVT is the cause
Abrupt onset (1 week) of ascites → suggests an acute process, not slow progression of cirrhosis
New RUQ abdominal pain → classic for acute PVT
Previously stable INR/LFTs → argues against intrinsic hepatic deterioration
New splenomegaly + more prominent abdominal wall veins → signs of suddenly worsened portal hypertension
Therapeutic anticoagulation
ASH recommends for all PVT
AGA recommends for <6 month hx, >50% occlusion vessel, or involves the main portal vein/mesenteric vessels - which appear to be the case here