A 72 YOF presents with worsening dyspnea and severe MR with planned repair of the valve leaflet pictured. Which valve leaflet will be repaired?
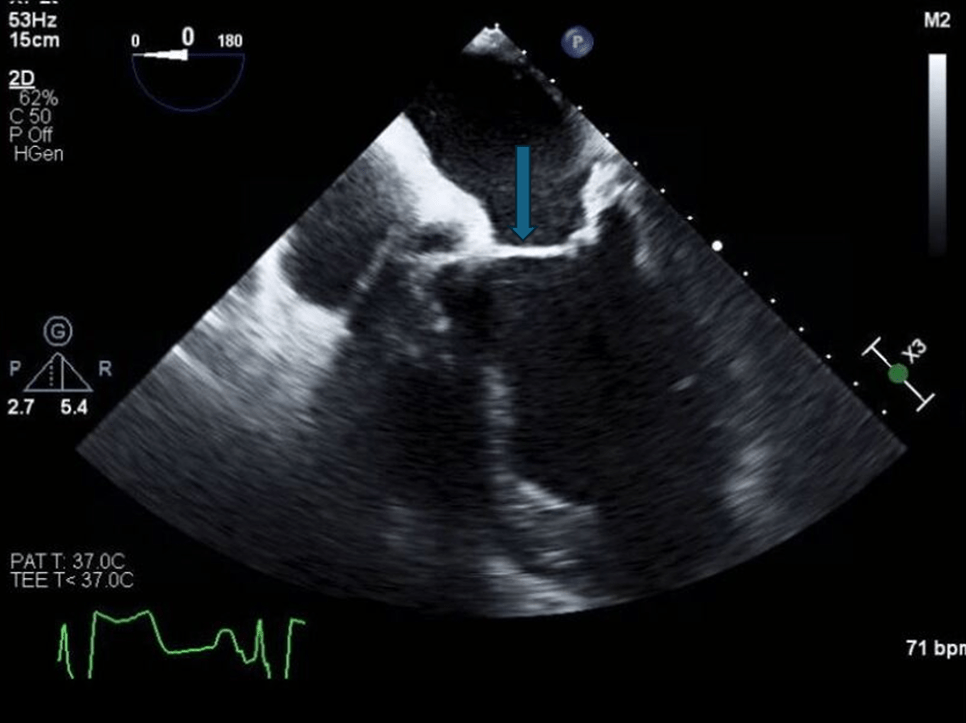
Anterior leaflet (A1/2)
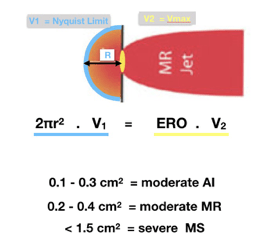
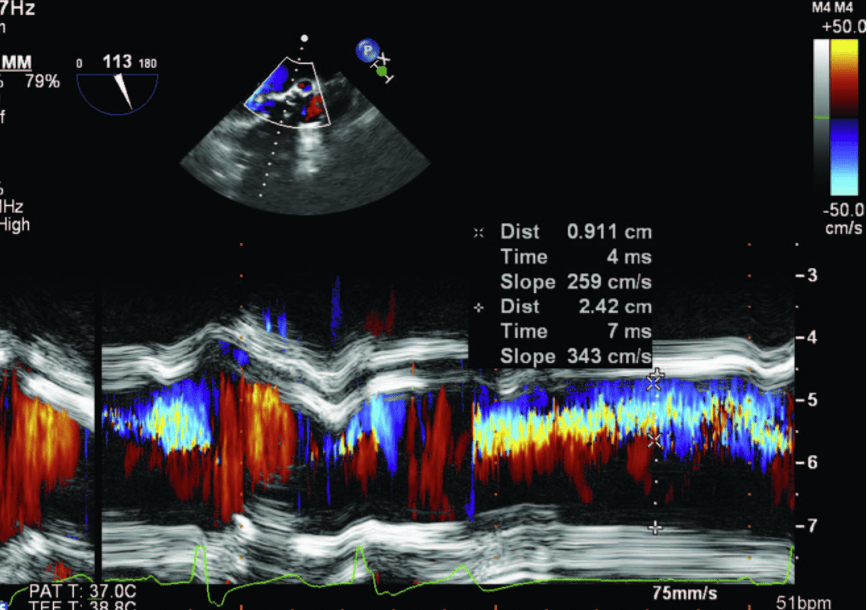
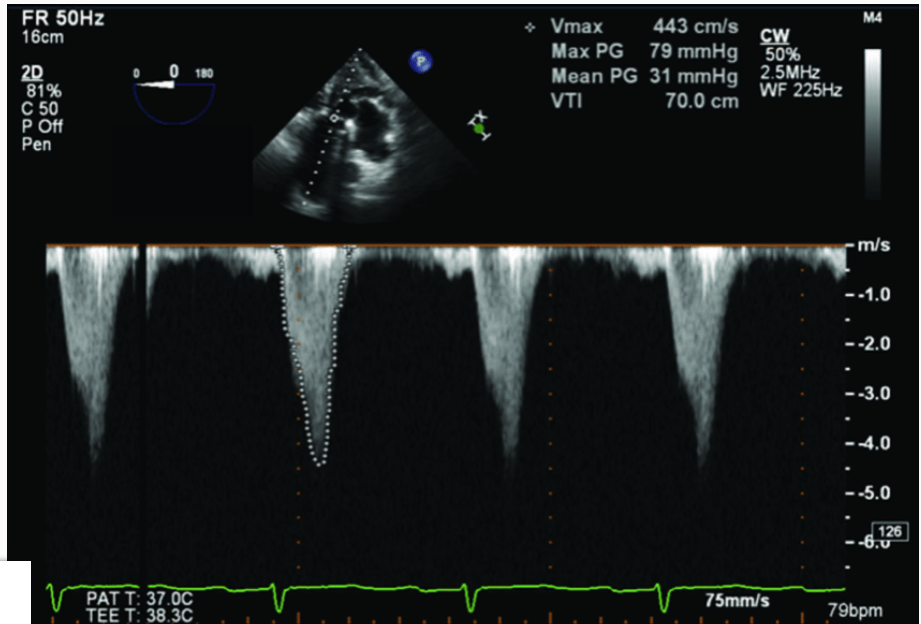
The following intraoperative spectral Doppler images are obtained in a 55 year old man undergoing an aortic valve replacement. What is the calculated aortic valve effective regurgitant orifice area in cm2?
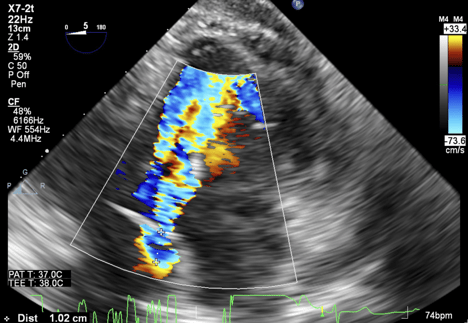
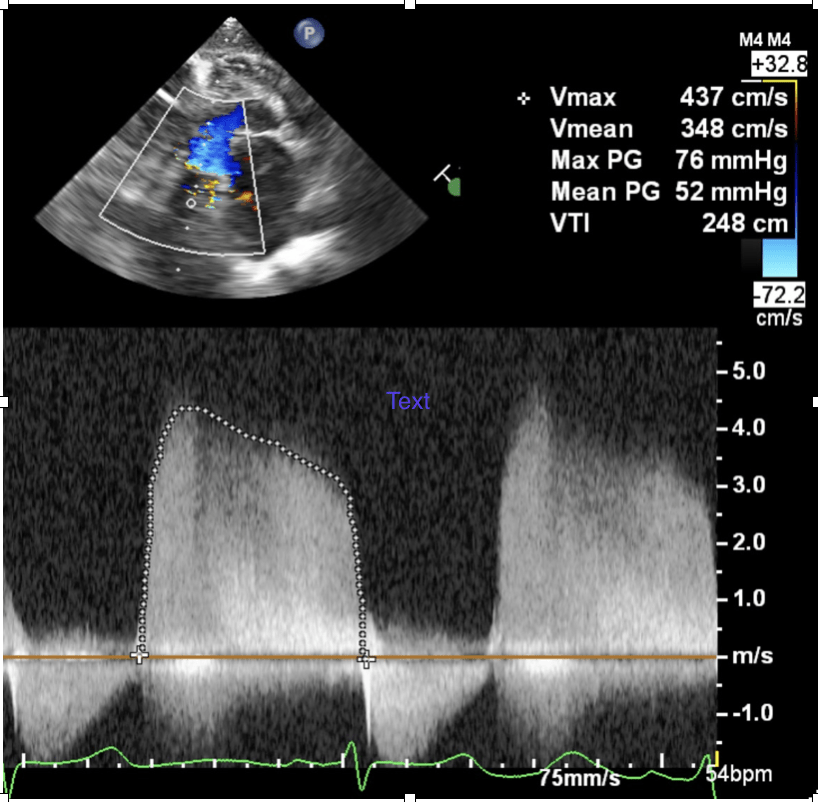
0.49 cm2
AI ERO = 2 * ∏ * PISA radius2 * (Aliasing velocity/Peak E-wave velocity)
= 2 * 3.14 * 1.022 * 33.4/437 = 0.49cm2
Answer B = 3.14 * 1.022 * 33.4/437 = 0.25cm2 (using π instead of 2π)
Answer C = 2 * 3.14 * 1.022 * 73.6/437 = 1.1cm2 (using wrong aliasing velocity)
Answer D = 2 * 3.14 * 1.022 * 33.4/348 = 0.62cm2 (using mean velocity instead of peak)
Rationale:
Instantaneous flow rate through the hemispheric surface area of flow convergence has to equal the flow rate through the narrowest orifice (the AI regurgitant orifice in this case). As flow accelerates as the flow path narrows, the peak velocity on continuous wave Doppler will be the flow rate at the orifice.
When interrogating blood flow velocity through a stenotic aortic valve, the angle formed between the true direction of blood flow and the direction of the ultrasound beam is 60 degrees. With respect to the true Doppler shift (calculated if the direction of blood flow and ultrasound beam were parallel), the calculated Doppler shift will be reduced by what percentage?
50% less than the true Doppler shift
W
The relationship between the calculated Doppler shift and the angle formed between the true direction of blood flow and the direction of the ultrasound beam is described by
cosθ
Therefore, if q = 60, then cos60=0.5cos60=0.5 or 50%.
What is the most common congenital heart defect?
Bicuspid aortic valve
A 57 YOM with metastatic prostate cancer undergoes drainage of a large pericardial effusion with a surgical approach. Post drainage, the patient's blood pressure drops from 110/70 to 75/30. TEE is negative for myocardial or aortic injury. What is the most likely diagnosis?
Decompression syndrome is a common cause of hypotension after surgical drainage of pericardial effusions. Often due to the rapid expansion of the right sided chambers as a well as rapid increase in ventricular filling.
In Phase 0 of the action potential of cardiac pacemaker cells, which ion undergoes rapid influx.
In 2022, Meng et. al showed Pre-anesthetic use of this medication preoperatively reduced the incidence of emergence agitation in patients undergoing VATS lobectomy/segmentectomy.
butorphanol
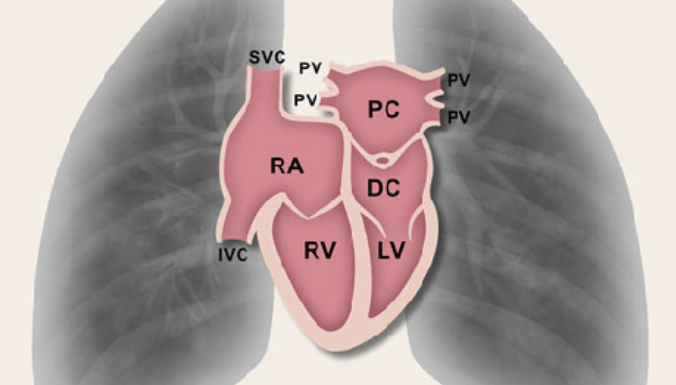
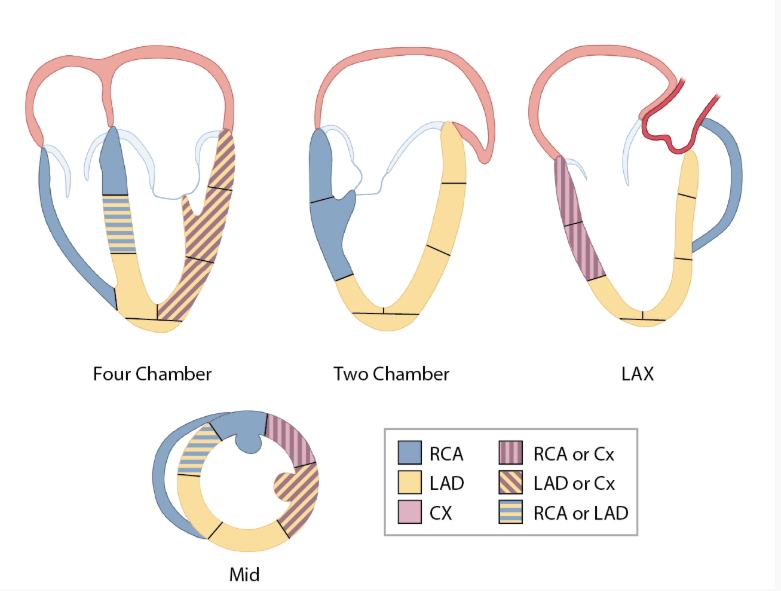
A 86 YOM with unknown PMHX is undergoing emergent ORIF of his lower extremity under general anesthesia. After induction the patient becomes hypotensive with ST changes, and then complete heart block. Coronary perfusion from which artery is most likely the culprit.
Right coronary artery: The AV nodal artery is derived from the RCA in 90% of patients, the other 10% of patients it is derived from the left circumflex.
Calculate the LV stroke volume from the following data:
Heart Rate: 64 BPM
LV end-diastolic dimension: 5.3 cm
LV end-systolic dimension: 3.8 cm
LV outflow tract diameter: 2.4 cm
LV outflow tract VTI: 15 cm
98 mL
Stroke volume (SV) is volume of blood ejected from the LV during systole. SV is calculated as the product of the VTI and cross-sectional area (CSA) at the point of interrogation and at the same point in the cardiac cycle. In the case SV across the LVOT in systole can be calculated as follows:
CSAlvot X VTIlvot = (pi*Radiuslvot)2 X VTIlvot = pi(2.4/2)^2 X 15 = 68 mL
You are interrogating a recently replaced aortic valve with transesophageal echocardiography. Due to the patient’s tachycardia, you are having a difficult time visualizing the valve and confirming that both leaflets are opening appropriately. You elect to increase the temporal resolution of your ultrasound image to improve your image quality. Which of the following changes will result in an increased temporal resolution of your ultrasound image?
Answer Options:
Decreasing the sector width
Increasing the sector depth
Increasing scan line density
Decreasing the pulse repetition frequency
Decreasing the sector width
Temporal resolution is the ability of the ultrasound system to display an object’s correct position in time during imaging. Temporal resolution is primarily determined by the ultrasound frame rate, or number of images per second that the ultrasound system is able to stitch together into video. Frame rate is measured in hertz (Hz) but described in number of images per second, and is analogous to pulse repetition frequency (number of ultrasound pulses per second). A higher frame rate or pulse repetition frequency, results in more images stitched together per second and is associated with improved temporal resolution.
When creating a frame, the ultrasound system generates a pulse of sound from a piezoelectric crystal element and then waits for the return of reflected sound waves that occur as the pulse encounters objects in its path. Each of these pulses comprises a scan line, and the ultrasound system must wait for each scan line to complete the pulse-listen period before generating a frame. Thus, factors which increase the time the ultrasound system must spend during this pulse-listen period subsequently decrease the frame rate and temporal resolution. Sector depth and sector width are directly correlated with pulse-wait time, as is scan line density. Thus, increases in any of these factors is associated with decreased frame rate and vice versa.
What 5 defects are associated with Cor Triatriatum Sinister?
Mitral stenosis, ASD, VSD, partial anomalous pulmonary venous return, total anomalous pulmonary venous return.
-Cor triatriatum sinister occurs when a membrane divides the left atrium
Bojanić, Katarina & Bursać, Danijel & Partl, Jasenka & Duić, Zeljko & Scavonetto, Federica & Weingarten, Toby & Sprung, Juraj. (2013). Isolated cor triatriatum sinistrum and pregnancy: Case report and review of the literature. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 60. 10.1007/s12630-013-9922-x.
A patient presents for TEE evaluation after being diagnosed with a carcinoid tumor. On evaluation moderate to severe mitral regurgitation with restricted leaflet motion is appreciated. What else should be evaluated given these specific findings?
Left sided carcinoid disease should also be screened for right to left shunt (ASD, PFO, or extracardiac shunt).
Which phase of the cardiac cycle contributes most to the largest volume of blood to the left ventricle during diastole
Early rapid filling
During a thoracoabdominal aortic aneurysm repair the surgeon reports there is sudden significant bleeding at the surgical site. The surgeon has to hold pressure near the anterior radicular vessels at the lower thoracic and upper lumbar levels. What would you expect to happen to the motor evoked potential monitoring.
Decreased amplitude and increased latency (Anterior spinal cord)
What proportion of the spinal cord does the anterior spinal artery supply
2/3
Calculate the cardiac output from the following data:
Heart Rate: 64 BPM
LV end-diastolic dimension: 5.3 cm
LV end-systolic dimension: 3.8 cm
LV outflow tract diameter: 2.4 cm
LV outflow tract VTI: 15 cm
4.4 L/min
CO is product of SV (From previous ?) and heart rate
CO=SV X HR = (68 mL X 64 BPM)/(1000(Conversion to L)
The interaction of ultrasound waves with tissue results in bioeffects, such as generation of heat and cavitation. Increasing which property of an ultrasound beam will most directly result in an increase in bioeffects?
Intensity
When an ultrasound wave strikes a biological surface, a small portion of that energy is reflected back to the ultrasound transducer and is processed into an image. However, the vast majority of that energy is absorbed by and interacts with the biological surface in other ways. These other interactions between ultrasound waves and biological tissues are defined as bioeffects. Bioeffects can be grouped as thermal and non-thermal. Thermal effects consist of elevations in temperature in the tissue being imaged. Non-thermal effects include radiation forces and cavitation. Radiation forces are the sheer stresses and streaming of fluids exerted by ultrasound waves, and cavitation is the interaction of sound waves with microscopic gas bubbles in tissues.
The most important determinant of bioeffects is ultrasound intensity, or ultrasound power per unit area. Alterations to pulse repetition period, wavelength and frequency have minimal to no influence on bioeffects.
A patient is undergoing aortic valve and root replacement. Retrograde cardioplegia is planned after initial arrest. On initial TEE imaging you notice a dilated coronary sinus. What pathology should be ruled out?
Persistent left SVC. It can be diagnosed by agitated saline injection into the LUE resulting in bubbles in the coronary sinus prior to the right atrium.
This repair-oriented classification system is used to assess aortic regurgitation.
El Khoury
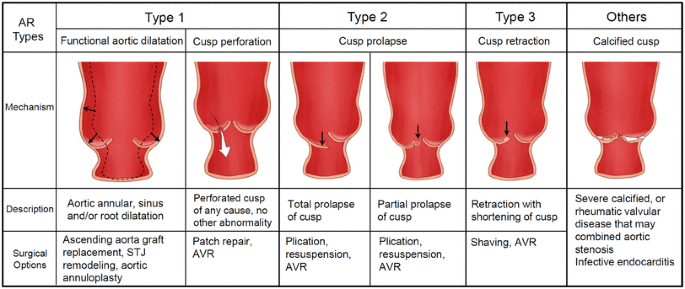
Koo, H.J., Kang, JW., Kim, J.A. et al. Functional classification of aortic regurgitation using cardiac computed tomography: comparison with surgical inspection. Int J Cardiovasc Imaging 34, 1295–1303 (2018). https://doi.org/10.1007/s10554-018-1341-1

Which adrenergic receptors are involved in sympathetic cardiac innervation
A1, B1, B2
Which quadrants of the body drain into the thoracic duct?
left upper body and bilateral lower body (Right upper body drains into right lymphatic duct)
You are consulted for a 68 YOM undergoing emergent appendectomy with ST changes on telemetry. TEE is notable for hypokinesis of the free wall of the right ventricle. Which coronary artery supplies this region?
Right (acute) Marginal artery (Branch of the RCA)
An 82 YOM with prior ischemic heart disease presents for evaluation of his aortic valve. Echocardiography demonstrates a heavily calcified aortic valve, an EF of 24%, and regional wall motion abnormalities in the anterior wall, inferior wall, and apex. The LVOT diameter measures 2.4 cm. The data below was calculated from a dobutamine stress test. Calculate the baseline (Cm2) aortic valve area
EF Baseline: 24%
EF dobutamine: 38%
LVOT velocity (m/s) Baseline: 0.7
LVOT velocity (m/s) Dobutamine: 1.2
Aortic maximum velocity (m/s) Baseline: 3.6
Aortic maximum velocity (m/s) Dobutamine: 4.4
Mean aortic gradient (mm Hg) Baseline: 32
Mean aortic gradient (mm Hg) Dobutamine: 38
0.9 cm2
Baseline AVA = (CSALVOT X VLVOT)/Vav
What are the 5 essential functions of an ultrasound receiver:
There are 5 essential functions of an ultrasound receiver: amplification, compensation, compression, demodulation and rejection. Amplification consists of enlarging the returning ultrasound signal which is significantly smaller than the emitted signal. Amplification is also referred to as receiver gain and can be altered by the sonographer to alter the brightness of the ultrasound image. Ultrasound waves and subsequent reflections weaken as they travel further from the source. Compensation refers to the enhancement of returning signals from deeper structures so that the image is uniformly bright from top to bottom. This is also adjustable by the sonographer via time-gain compensation slide bars. Compression reduces the total range of signals to keep the signal levels within the accuracy range of the system and to keep the gray scale content within the range of detection by the human eye. Demodulation changes the shape of the electrical signal so it is recognizable by changing all negative voltages to positive signals and smoothing out the rough edges. Lastly, rejection ignores low level signals and background noise.
Transmission is not an essential function of an ultrasound receiver.
What are the three main types of Atriventricular septal defects (AVSDs)?
Partial AVSD – an ostium primum ASD, cleft mitral valve and two separate atrioventricular valves
Transitional AVSD – ostium primum ASD, small VSD and two distinct atrioventricular valves
Complete AVSD – an ostium primum ASD, inlet-type VSD and a common atrioventricular valve (the most common type).
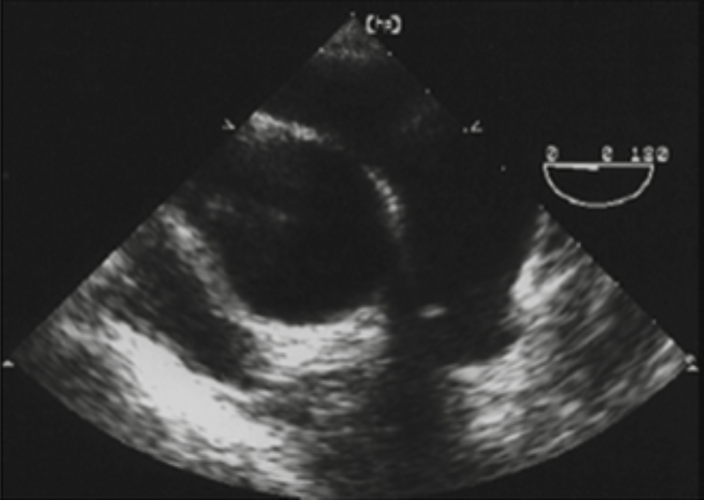
45 year old female presents for mitral valve replacement. Post induction the following image is obtained on TEE. What is the most probably cause of her mitral valve disease?
a. impaired production of connective tissue
b. calcification of the mitral valve commissures
c. myxoid infiltration
d. Aschoff nodules
"Billowing" of the mitral leaflets due to excess leaflet tissue characteristic of myxomatous mitral valve disease. Myxomatous degeneration refers to a pathological weakening of connective tissue characterized by myxoid infiltration.
At what temperature is the cerebral metabolic rate reduced by approximately 70%
26oC. There is a 6-7% reduction in cerebral metabolic rate per degree decrease in temp.
A patient is undergoing open thoracoabdominal aneurysm repair under left heart bypass. 6 minutes after initiating left heart bypass, the cerebral oximetry readings decrease by 30%. What intervention would be most appropriate immediately?
Decrease bypass flow
Name the cardiac veins that commonly run with the following coronary arteries:
RCA:
LAD:
PDA:
RCA: Anterior cardiac vein
LAD: Great cardiac vein
PDA: Middle cardiac vein

A patient has a peak velocity at the aortic valve of 3 m/s. What is the patient’s peak pressure gradient?
36 (4V2) AKA simplified bernoullie equation
What is the most common associated defect seen with coarctation of the aorta?
Bicuspid aortic valve
Coarctation of the aorta accounts for 8% of all cases of congenital heart disease. The anatomic lesion most commonly found is a discrete ridge of localized medial thickening, infolding of the media, and superimposed neointimal tissue that narrows the aortic segment just below the left subclavian artery. Associated defects include:
Bicuspid aortic valve (80-85%)
PDA
VSDs
Aortic stenosis
Subaortic stenosis
Turner Syndrome
A 76 YOM presents for aortic valve replacement. A color M-mode was obtained. Which mitral valve leaflet is the is the regurgitant jet oriented towards.
The AR is oriented toward the anterior leaflet of the mitral valve.
Compared to pressure monitoring at the proximal aorta, how would the systolic peak and dicrotic notch change when measured at the radial artery
Higher systolic peak and blunted dicrotic notch
Compared to the proximal aorta, arterial waveforms measured at more distal sites have higher systolic peak, steeper systolic upstroke, lower diastolic peak, blunted dicrotic notch, delayed dicrotic notch, and slightly lower MAP.
What 3 techniques can be used during thoracic aortic aneurysm stenting to help position the stent correctly and avoid migration.
Induced hypotension (reduce shear fear)
Transient asystole (Often with adenosine)
Rapid ventricular pacing (>180, will cease LV ejection)
The AV node is supplied by what coronary artery in the majority of the population
Right coronary:
The blood supply to the AV node is supplied by the right coronary artery in approximately 80% of the population. The blood supply to the AV node is supplied by the left circumflex artery in approximately 20% of the population.
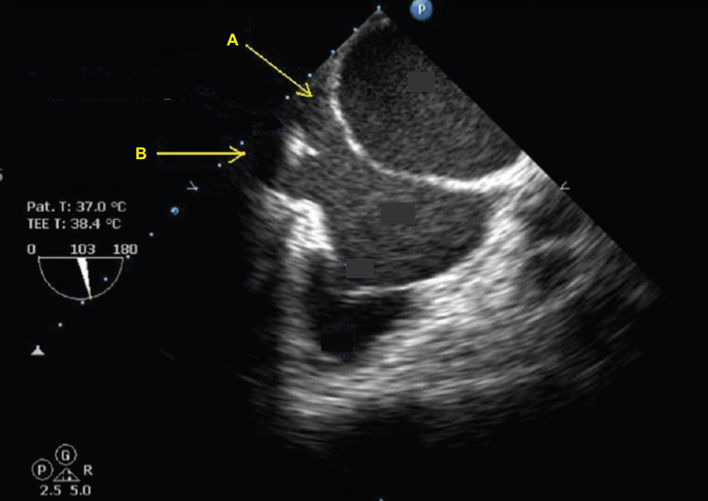
The following image is a four-chamber view zoomed on the mitral valve during diastole. Which velocity is greater, A or B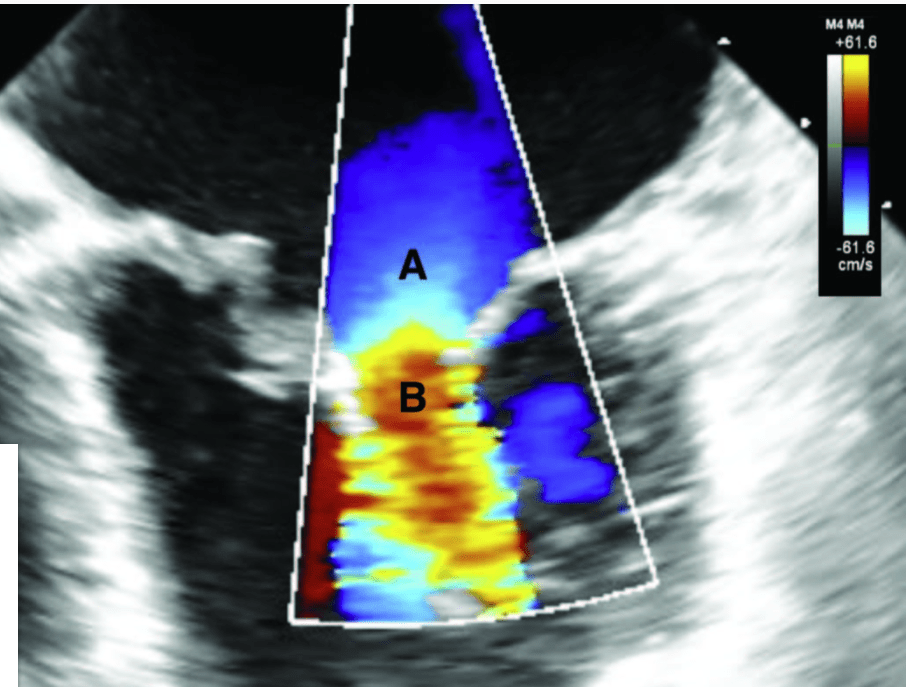
Velocity at B is greater than A
In this view blood flow is moving from the left atrium to the left ventricle. Aliasing can be appreciated at point B, where despite the flow going away from the probe, it is represented as going toward the probe (red). This is due to the fact that flow acceleration occurred and the velocity is exceeding the nyquist limit.
How are axial resolution and spatial pulse length related?
½ * spatial pulse length
Wolff-Parkinson-White syndrome or other arrhythmias are seen in 10-15% of patients born with this defect.
Ebstein's anomaly
Ebstein’s anomaly is a rare defect, accounting for less than 1% of all congenital heart defects, but constitutes 40% of the congenital malformations of the tricuspid valve. Anatomical findings in this patients include:
Downward displacement of the septal and posterior leaflets of the tricuspid valve into the right ventricle.
Large and redundant anterior leaflet, often described as “sail-like”. It is typically not displaced downward, unlike the other two leaflets.
Arterialization of the portion of right ventricle that is now part of the right atrium. The remaining RV is usually hypoplastic and functionally impaired.
Regurgitant tricuspid valve with multiple eccentric jets.
Interatrial communication such as ASD or PFO in 80% of patients.
Marked RV enlargement leads to arrhythmia in 10-15% of patients. WPW is also common in this patients.
A 65 YOM is undergoing hip pinning and you are called to the OR for assistance with rescue TEE after the patient has become hypotensive post-induction. What valvulopathy is most likely seen in this patient.
Severe TR. This video shows a transgastric short-axis view with a D-shaped LV at end diastole. This flattening of the interventricular septum at end diastole is typical of right ventricular volume overload, which commonly results in severe TR.
Which phase of the EKG corresponds to mitral valve closure?
R wave
The closing of the mitral valve corresponds to the electrical R wave of the QRS complex.
In a patient under deep hypothermic circulatory arrest, is air embolus more likely with retrograde cerebral perfusion or anterograde cerebral perfusion?
Retrograde
Which papillary muscle is most prone to rupture secondary to ischemia
The posteromedial papillary muscle
In the setting of ischemia and acute MR there should be a high suspicion for papillary muscle rupture. The posteromedial papillary muscle receives a single blood supply from the right coronary artery in two-thirds of patients. It is more prone to infarct than the anterolateral papillary muscle that receives dual blood supply from the LAD and left CX.
WHat is the pressure half-time in ms when the mitral valve has an area of 2 cm2
110 ms
The pressure half-time is a measurement of mitral stenosis severity. The decline of velocity of diastolic trasnmitral blood flow is inversely proportional to mitral valve area, which is derived using the formula:
MV area (CM^2) = 200/(PressureHalfTime(MS)
Which of the following parameters is determined by the ultrasound source and the medium through which the sound travels?
-period
-wavelength
-Frequency
-Amplitude
-Power
-Velocity
-Intensity
Wavelength
A 65 YOM presents with severe aortic regurgitation. The TEE is shown below. In this patient replacement of the aortic root should be considered at what diameter.
4.5 cm
This shows a bicuspid aortic valve. This condition is present in up to 2% of the general population. During aortic valve surgery for severe regurgitation or stenosis, it has been suggested that aortic root replacement should also be performed in patients with bicuspid aortic valves int eh ascending aorta is larger than 4.5 cm in diameter.
A patient with left-dominant coronary circulation has the following flow pattern in the RCA. What pathology is most likely present?
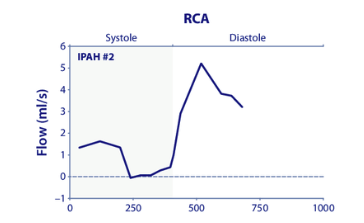
Right coronary artery flow impairment in patients with pulmonary hypertension - Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/Representative-examples-of-the-right-coronary-artery-and-left-anterior-descending-flow_fig11_5782087 [accessed 30 Apr 2025]
Chronic pulmonary artery hypertension (RV hypertyrophy)
A sixty-three-year-old female patient presents for a three-vessel coronary artery bypass graft. A comprehensive intraoperative transesophageal echocardiography study is performed and the following recommended view is obtained. Identify the correct view.
The midesophageal ascending aorta short axis view
A patient ha a mitral inflow deceleration time of 800 ms, What is the pressure half time in milliseconds?
232 ms
Pressure half time = 0.29 X Decel time
Which of the following statements is true regarding ultrasound?
A. Ultrasound waves have a frequency greater than 0.02 MHz
B. Imaging transducers have frequencies of 20 to 30 MHz
C.) Frequency is directly proportional to wavelength
D.) Frequency is determined by the medium through
A:
Ultrasound waves have frequencies greater than 0.02 MHz (20,000 Hz). Imaging transducers usually have a range of 3.5 to 12 MHz. Frequency is inversely proportional to wavelength.
A 35 YOM presents with exertional dyspnea. TEE is notable for the following images. What is the diagnosis?
Subaortic stenosis is usually secondary to an abnormal fibromuscular ridge that is found in LVOT. This results in LV outflow obstruction with similar hemodynamic effects to aortic valve stenosis and HOCM. Surgical repair involves excision of the membrane or ridge, septal myomectomy, and aortic valve replacement if severe aortic regurgitation is present. On TEE, you will find the appearance of flow acceleration with turbulent flow via color flow doppler proximal to the aortic valve. You’ll also find high frequency oscillation or “fluttering” of the aortic valve leaflets on M-mode. This is a classic finding of subaortic stenosis.
A 65 year old presents for emergent CABG. TEE is performed post induction showing the following image. What pathology should be identified?
LV thrombus, a common complication of acute MI. LV thrombi occurring as a result of acute MI are usually classified as "Mural" due to their usual proximity or attachment to the ventricular wall as seen in this video.
Which of the following is NOT a cause of regional wall motion abnormalities
a.) Coronary air embolus
b.) Right bundle branch block
c.) Ventricular pacing
d.) Aortic cross-clamping
e,) Myocardial ischemia
B: Right bundle branch block
The following midesophageal TEE image was recorded during a transesophageal echocardiography study. The labels that best represent the letters are the following:
A = inferior vena cava; B = coronary sinus
You are evaluating a patient for aortic valve replacement. The following measurements are obtained. What is the peak gradient across the aortic valve:
LVOT diameter: 2.1 cm
LVOT VTI: 13 cm
LVOT peak velocity: 0.5 m/s
Aortic valve peak velocity: 4.5 m/s
Aortic valve VTI: 22 cm
81 mmHg
Modified Bernoulli equation:
P=4(Peak aortic valve velocity)2
=5(4.5)2
=81 mmHg
Which of the following tissues has the lowest speed of propagation for US waves
A.) liver
B.) blood
c.) Bone
d.) Soft tissue
e.) Lung
E
The lung has the lowest speed for conduction of sound (500 m/s). This is because lung fields primarily represent air. Recall that the speed of sound is slowest and air and becomes progressively faster in stiffer materials.
A patient underwent atrial switch repair (Mustard procedure) as an infant for transposition of great arteries. Patient presented to his cardiologist at age 35 with progressively worsening dyspnea. A TEE exam would reveal this most likely diagnosis:
RV dysfunction
In d-TGA, the deoxygenated systemic venous return is directed from the right ventricle (RV) into the aorta while the oxygenated pulmonary venous return flows back into the pulmonary system via the left atrium and ventricle, thus creating two parallel circuits. In atrial switch repair (Mustard procedure) the atrial baffle redirects systemic venous return to the left heart, which then flowed into the pulmonary system, while the pulmonary venous return is redirected to the right heart, which ejects the oxygenated blood systemically. The atrial switch in effect makes the morphologic RV into the systemic ventricle. By the late 1980s, this procedure was replaced by the arterial switch technique because it allowed for the reestablishment of ventriculoarterial concordance.
With ventriculoarterial discordance, the morphologic RV is unable to function long-term as the systemic pump. In a longitudinal, single-center study of Mustard procedure patients, RV dysfunction was observed in all but one patient, with 23% being diagnosed with heart failure (Dobson). The severity of RV dysfunction will likely worsen as the patients continue to age.
A patient is undergoing mitral valve replacement. Pre-bypass TEE is shown. What 2 pathologies are noted?
A 75-year-old man with a history of an esophageal stricture and dysphagia presents for a coronary artery bypass graft procedure. The following epicardiac echocardiographic image was recorded. Identify the structures labelled A, B and C.
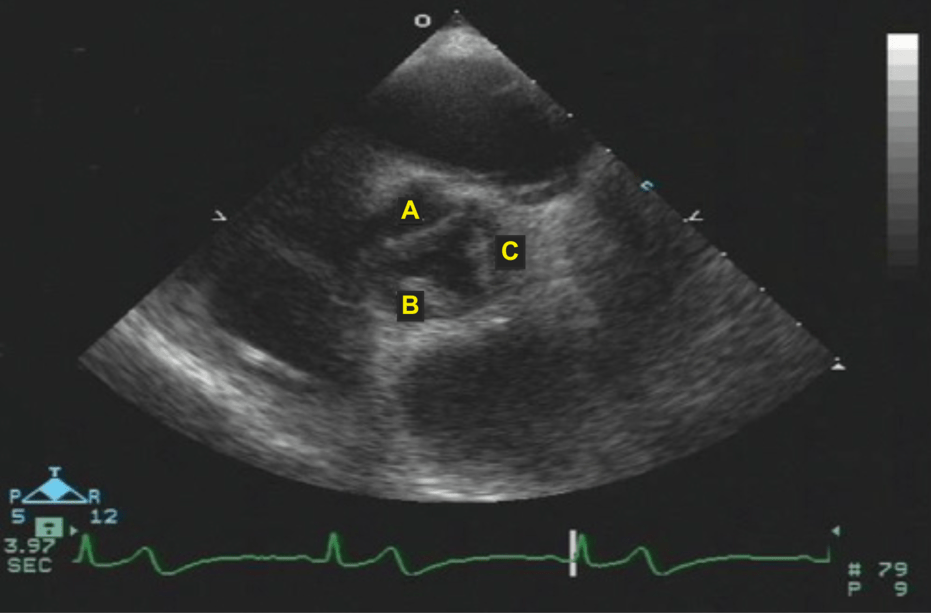
A = right coronary cusp; B = left coronary cusp; C = non coronary cusp
To obtain a correct epicardial aortic valve short-axis view, the ultrasound transducer is placed on the aortic root above the aortic valve (AV) annulus, with the ultrasound beam directed towards the AV in a short-axis (SAX) orientation. Appropriate transducer alignment requires up to 30° of clockwise rotation with the orientation marker (indentation) on the transducer directed toward the patient’s left.
When the orientation marker (indentation) on the transducer is pointed towards the patient’s left, the right coronary cusp (R) will be at the top of the monitor screen, the left coronary cusp (L) is on the bottom left, and the noncoronary cusp (N) is on the right side of the screen adjacent to the interatrial septum, as indicated in the figure below.
A patient undergoes TEE and is found to have a TR jet with a peak velocity of 2.2 m/s, with a tricuspid annular plane systolic excursion of 18 mm. He has a CVP of 10 mmHg, what is his pulmonary artery systolic pressure
29.36 mmHg
PASP= CVP + (RV to RA pressure gradient)
TR gradient = 4(TR peak velocity)2
=4(2.2)2 = 19.36 mmHg
PASP = 10+19.36 = 39.36 mmHg
Which of the following increases when switching from a 3.5 MHz to a 7 MHz transducer?
a.) Axial Resolution
b.) Duty factor
c.) Frame rate
d.) Speed of sound
A. Axial resolution
-Axial resolution is related to the frequency of the transducer, the higher the frequency the higher the resolution
What is the most common type of ventricular septal defect?
Membranous, peri-, para-, infracristal, subaortic
On TEE of the descending thoracic aorta a protruding 6 mm atheroma is found. What is the severity of aorta atheroma?
Class 4
"Montgomery's" Classification of aortic atheromas is as follows
1: normal or mild thickening of intima
2: extensive intimal thickening
3: Atheroma <5 mm
4: Atheroma>5 mm
5: Mobile lesion
A 73 year old man with a history of sick sinus syndrome undergoes a laser lead extraction for infected pacemaker leads. A post extraction TEE study is performed to rule out suspected pericardial effusion. What is the correct diagnosis for the following finding.
Chiari Network
The Eustachian valve is a derivative of the embryologic right venous valve (valve of the sinus venosus), which directs oxygenated blood from the IVC through the foramen ovale and into the left atrium. In adults, it is visualized at the junction of the IVC and RA and is present in 57% of patients. The Eustacian valve does not cross the tricuspid valve. In stroke patients, those who have experienced a paradoxical embolism appear to be twice as likely to have a Eustacian valve than those who don’t. The Eustacian valve has also been implicated as a site for endocarditis.
Chiari network are large fenestrated remnants of the embryonic right venous valve (just like the Eustachian valve). Chiari networks are less common (only 2% of adults), but are highly associated with PFO (relative risk 2.96 based on an analysis of 1436 patients) and also atrial septal aneurysms.
The Crista Terminalis is a muscular ridge whose embryologic origin is from the junction between the sinus venosus and the atrium of the developing embryo. During development, portions of the sinus venosus (the right horn and transverse portions) are incorporated into the adult right atrium. In the adult, the Crista Terminalis resides at the junction of the SVC and the RA, and is directed towards the IVC. It is sometimes mistaken for a mass lesion.”
A patient is undergoing mitral valve repair. He has an MR jet with a peak velocity of 6 m/s. The rest of his valves are normal. He is stable with an arterial blood pressure of 143/76. Heart rate 80 beats/min, CVP 10 mm Hg, ETCO2 36 mm HG. What is his left atrial pressure during systole?
6 mmHg
The atrial pressure during systole in this patient is equal to the systolic left ventricular pressure minus the pressure gradient across the mitral valve during systole. The systolic left ventricular pressure is equal to the systolic arterial pressure in the absence of aortic valve abnormalities.
LAP = systolic arterial pressure - (4 X MRvelocity2)
=150-144
= 6 mmHg
hich of the following happens when the gain is increased in an US system:
a.) Increase in the signal to noise ratio
b.) Increase in the amplification of the returning signals
c.) Decrease in the brightness of the image
d.) decrease in the quality factor
e.) Decrease in attenuation
f.) Increase in the energy of the waves emitted
b.) Gain amplifies the returning signal. Gain does not change signal to noise ratio, and it does not vary the energy of the waves that are emitted from the transducer. Gain does not change attenuation because attenuation occurs before the ultrasound waves reach the transducer.
This is the only VSD located above the crista supraventricularis
Type 1 (Outlet, subpulmonic, subvalvular, supracristal, conal, intraconal, doubly committed subarterial)
This CWD profile was obtained in the deep transgastric view. The peak velocity is 4 m/s. What type of flow/pathology is most likely?
Dynamic LVOT obstruction
-Dagger shaped doppler profile
A 44 y/o female presents for VA-ECMO due to cardiogenic shock. The surgeon asks for echo guidance for placement of the venous cannula. The cannula is placed where the * is in the image below. Identify the structure with the *.
This is an image of the bicaval view. In this view, you should see the inferior vena cava (IVC), superior vena cava (SVC), left atrium (LA) and right atrium (RA). See the image below.
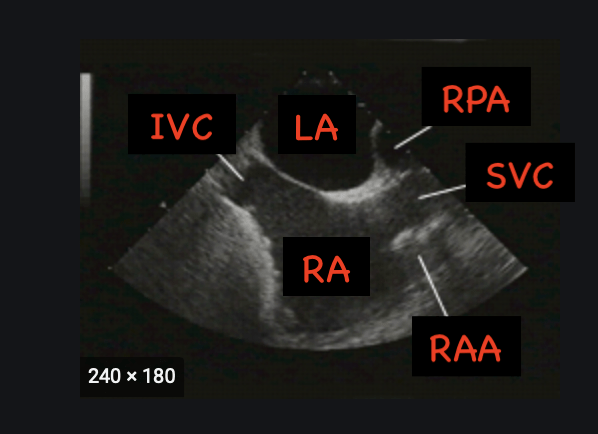
Often times, you'll also be able to visualize the right atrial appendage (RAA).
When providing guidance for the surgeon during placement of a venous cannula it is important for you to visualize the cannula going into the IVC, RA or SVC (whichever the surgeon and procedure calls for.). Placement of the venous cannula anywhere else (hepatic vein, across tricuspid valve, abutting the interatrial septum, RAA) is very dangerous.
What effect does backing material have on ringing of piezoelectric crystals
Backing material reduces the ringing of piezoelectric crystals, rendering them unable to vibrate freely. Consequently, the sound pulses become shorter, enhancing axial resolution. Short pulse duration, a click, has multiple frequencies rather than multiple resonant frequencies.
What are the 2 surgical options to augment pulmonary blood flow during a Stage I Norwood procedure?
Sano shunt (RV to PA conduit) or BT shunt (SCA to PA)
